When doctors need to stop dangerous blood clots from forming, they often turn to LMWH, low molecular weight heparin, a type of anticoagulant that prevents clots without requiring constant blood monitoring. Also known as low molecular weight heparin, it's a refined version of traditional heparin, designed to be more predictable and safer for long-term use. Unlike older blood thinners, LMWH doesn’t need frequent lab tests to check your blood’s clotting ability. That’s why it’s become a go-to for people recovering from surgery, those with deep vein thrombosis, or patients at risk for pulmonary embolism.
LMWH works by blocking a key protein in your blood called Factor Xa, which stops clots from growing. It’s usually given as a simple injection under the skin—often once or twice a day—and can be done at home. That’s a big reason why it’s preferred over intravenous heparin in many cases. You’ll find it used after hip or knee replacements, during cancer treatment (where clot risk is higher), and even in pregnancy when other blood thinners aren’t safe. It’s not for everyone—people with severe kidney problems or certain bleeding disorders need careful monitoring—but for millions, it’s a lifeline.
LMWH is closely tied to other important concepts in medication safety. For example, anticoagulants, medications that reduce blood clotting, including warfarin, direct oral anticoagulants (DOACs), and LMWH, require precise dosing and awareness of interactions. A missed dose or accidental overdose can lead to serious bleeding or clotting events, which is why knowing how to handle missed doses safely matters. And because LMWH is often prescribed long-term, medication adherence, the practice of taking your drugs exactly as prescribed, even when you feel fine becomes critical. People who skip doses because they forget or fear side effects put themselves at risk.
There’s also a strong link between LMWH and high-alert medications, drugs that carry a high risk of serious harm if misused, including insulin, opioids, and anticoagulants like LMWH. That’s why doctors and pharmacists use strict safety protocols—like clear labeling and double-checking doses—to prevent errors. If you’re on LMWH, you should always keep an updated medication list, document any safety alerts, and know how to recognize signs of bleeding or clotting.
The posts below cover everything you need to know about LMWH and the broader world of blood thinners. You’ll find real-world advice on avoiding missed doses, understanding drug safety alerts, managing side effects, and knowing when to ask your provider for alternatives. Whether you’re just starting LMWH therapy or have been on it for years, these guides help you take control—without the confusion.
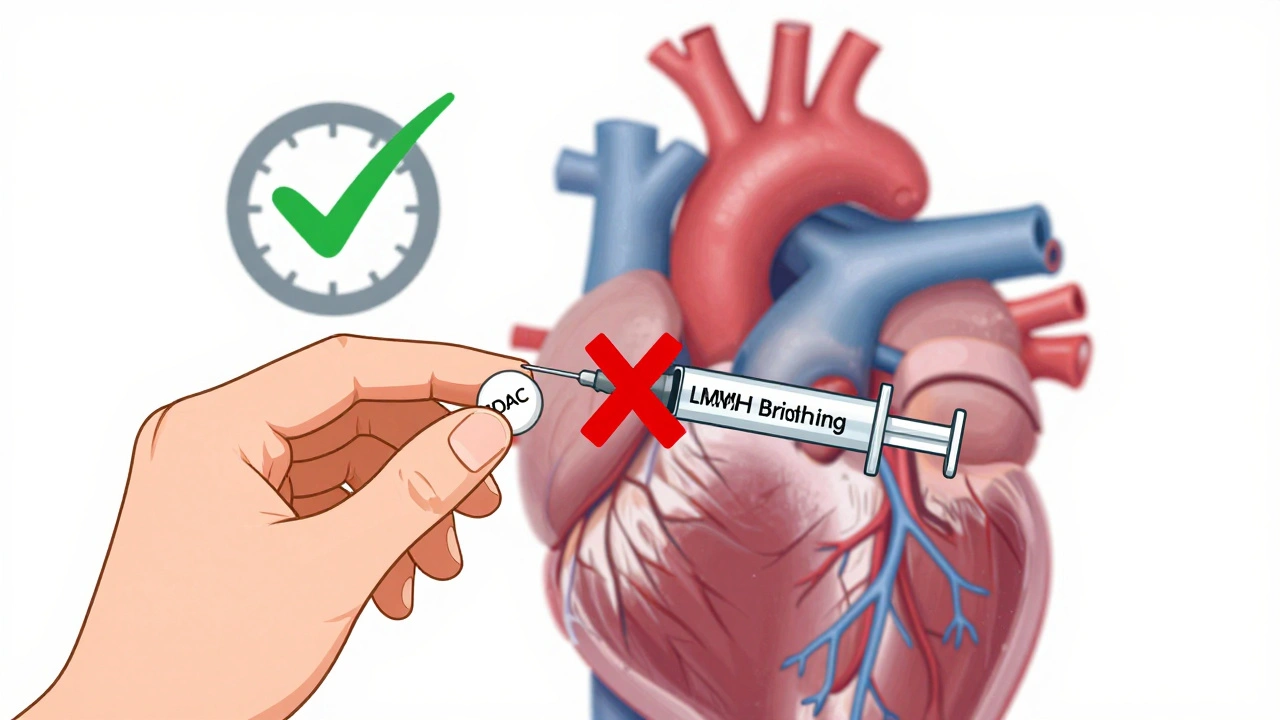
Learn when bridging therapy is truly needed when switching between blood thinners. Most patients don’t require it anymore - especially those on DOACs. Discover the latest guidelines, risks, and safe protocols for warfarin and newer anticoagulants.