When swallowing becomes painful, food feels stuck, or you notice a persistent white coating in your throat, it might not just be a cold. For people with weakened immune systems-like those with HIV, cancer, or on long-term steroids-these signs could point to candida esophagitis, a fungal infection of the esophagus caused by Candida yeast. Left untreated, it can lead to serious complications. Fluconazole is the most common and effective treatment, but knowing how it works, when to use it, and how to avoid recurrence is just as important as taking the pill.
What Is Candida Esophagitis?
Candida esophagitis happens when the Candida fungus, usually harmless and present in small amounts in your mouth and gut, overgrows and spreads into the esophagus. This isn’t something that happens to healthy people often. It’s mostly seen in those with weakened immunity. People with uncontrolled diabetes, those taking antibiotics for long periods, or anyone on chemotherapy or corticosteroids are at higher risk.
The infection causes inflammation and sometimes ulcers in the esophagus. Symptoms aren’t always obvious at first, but they get worse if ignored. You might feel like food is sticking in your chest, especially when eating bread or meat. Swallowing hurts-sometimes so badly that you avoid eating altogether. Some people report a metallic taste or even nausea. In severe cases, you might vomit blood or lose weight without trying.
How Fluconazole Works Against Candida
Fluconazole is an antifungal drug in the azole class. It doesn’t kill Candida outright. Instead, it blocks the fungus from building a strong cell membrane. Without that protective layer, the yeast cells leak and die. It’s absorbed well by the body and travels through the bloodstream to reach the esophagus, even though it’s not on the surface like oral thrush.
What makes fluconazole ideal for this infection? It’s taken as a pill, works systemically, and has fewer side effects than older antifungals like amphotericin B. Studies show that a single 200 mg dose on day one, followed by 100 mg daily for 14 to 21 days, clears the infection in over 90% of patients with HIV-associated esophagitis. Even in non-HIV patients, success rates stay above 85% when taken as directed.
It’s not just effective-it’s convenient. Unlike some antifungals that require IV drips or multiple daily doses, fluconazole is usually just one pill a day. Most people start feeling better within 3 to 5 days. But stopping early is a mistake. Even if symptoms fade, the fungus might still be hiding. That’s why completing the full course matters.
Who Should Take Fluconazole for Esophagitis?
Not everyone with a sore throat needs fluconazole. Doctors don’t just prescribe it based on symptoms. Diagnosis usually requires an endoscopy-a thin camera inserted down the throat-to see the white plaques and sometimes take a biopsy. That’s because other conditions like acid reflux, viral infections, or even esophageal cancer can mimic candida esophagitis.
Fluconazole is recommended when:
- Endoscopy confirms Candida infection in the esophagus
- You’re immunocompromised (HIV with CD4 count under 200, transplant recipients, cancer patients)
- You’ve had recurrent oral thrush and now have swallowing issues
- Other treatments like nystatin swish-and-swallow didn’t work
For healthy people with mild symptoms, doctors may try lifestyle changes or topical treatments first. But if symptoms persist beyond a week or worsen, fluconazole becomes the go-to option.
Dosage and How to Take It
Standard treatment for candida esophagitis is 200 mg on the first day, then 100 mg once daily for at least 14 days. In severe cases, or if you’re not responding, the dose may be raised to 400 mg daily. Treatment usually lasts 2 to 3 weeks, even if you feel better sooner.
Take it with or without food-it doesn’t matter. But avoid taking it with antacids or H2 blockers like ranitidine within two hours, because they can reduce absorption. If you’re on other medications, check with your doctor. Fluconazole can interact with blood thinners, diabetes pills, and some seizure medications.
Side effects are usually mild: nausea, headache, or stomach upset. Serious reactions like liver damage or allergic rashes are rare but possible. If you develop yellow skin, dark urine, or a severe rash, stop taking it and call your doctor immediately.
What Happens If Fluconazole Doesn’t Work?
