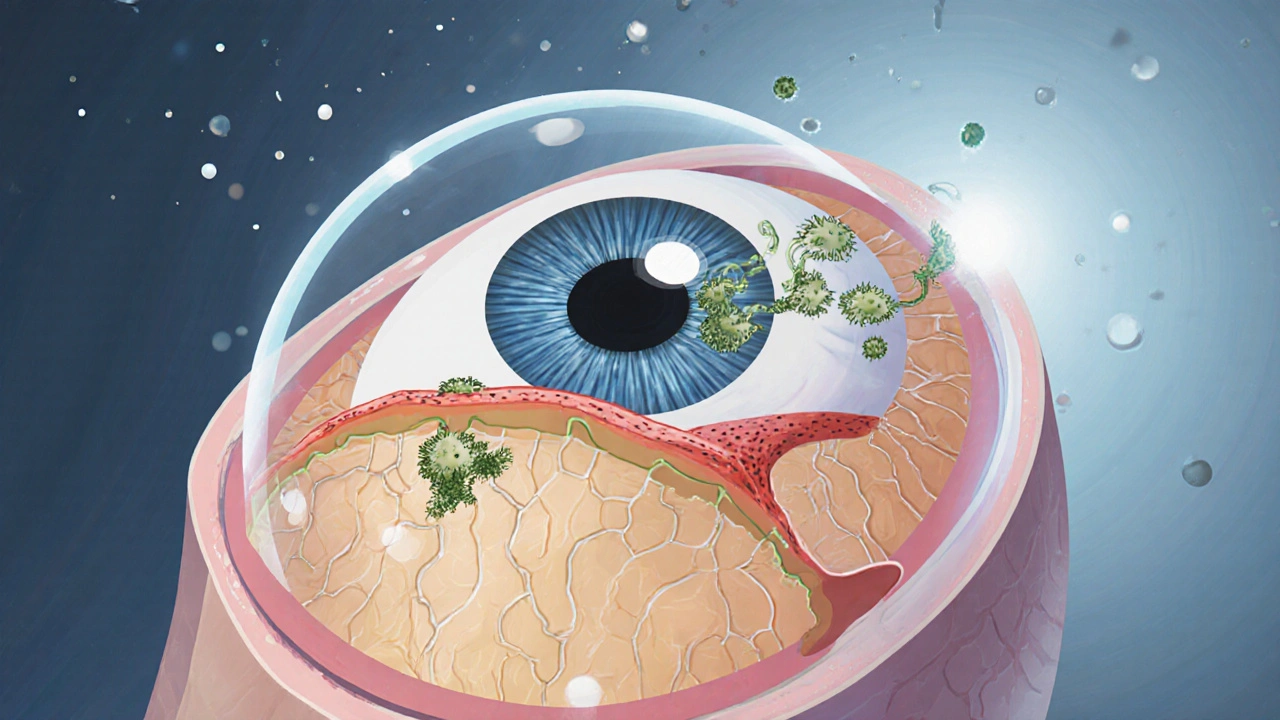
When dealing with ocular fungal infection, a fungal invasion of the eye that can affect the cornea, conjunctiva, or internal structures. Also known as fungal keratitis, it often begins after trauma, contact lens wear, or in an immune‑compromised host. Corneal ulcer, a breakdown in the corneal surface that can be caused by fungal organisms is a frequent complication, and prompt antifungal eye drops, medications like natamycin or voriconazole applied directly to the eye often decides whether vision is saved.
Fungal spores thrive in warm, moist environments, so outdoor activities such as gardening or farming raise exposure risk. Injuries that pierce the cornea with plant material can deposit mold or yeast right into the eye, creating a direct pathway for infection. People who wear extended‑use contact lenses, especially if hygiene is lax, provide a perfect breeding ground for fungi. Immunosuppressed patients—those on steroids, chemotherapy, or with HIV—also have a harder time fighting off these organisms, making them more vulnerable.
Understanding the link between ocular fungal infection and its triggers helps you spot danger early. For example, a sudden onset of pain, redness, and a gritty feeling after a garden accident should raise suspicion. Likewise, worsening vision despite antibiotic eye drops often signals that a fungus, not a bacterium, is at work. Recognizing these patterns lets you seek specialist care before the cornea thins into a full‑blown ulcer.
Diagnosis relies on a handful of practical steps. An eye doctor will perform a slit‑lamp examination to look for characteristic feathery borders or satellite lesions on the cornea. Samples collected with a sterile blade are sent for culture, and newer labs may run PCR tests that spot fungal DNA within hours. Imaging such as optical coherence tomography can map the depth of a corneal ulcer, guiding treatment intensity. In short, accurate diagnosis hinges on recognizing corneal ulcer features, collecting a specimen, and confirming the fungus with lab tests.
Once the culprit is identified, treatment centers on topical antifungal agents. Natamycin 5% eye drops remain the first‑line choice for filamentous fungi, while voriconazole or amphotericin B are preferred for yeasts. In severe cases, oral antifungals like itraconazole are added to achieve deeper tissue penetration. Patients must apply drops every hour initially and taper over weeks as the ulcer heals. Close follow‑up is essential because fungal infections can relapse or scar the cornea, potentially requiring a transplant.
Beyond medication, supportive care speeds recovery. Lubricating drops keep the eye moist, and protective eye shields prevent accidental rubbing. Avoiding corticosteroid drops until the infection is fully under control is critical, as steroids can worsen fungal growth. Lifestyle tweaks—like stopping contact lens wear, improving hand hygiene, and wearing eye protection during high‑risk activities—reduce the chance of a repeat infection.
In the end, the key takeaway is simple: spot the warning signs, get a proper diagnosis, and start the right antifungal therapy fast. Below you’ll find a curated list of articles that dive deeper into each aspect—risk factors, diagnostic tricks, medication comparisons, and real‑world case studies. Use them to build a solid game plan for preventing and managing ocular fungal infections in yourself or anyone you care for.
Learn how itraconazole treats fungal eye infections, with dosage guidelines, safety monitoring, and practical tips for patients and doctors.