Bridging Therapy Calculator
This tool helps you determine if bridging therapy is medically necessary when switching blood thinners before surgery. Based on the latest guidelines from the American Heart Association and American College of Cardiology, bridging therapy is only needed for a small percentage of patients.
Switching between blood thinners isn’t just a matter of stopping one pill and starting another. For many people on long-term anticoagulation, a surgical procedure or medical intervention means temporarily stopping their medication - and that’s where bridging therapy comes in. But here’s the catch: for most people, it’s no longer needed. The old standard - injecting heparin while waiting for warfarin to clear - is now seen as risky, not protective. If you’re on a blood thinner and facing a procedure, understanding when bridging is truly necessary could mean the difference between a smooth recovery and a dangerous bleed.
What Is Bridging Therapy, Really?
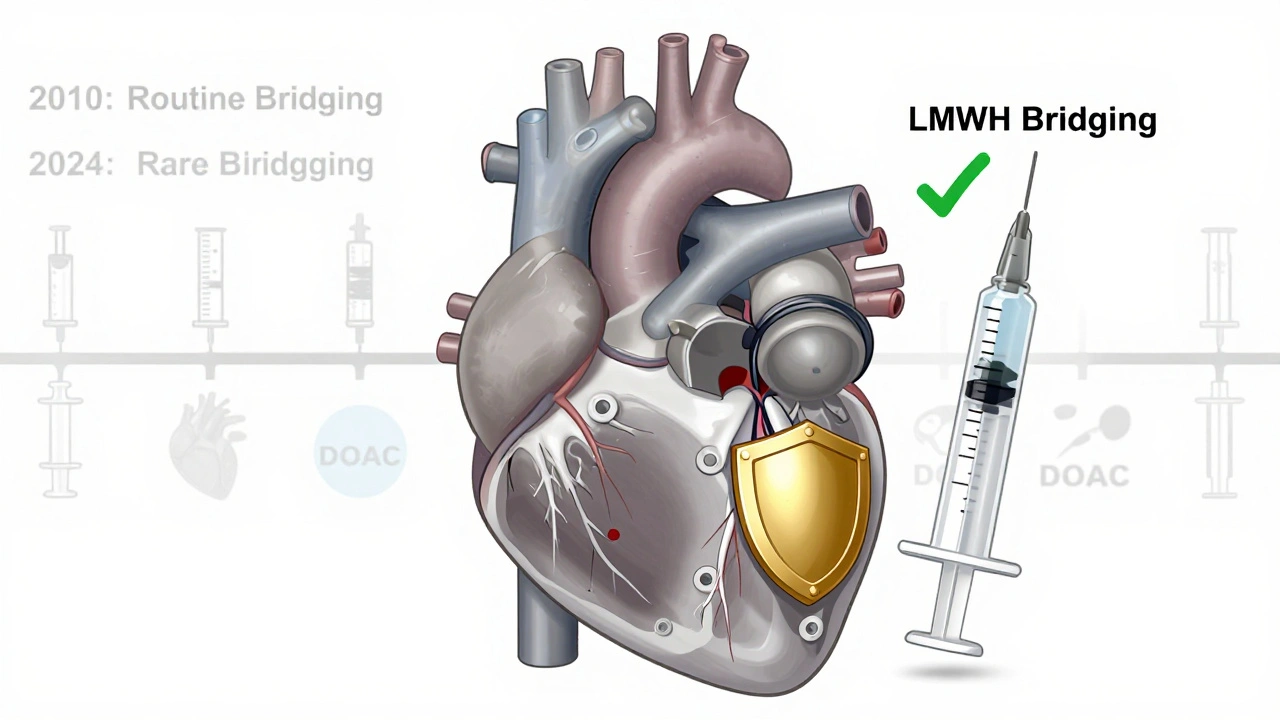
Bridging therapy means using a fast-acting injectable anticoagulant - usually low molecular weight heparin (LMWH) like enoxaparin - while you pause your long-term blood thinner, typically warfarin. The idea was simple: keep your blood from clotting during the gap when warfarin is out of your system. But research has flipped this logic on its head. The BRIDGE trial in 2015 changed everything. It followed over 1,800 patients with atrial fibrillation who stopped warfarin for surgery. Half got bridging with enoxaparin; half didn’t. The results? No drop in strokes or clots among those who got bridging. But their risk of major bleeding jumped from 1% to 2.3%. That’s more than double. And the PERIOP2 trial in 2020 confirmed it: even in high-risk patients, bridging didn’t prevent clots - it just caused more bleeding. Today, guidelines from the American Heart Association and the American College of Cardiology agree: bridging should be reserved for only the highest-risk cases. For most people, it’s not just unnecessary - it’s harmful.Who Actually Needs Bridging?
