When you pick up a prescription for Atenolol is a beta‑blocker used to lower blood pressure and treat heart‑related conditions, the focus is often on heart rate, not on whether it might make you feel off‑balance.
What is Atenolol?
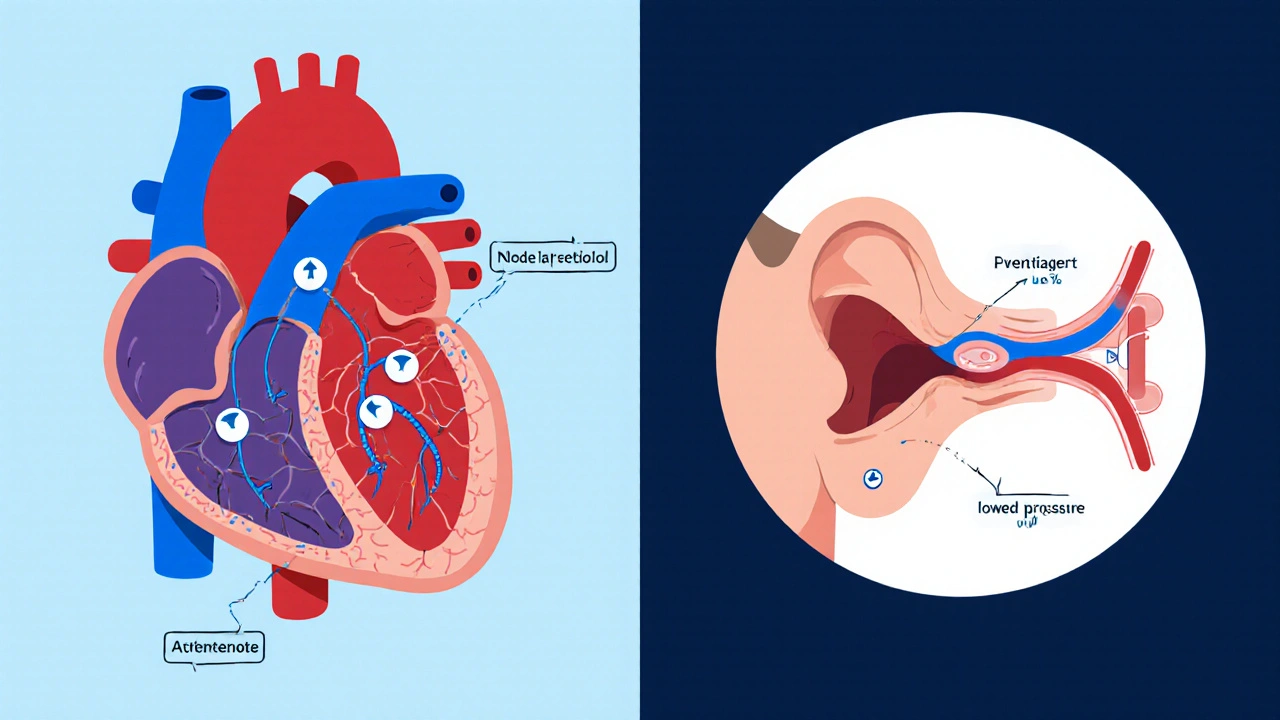
Atenolol belongs to the Beta‑blocker class. It works by blocking the action of adrenaline on β‑adrenergic receptors, which slows the heart and lowers blood pressure. Typical adult doses range from 50 mg to 100 mg once daily, and the drug’s half‑life is about 6-7 hours.
How Atenolol Works
By reducing the heart’s workload, atenolol helps prevent spikes in blood pressure. The drug also mildly dampens the sympathetic nervous system, which can lead to a calming effect on the entire cardiovascular system. This calming is usually a good thing, but it also means the body’s automatic balance‑keeping signals can become less responsive.