Most people respond well, but about 5-10% don’t. This is called fluconazole-resistant candida esophagitis. It’s more common in people who’ve taken azole antifungals repeatedly over time-like those with chronic thrush or long-term HIV treatment.
If fluconazole fails, your doctor will likely switch you to another antifungal:
- Echinocandins (like caspofungin): given by IV, used in hospitals
- Amphotericin B: older, more toxic, but still effective
- Itraconazole or voriconazole: other oral azoles, sometimes used if fluconazole fails
Resistance isn’t random. It’s often linked to long-term, low-dose antifungal use. That’s why doctors avoid prescribing fluconazole as a daily preventive unless absolutely necessary.
How to Prevent Recurrence
Once the infection clears, the biggest fear is it coming back. Prevention isn’t just about pills-it’s about managing the root cause.
If you have HIV, keeping your viral load low and your CD4 count above 200 is the best defense. For diabetics, controlling blood sugar is critical-high glucose feeds yeast. Avoid unnecessary antibiotics. They wipe out good bacteria that keep Candida in check.
For people prone to recurrent infections, doctors may recommend maintenance therapy: 100-200 mg of fluconazole once a week. But this isn’t for everyone. Long-term use increases resistance risk. It’s usually reserved for those with frequent relapses (three or more episodes a year).
Lifestyle changes help too:
- Limit sugary foods and refined carbs
- Don’t use mouthwashes with alcohol-they dry out the mouth
- Brush and floss daily, and clean dentures thoroughly if you wear them
- Stay hydrated to keep saliva flowing-saliva naturally fights yeast
When to See a Doctor
Don’t wait for symptoms to get worse. See a doctor if:
- Swallowing pain lasts more than 5 days
- You’re losing weight without trying
- You’ve had recent antibiotic use or immune-suppressing treatment
- You have white patches in your mouth that spread to your chest
Early diagnosis means faster relief and fewer complications. If you’re immunocompromised and develop new swallowing problems, treat it like a medical alert. Don’t assume it’s heartburn or a cold.
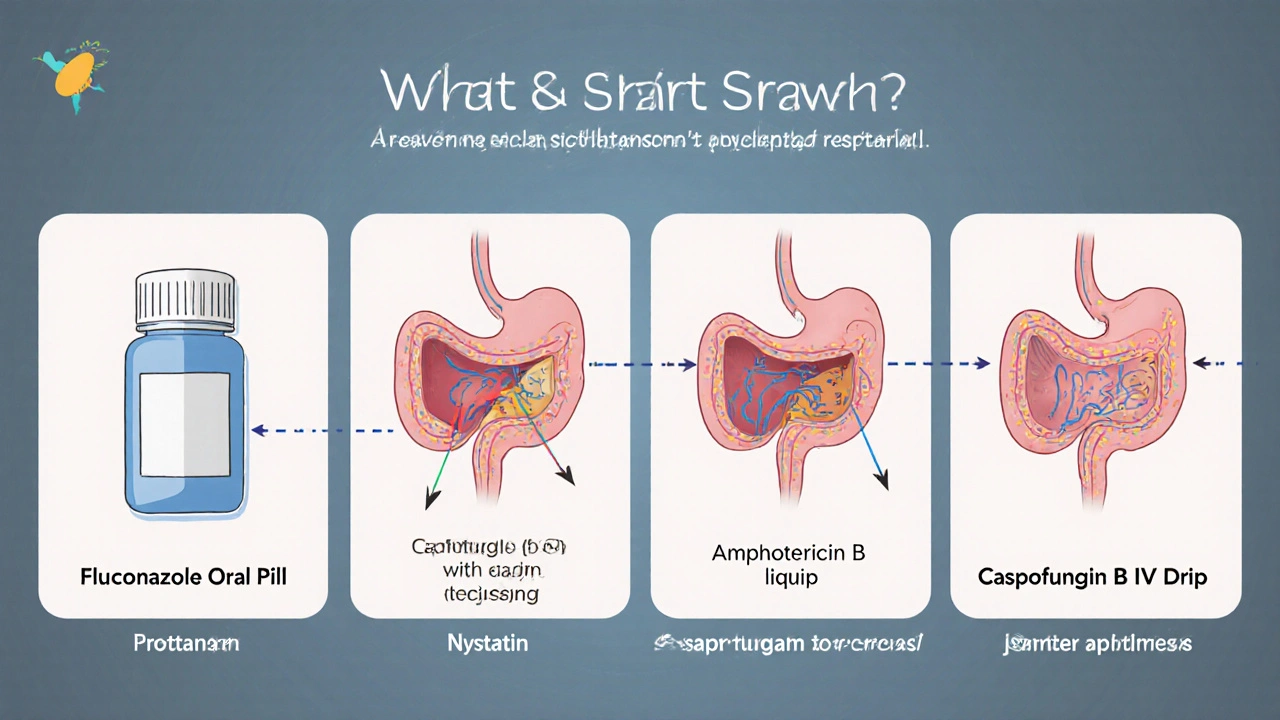
Fluconazole vs. Other Treatments
There are other options, but fluconazole remains the first choice for most cases.
