Parkinson's psychosis, a neuropsychiatric condition that develops in some people with Parkinson’s disease, characterized by hallucinations, delusions, and sometimes confusion. It’s not just a side effect—it’s a direct result of brain changes caused by the disease itself, often worsening as Parkinson’s progresses. Also known as Parkinson’s disease psychosis, it affects up to half of all patients over time and is one of the most challenging non-motor symptoms to manage.
Parkinson’s psychosis doesn’t happen out of nowhere. It’s closely tied to the same brain chemicals that cause tremors and stiffness—especially dopamine. But here’s the catch: the very drugs that help movement, like levodopa, can also trigger hallucinations. People start seeing people who aren’t there, hearing voices, or believing their spouse is an imposter. These aren’t just "bad dreams"—they’re real to the person experiencing them. And when doctors try to fix it by cutting dopamine meds, the tremors come back hard. That’s why treating Parkinson’s psychosis is like walking a tightrope.
That’s where antipsychotics, medications designed to reduce hallucinations and delusions without making movement worse. Also known as atypical antipsychotics, they’re the only class of drugs that can help without worsening Parkinson’s symptoms. Pimavanserin is the only one FDA-approved specifically for this, and it works differently than older antipsychotics—it doesn’t block dopamine the same way. Quetiapine and clozapine are also used off-label, but clozapine needs weekly blood tests because of rare but serious side effects. The key? Start low, go slow. And never use older antipsychotics like haloperidol—they can paralyze someone with Parkinson’s.
It’s not just about pills. dementia with Lewy bodies, a related brain disorder that shares the same abnormal protein buildup as Parkinson’s. Also known as Lewy body dementia, it often overlaps with Parkinson’s psychosis and can make symptoms harder to control. If someone has memory loss, confusion, and visual hallucinations along with movement issues, they might be dealing with both conditions. That changes the treatment plan. Sleep problems, infections, or even new medications can suddenly make psychosis worse. A simple urinary tract infection can trigger a psychotic episode in someone with Parkinson’s.
What you’ll find in the posts below are real, practical guides on how to read drug labels to spot risks, how to safely adjust meds like butylscopolamine or antipsychotics, and how to avoid dangerous interactions—like mixing MAOIs with cold medicines. You’ll see how therapeutic drug monitoring helps with NTI drugs, why some antibiotics can harm the nervous system, and how alternatives to common Parkinson’s meds are compared by doctors and patients. This isn’t theory. These are the exact tools and warnings that help families and clinicians make safer choices every day.
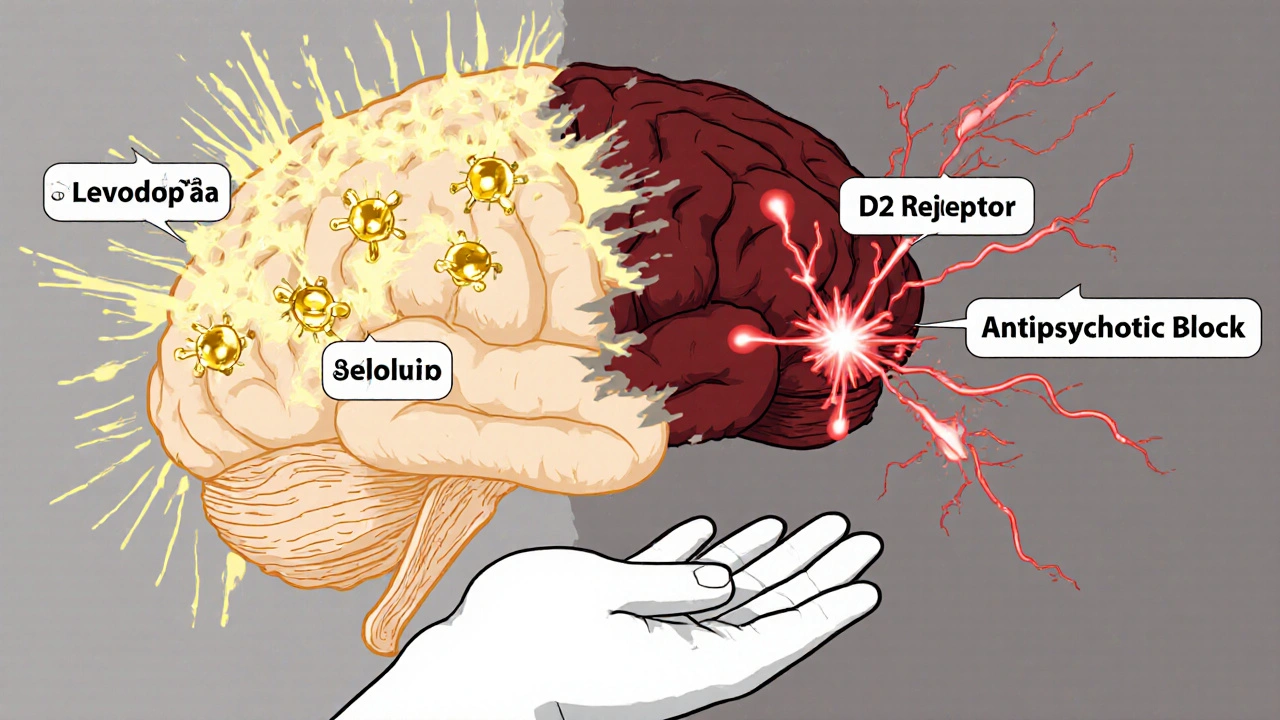
Levodopa and antipsychotics have opposing effects on dopamine, making it dangerous to use them together. This interaction can worsen Parkinson's symptoms or trigger psychosis, creating a difficult treatment dilemma for patients and doctors.