Why Some People Feel Dizzy
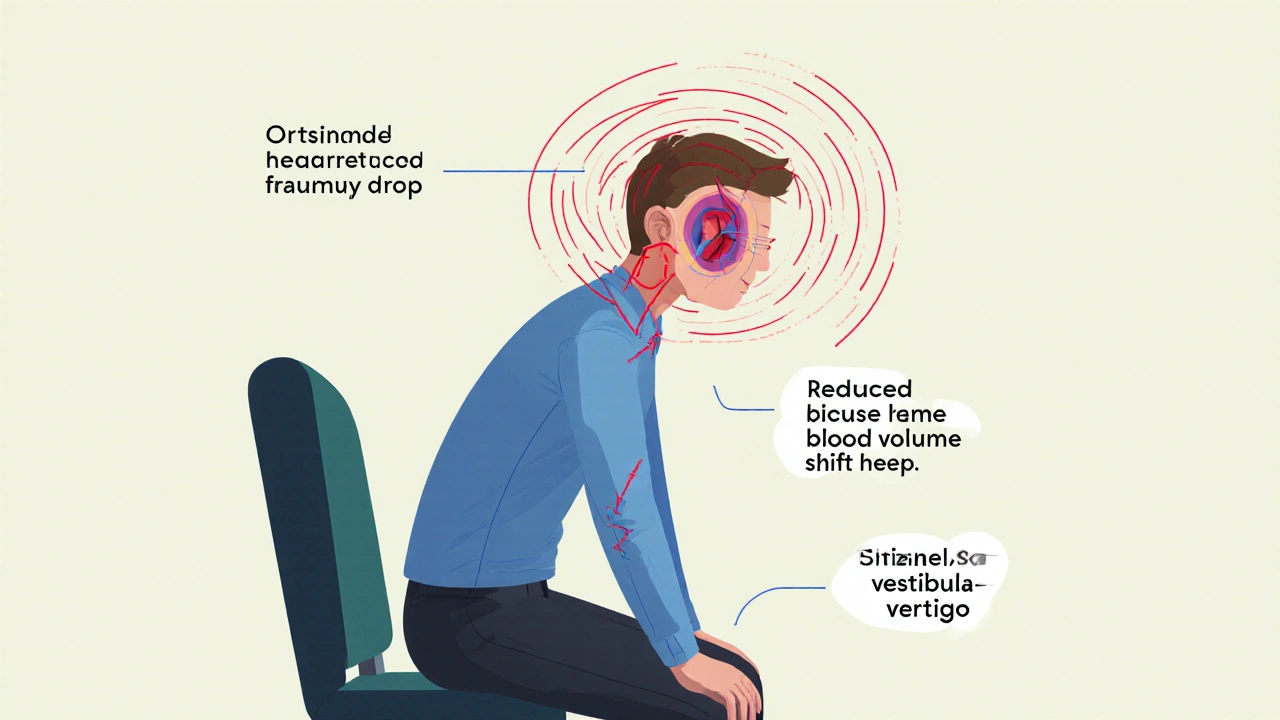
Dizziness and the more specific sensation of vertigo are reported side effects in up to 12 % of users, according to a 2023 meta‑analysis of beta‑blocker trials. The main mechanisms are:
- Lowered blood pressure that drops suddenly when you stand up (orthostatic hypotension).
- Reduced heart rate, which can limit the amount of blood reaching the inner ear.
- Interaction with other medications that also affect the vestibular system.
When the inner ear receives less blood, the brain’s balance center receives mixed signals, leading to that wobbly feeling.
Who’s Most Likely to Experience Balance Problems
Not everyone on atenolol gets dizzy, but certain groups have a higher fall risk:
- Elderly patients - age‑related decline in baroreceptor sensitivity makes orthostatic changes more pronounced.
- People on multiple drug interactions, especially diuretics, other antihypertensives, or sedatives.
- Individuals with pre‑existing vestibular disorders, such as Meniere’s disease.
- Those who consume alcohol heavily - alcohol already impairs balance.
If you fall into any of these categories, keep a close eye on how you feel after each dose.
Practical Tips to Manage Dizziness
Fortunately, most balance issues can be mitigated with simple habits:
- Rise slowly. When getting out of bed or a chair, pause for 10-15 seconds before standing.