| Treatment | Route | Dosing | Effectiveness | Side Effects |
|---|---|---|---|---|
| Fluconazole | Oral | 200 mg day 1, then 100 mg daily | 85-95% | Mild: nausea, headache |
| Nystatin | Oral suspension (swish and swallow) | 4-6 times daily for 14 days | 50-70% | Bitter taste, stomach upset |
| Itraconazole | Oral capsule | 200 mg daily | 80-90% | Liver enzyme changes, drug interactions |
| Amphotericin B | IV | 0.3-0.7 mg/kg daily | 90%+ | Fever, chills, kidney damage |
| Caspofungin | IV | 70 mg day 1, then 50 mg daily | 85-90% | Headache, nausea, low potassium |
Topical treatments like nystatin are often tried first in mild cases, but they’re less reliable for esophageal infections because they don’t reach deep enough. IV drugs like amphotericin B are powerful but too harsh for routine use. Fluconazole hits the sweet spot: effective, safe, and easy to take.
Common Myths About Fluconazole and Yeast Infections
There’s a lot of misinformation out there.
- Myth: Fluconazole cures all yeast infections. Truth: It works for esophageal and vaginal candida, but not for skin or nail infections-those need different antifungals.
- Myth: You can take fluconazole as a preventive if you eat sugar. Truth: Diet alone doesn’t cause esophageal candida. Immune status matters far more.
- Myth: One pill is enough. Truth: A single dose might help oral thrush, but esophagitis needs a full 2-week course.
- Myth: Fluconazole makes you immune to future infections. Truth: It treats the current infection, but doesn’t prevent new ones unless you fix the underlying cause.
Understanding these myths helps you avoid mistakes that lead to relapse or resistance.
Can fluconazole cause liver damage?
Rarely, but it’s possible. Fluconazole is generally safe for short-term use. Liver enzyme changes happen in less than 1% of patients. If you’re on long-term therapy or have existing liver disease, your doctor will monitor your liver function with blood tests. Stop taking it and call your doctor if you notice yellowing skin, dark urine, or persistent nausea.
Is fluconazole safe during pregnancy?
High doses (400-800 mg daily) are linked to birth defects and should be avoided. Low-dose, short-term use (like the 100-200 mg for esophagitis) is considered low risk, but only if benefits outweigh risks. Always tell your doctor if you’re pregnant or planning to be. For pregnant women with candida esophagitis, topical treatments like nystatin are often tried first.
How long until fluconazole starts working?
Most people notice improvement in swallowing pain within 3 to 5 days. But don’t stop taking it then. The infection may still be present under the surface. Completing the full 14-21 day course reduces the chance of the infection coming back.
Can I drink alcohol while taking fluconazole?
There’s no direct dangerous interaction between fluconazole and alcohol. But both can cause liver stress, and alcohol can worsen nausea or stomach upset. It’s best to avoid alcohol while you’re on treatment, especially if you have other risk factors like diabetes or liver disease.
