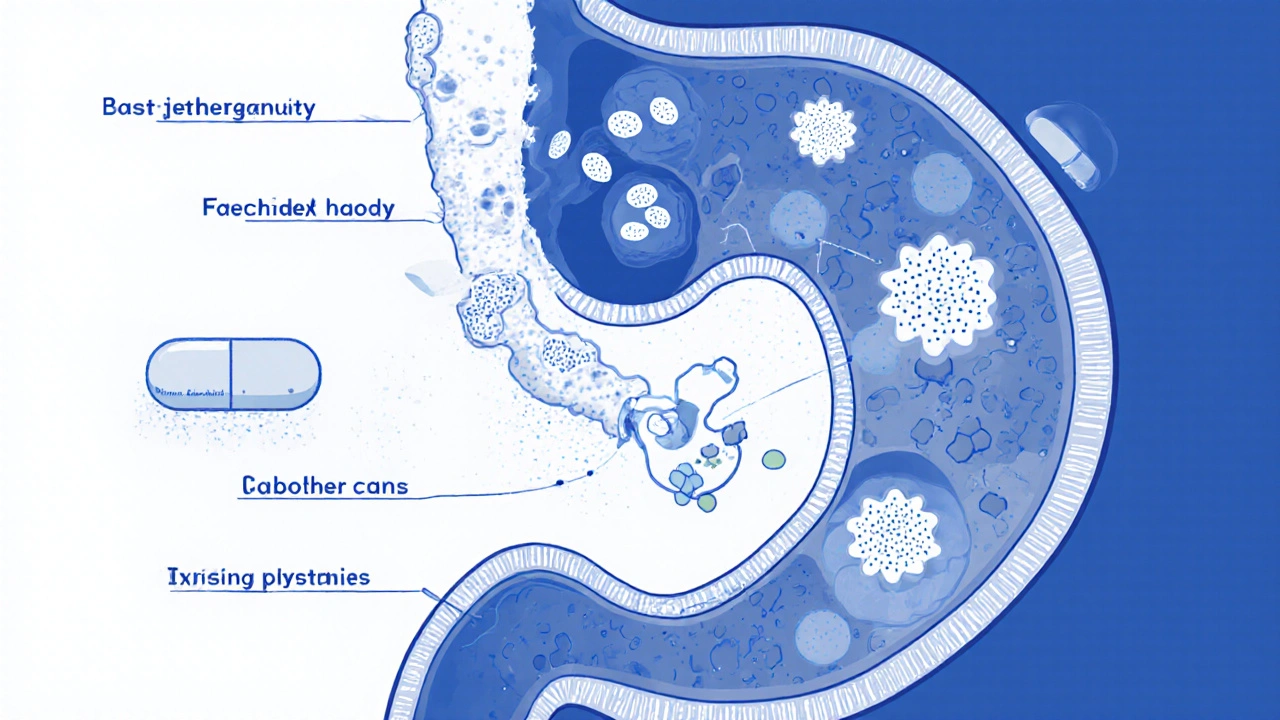
When a yeast infection esophagus, a fungal infection caused by Candida species that spreads from the mouth into the esophagus. Also known as esophageal candidiasis, it doesn’t just cause discomfort—it can make swallowing painful or even impossible. This isn’t just a bad case of oral thrush. While oral thrush stays in the mouth, a yeast infection esophagus moves deeper, affecting the tube that connects your throat to your stomach. It’s most common in people with weakened immune systems—like those with HIV, diabetes, or people on long-term steroids or antibiotics—but it can happen to anyone.
It’s not just about feeling a burning sensation when you eat. People with this condition often describe food sticking in their chest, a constant sore throat, or even nausea after meals. If you’ve had oral thrush and it didn’t clear up with mouth rinses, that’s a red flag. The fungus can climb down. antifungal treatment, medications like fluconazole or nystatin that target Candida overgrowth is the standard fix. But not all antifungals work the same. Fluconazole is usually the first choice because it’s taken as a pill and reaches the esophagus directly. Nystatin works only if you can swallow it properly—some people spit it out, which defeats the purpose. And if you’ve tried one antifungal and it didn’t help? You might be dealing with a resistant strain. That’s when doctors move to stronger options like itraconazole or even intravenous drugs.
What makes this worse is that people often ignore early signs. They think it’s heartburn, a cold, or stress. But if your symptoms last more than a week, especially with a history of immune issues, don’t wait. Left untreated, the infection can spread to other organs. It’s also linked to other conditions. For example, if you have chronic acid reflux, the damaged lining of your esophagus makes it easier for yeast to take hold. That’s why managing reflux is part of recovery. And if you’re on inhaled steroids for asthma? Rinsing your mouth after each use isn’t just a suggestion—it’s a must to prevent yeast from moving down.
You might be surprised how often this gets misdiagnosed. Some patients are told they have GERD for months, when the real issue is fungal. A simple endoscopy with a biopsy can confirm it. No guessing. No waiting. And once you know it’s yeast, treatment is usually fast and effective. But recurrence is common if the root cause isn’t addressed. So if you’ve had this twice, it’s time to look at your overall health: Are you on antibiotics too often? Do you have undiagnosed diabetes? Are you smoking or drinking too much alcohol? These aren’t just lifestyle choices—they’re risk factors that keep the yeast coming back.
Below, you’ll find real-world guides on how different antifungals compare, what to avoid mixing with them, and how to spot when a simple infection turns serious. These aren’t theoretical articles—they’re written by people who’ve been through it, and the doctors who treat it. Whether you’re dealing with this now or helping someone who is, the information here cuts through the noise and gives you what actually works.
Fluconazole is the standard treatment for candida esophagitis, especially in immunocompromised patients. Learn how it works, proper dosing, what to expect, and how to prevent recurrence.