- Stay hydrated. Dehydration lowers blood volume, worsening orthostatic drops.
- Monitor your blood pressure. Check sitting and standing readings; a drop of more than 20 mmHg systolic suggests a problem.
- Review other meds. Ask your pharmacist if any other prescription or over‑the‑counter drug could amplify the dizziness.
- Exercise balance. Simple heel‑to‑toe walks or yoga poses improve proprioception.
If dizziness persists despite these steps, it may be time to adjust the dose or switch drugs.
When to Talk to Your Doctor
Schedule a call or appointment if you notice any of the following:
- Frequent light‑headedness that interferes with daily activities.
- Fainting or near‑fainting episodes.
- New onset of vertigo that lasts more than a few minutes.
- Falls or near‑falls, especially when they happen without an obvious trip hazard.
- Unexplained fatigue that feels worse when standing.
Your provider might lower the atenolol dose, split it into twice‑daily dosing, or try a different class of blood‑pressure medication.
Alternatives to Atenolol for Blood Pressure Control
If balance issues become a deal‑breaker, consider these substitute options, each with its own side‑effect profile:
| Medication | Typical Dose | Half‑Life | Key Side‑Effects (incl. dizziness) |
|---|---|---|---|
| Atenolol | 50-100 mg daily | 6-7 h | Fatigue, dizziness (≈12 %), cold extremities |
| Metoprolol | 50-200 mg daily | 3-7 h | Bradycardia, dizziness (≈8 %), depression |
| Propranolol | 40-160 mg daily | 3-5 h | Bronchospasm, dizziness (≈10 %), sleep disturbances |
| ACE Inhibitor (Lisinopril) | 10-40 mg daily | 24 h | Cough, rare dizziness (<5 %) |
Switching to an ACE inhibitor like lisinopril often reduces the dizziness complaint because it works through a different pathway that doesn’t blunt the sympathetic response.
Quick Checklist - Stay Safe on Atenolol
- Measure blood pressure while seated and standing each week.
- Keep a symptom diary for the first two weeks of therapy.
- Discuss all current meds with your prescriber.
- Stay hydrated and rise slowly.
- Call your doctor if dizziness interferes with daily life.
Frequently Asked Questions
Can atenolol cause long‑term balance problems?
Most dizziness is temporary and linked to dose or dehydration. Long‑term issues are rare, and they usually disappear when the medication is adjusted or stopped.
Why do I feel dizzy only when I stand up quickly?
Atenolol can blunt the body’s quick reflex to raise blood pressure on standing (orthostatic hypotension). Slowing your rise lets the circulatory system catch up.
Is it safe to combine atenolol with a diuretic?
Combining them can increase the chance of low blood pressure and dizziness. Your doctor should monitor you closely and may adjust doses.
Should I stop atenolol if I start feeling dizzy?
Don’t stop suddenly; that can cause a rebound rise in heart rate. Instead, contact your prescriber-tweaking the dose is usually enough.
Are there lifestyle changes that reduce atenolol‑related dizziness?
Yes. Stay well‑hydrated, limit alcohol, use a chair to sit before standing, and do balance‑strengthening exercises twice a week.

Jacqueline Galvan
October 24, 2025 AT 13:24It is prudent to regularly assess both sitting and standing blood pressure readings when initiating atenolol therapy. A consistent drop of more than 20 mmHg systolic upon standing may herald orthostatic hypotension, which can precipitate balance disturbances. Keeping a simple log of these measurements alongside any episodes of light‑headedness enables your clinician to make data‑driven adjustments. Additionally, ensure adequate hydration throughout the day, as fluid deficits can exacerbate the hypotensive effect. Should you notice persistent dizziness, do not hesitate to schedule a follow‑up appointment for possible dose modification.