Will I need a follow-up endoscopy after treatment?
Usually not-if symptoms resolve and you’re not immunocompromised. But if you have HIV, cancer, or a transplant, your doctor may recommend a repeat endoscopy to confirm the infection is gone. In some cases, they’ll also test for drug-resistant strains if symptoms return.
Final Thoughts
Fluconazole is a powerful tool for treating candida esophagitis, especially for those with weakened immunity. But it’s not a magic bullet. Its success depends on taking it correctly, understanding why the infection happened in the first place, and making changes to prevent it from returning. If you’re at risk, focus on immune health, avoid unnecessary antibiotics, and don’t ignore swallowing pain. Early action saves you from longer treatments, hospital visits, and complications down the road.

Beth Banham
November 4, 2025 AT 05:44Been through this twice with my HIV meds. Fluconazole saved my life, but only because I didn't skip the last week. That metallic taste? Yeah, that's the fungus saying goodbye. Don't ignore it.
Brierly Davis
November 5, 2025 AT 09:12Just finished my 14-day course and wow-felt like a new person by day 5. No more choking on toast 😅 Thanks for the clear breakdown. I didn't realize how much I was avoiding food until it stopped hurting.
Ankit Yadav
November 6, 2025 AT 02:39Fluconazole works but only if you fix the root cause. My cousin took it three times in a year because he kept eating sugar and skipping his diabetes meds. No pill fixes bad habits. You gotta change the environment, not just treat the symptom
Meghan Rose
November 7, 2025 AT 22:00Wait so you're telling me I don't need to go keto to stop yeast? I've been avoiding carbs for 8 months and still got this. So it's not sugar? Then why does everyone say sugar feeds it? I'm confused now.
Steve Phillips
November 9, 2025 AT 13:39Ohhh, so you're telling me this isn't just a "yeast overgrowth" from eating yogurt and being "stressed"? I mean, come on-this is *medicine*, not a wellness influencer's TikTok. Fluconazole? Yes. Nystatin swish-and-swallow? Please. That's like using a toothpick to fix a leaking dam. Pathetic.
Rachel Puno
November 11, 2025 AT 03:23You got this. Seriously. I was scared to swallow water after my chemo and now I'm eating tacos again. One pill a day. Two weeks. Done. Your body is stronger than you think. Keep going
Clyde Verdin Jr
November 11, 2025 AT 08:02Fluconazole? More like Fluconazole™-the corporate antifungal that’s been pushing this for 20 years while Big Pharma hides the real cure: probiotics and fasting. Also, why is no one talking about the fact that this is basically a symptom of capitalism? You’re sick because you can’t afford real food. Just saying.
Key Davis
November 13, 2025 AT 00:47It is of paramount importance to underscore that the administration of fluconazole, while efficacious, must be undertaken under the direct supervision of a qualified medical practitioner. The potential for hepatic adverse events, though statistically infrequent, necessitates vigilant monitoring, particularly in patients with preexisting hepatic insufficiency or concomitant polypharmacy.
Cris Ceceris
November 14, 2025 AT 01:51I wonder if the real issue isn't the fungus, but the way we've disconnected from our bodies. We suppress symptoms with pills, but never ask why the immune system let it happen in the first place. Is it stress? Sleep? The air we breathe? Fluconazole fixes the symptom, but the question remains: what broke the balance?
Brad Seymour
November 15, 2025 AT 02:26Great post. I'm from the UK and we see this a lot with transplant patients here too. The key is early diagnosis-too many wait till they're in agony. Fluconazole's cheap, easy, and works. No drama. Just do the 14 days and get on with life.
Malia Blom
November 15, 2025 AT 17:16What if fluconazole isn't the answer? What if the real problem is that we've pathologized a natural fungal presence in our bodies? Maybe Candida isn't the enemy-it's our fear of imperfection. We're terrified of imbalance so we reach for pills instead of asking why we're so out of sync in the first place. The pill treats the symptom, but the soul? The soul stays silent