When working with Medication safety, the practice of ensuring that prescription and over‑the‑counter drugs are used correctly to avoid harm. Also known as drug safety, it forms the backbone of responsible healthcare and protects patients from preventable errors. In everyday life, safety isn’t just a checklist; it’s a mindset that blends science, communication, and vigilance. Adverse effects, unintended harmful reactions that can occur after taking a medication are the most visible sign that something went wrong, while Drug interactions, the way two or more substances affect each other's activity in the body often hide behind the scenes, ready to amplify risks. Dosage monitoring, regular checks of how much medicine a patient receives and how their body responds ties everything together, turning raw data into actionable decisions. Together these entities create a safety net: Medication safety encompasses adverse effect monitoring, drug interactions influence safety outcomes, and dosage monitoring requires patient counseling to stay effective.
First, understanding adverse effects means recognizing patterns—rash, nausea, or more subtle lab changes can signal a problem. Health professionals rely on pharmacovigilance databases, while patients benefit from simple tools like symptom diaries. Second, drug interactions are not limited to prescription meds; supplements, foods, and even herbal teas can tip the balance. A classic example is grapefruit juice boosting certain heart medications, turning a normal dose into a toxic one. Third, dosage monitoring isn’t just about numbers on a bottle; it involves timing, renal function checks, and adjusting for age or weight. When providers combine these practices with clear patient counseling, they reduce the incidence of preventable hospital visits. Studies from major hospitals show that structured medication safety programs cut adverse drug events by up to 30 % within a year, proving that each component—monitoring, education, and interaction checks—adds measurable value.
Beyond the clinical side, safety extends to the environment where medicines are stored and dispensed. Proper labeling, child‑proof packaging, and secure disposal prevent accidental ingestions. Digital tools like e‑prescribing platforms flag potential interactions before the prescription leaves the screen, while pharmacy technicians double‑check doses during dispensing. For patients, setting reminders, using pill organizers, and keeping an up‑to‑date medication list empower them to stay on top of their therapy. All these steps form a cohesive system: safety guidelines reduce risk, monitoring catches issues early, and patient involvement ensures the plan stays realistic. Below you’ll find a curated collection of articles that dive deep into each of these areas, from fungal eye infection treatments to blood pressure drug comparisons, all examined through the lens of safety. Explore the posts to see real‑world applications, dosage tips, and safety checks that can help you make informed choices.
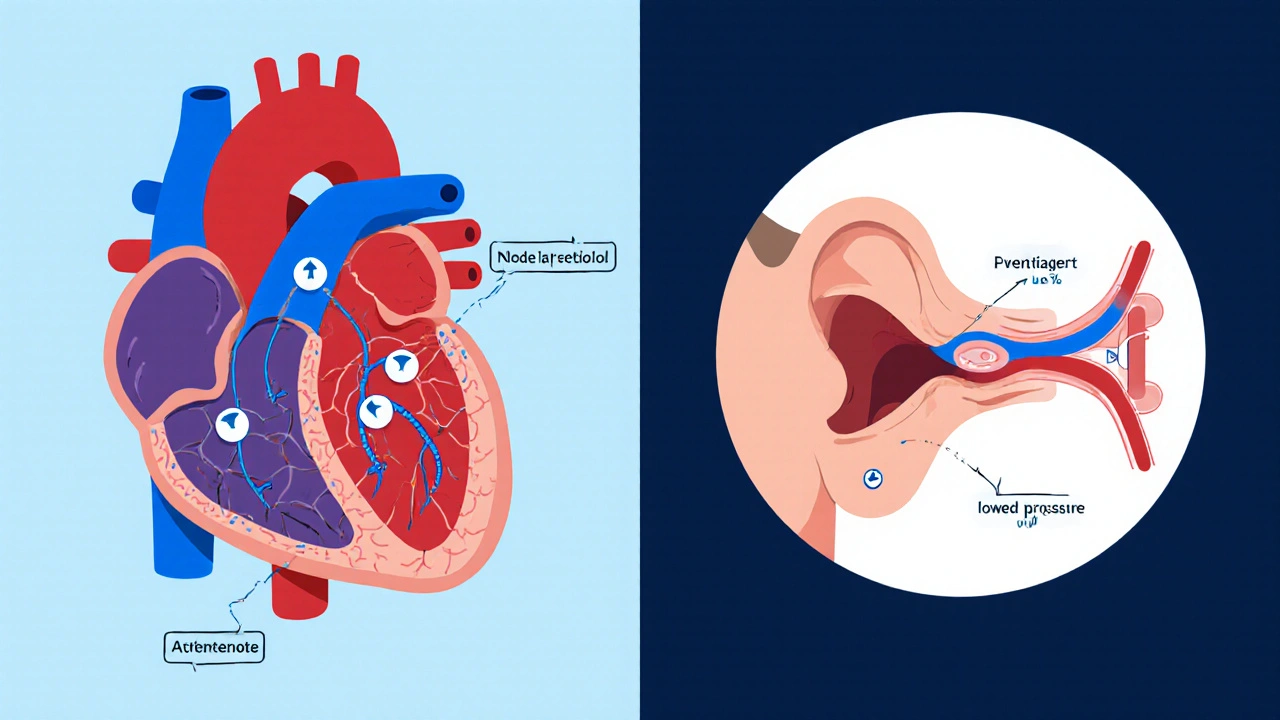
Explore how atenolol can affect balance, why dizziness happens, who’s most at risk, and practical steps to stay safe while using the medication.