Tammy Watkins
October 24, 2025 AT 13:34When contemplating the introduction of atenolol into one’s pharmacologic regimen, it is essential to adopt a holistic perspective that encompasses both cardiovascular dynamics and vestibular integrity. The beta‑blockade mechanism, while efficacious in tempering sympathetic surges, inevitably attenuates the reflexive vasoconstriction that safeguards cerebral perfusion during postural transitions. Consequently, the abrupt shift from a supine to an upright stance may culminate in a transient diminution of cerebral blood flow, manifesting as vertigo or unsteady gait. Moreover, the drug’s propensity to lower heart rate can further limit the delivery of oxygenated blood to the labyrinthine structures of the inner ear, thereby compromising the vestibular apparatus. Patients with pre‑existing vestibular disorders, such as Menière’s disease, are particularly susceptible to this synergistic impairment. The literature indicates that up to twelve percent of atenolol users report dizziness, an incidence that, while modest, is clinically significant in geriatric cohorts. Age‑related attenuation of baroreceptor sensitivity exacerbates orthostatic challenges, rendering the elderly population a high‑risk group for fall‑related injuries. In parallel, polypharmacy-often involving diuretics, other antihypertensives, or sedatives-can potentiate hypotensive episodes through additive vasodilatory effects. Alcohol consumption, too, should be judiciously moderated, since ethanol itself diminishes central nervous system equilibrium. From a therapeutic standpoint, simple behavioral modifications can ameliorate many of these adverse sensations: rising slowly, maintaining adequate hydration, and engaging in proprioceptive exercises such as heel‑to‑toe walking or yoga. Monitoring blood pressure in both seated and standing positions furnishes objective data that can guide clinicians toward dose adjustment or regimen alteration. Should dizziness persist despite adherence to these measures, a strategic switch to an alternative class, such as an ACE inhibitor, may be warranted. It is paramount that patients communicate any episodes of near‑syncope, frequent light‑headedness, or falls to their healthcare provider promptly. By fostering an open dialogue and employing vigilant self‑monitoring, one can safeguard both cardiovascular health and postural stability, thereby preserving overall quality of life.
Dawn Bengel
October 24, 2025 AT 13:44This over‑prescription of atenolol is a classic American health‑care blunder 🙄.
Dason Avery
October 24, 2025 AT 13:54Consider the subtle dance between heart rate and the inner ear; when the rhythm slows too much, the equilibrium orchestra falters 😊. A mindful approach-rising gradually and staying hydrated-can keep the performance harmonious.
HILDA GONZALEZ SARAVIA
October 24, 2025 AT 14:04One practical tip that often goes overlooked is the timing of medication relative to daily activities. Taking atenolol at night can sometimes reduce the incidence of daytime dizziness, as the peak plasma concentration aligns with sleep rather than active hours. Conversely, if you find yourself feeling wobbly in the early morning, switching to a morning dose and pairing it with a light snack may stabilize blood pressure fluctuations. It is worth experimenting under medical supervision to discover the schedule that best suits your routine.
Amanda Vallery
October 24, 2025 AT 14:14Check ur BP both sitng nd standing, then talk to doc.
Marilyn Pientka
October 24, 2025 AT 14:24From an etiological standpoint, the iatrogenic destabilization of vestibular homeostasis induced by non‑selective β‑adrenergic antagonism constitutes a flagrant violation of the principle of primum non nocere. Such pharmacodynamic perturbations-manifesting as orthostatic hypotension and compromised cochlear perfusion-are emblematic of a therapeutic paradigm that privileges hemodynamic reduction over neurosensory preservation. The lexicon of contemporary cardiology ought to integrate vestibular risk stratification as a mandatory component of risk‑benefit analysis, lest clinicians perpetuate a reductionist model that marginalizes the somatic integrity of the patient. In summation, the deployment of atenolol without rigorous vestibular assessment is not merely a clinical oversight; it is an affront to the holistic ethos that undergirds evidence‑based medicine.
Carla Taylor
October 24, 2025 AT 14:34yeah that makes sense just take it slow and drink water
Michelle Capes
October 24, 2025 AT 14:44I totally get how scary that wobbliness can feel, especially if you have to get up for kids 😊. Keep a log of when it happens and share it with your doctor, it really helps.