Not everyone on blood thinners needs bridging. In fact, fewer than 1 in 10 do. The only patients who still qualify are those with mechanical heart valves in the mitral position or those who’ve had a venous thromboembolism (like a DVT or pulmonary embolism) within the last three months. That’s it. If you have atrial fibrillation, a history of stroke, or even a high CHA₂DS₂-VASc score of 5 or more, you still don’t need bridging unless you fall into one of those two categories. The risk of bleeding from injections and overlapping anticoagulation outweighs any theoretical benefit. This is a big shift. Ten years ago, nearly half of all patients on warfarin got bridged before surgery. Now, it’s down to 10-15%. Why? Because we finally have data that proves bridging doesn’t save lives - it just adds risk.Why DOACs Made Bridging Obsolete
Direct oral anticoagulants (DOACs) - like apixaban (Eliquis), rivaroxaban (Xarelto), and dabigatran (Pradaxa) - changed the game. Unlike warfarin, which takes days to build up or wash out, DOACs work fast and leave fast. - Apixaban: half-life of 12 hours. Stop 24-48 hours before surgery. No bridging needed. - Rivaroxaban: half-life of 7-11 hours. Stop 24 hours before. No bridging. - Dabigatran: half-life of 12-17 hours (longer if kidney function is poor). Stop 2-5 days before, depending on creatinine clearance. Still no bridging. Because DOACs clear so quickly, you can safely pause them right before surgery and restart them as soon as bleeding risk drops - often within 24 hours. No injections. No INR checks. No guesswork. That’s why DOACs now make up 75% of all new anticoagulant prescriptions in 2023. They’re simpler, safer, and eliminate the need for bridging in almost every case.When Bridging Is Still Used: The Warfarin Protocol
If you’re still on warfarin - and you’re one of the rare few who need bridging - timing is everything. Here’s the standard protocol:- Stop warfarin 5-6 days before surgery. This lets your INR drop below 1.5.
- Start therapeutic-dose LMWH (like enoxaparin 1 mg/kg twice daily) 3 days before surgery.
- Stop LMWH 24 hours before the procedure.
- Restart warfarin 12-24 hours after surgery, at 15-20% higher than your usual dose.
- Check INR in 3-4 days. Adjust dose based on results.

What About After Surgery?
Restarting your blood thinner after surgery is just as critical as stopping it. Too early, and you bleed. Too late, and you clot. For DOACs: restart when your surgeon says it’s safe - usually 24 hours after minor procedures, 48-72 hours after major surgery. If you had spinal anesthesia, wait at least 24 hours to avoid spinal hematoma. For warfarin: restart at your usual dose or slightly higher (15-20% more), and check INR in 3-4 days. Don’t wait. If your INR is still low after 4 days, you may need a temporary bridge until it stabilizes - but only if you’re in the high-risk group.The Real Risks of Bridging
Bridging isn’t risk-free. Here’s what you’re really signing up for:- Bleeding: 2.3% major bleeding risk with bridging vs. 1% without. That’s not a small difference - it’s life-altering.
- Injections: Daily shots for up to a week. Many patients struggle with adherence - studies show 15-20% skip or delay doses.
- Cost: A 7-day course of LMWH in the U.S. costs $300-$500. In Australia, it’s covered under the PBS, but still adds administrative burden.
- Confusion: Multiple medications, timing changes, and unclear instructions lead to errors. One mis-timed injection can cause a bleed.
What Should You Do?
If you’re on a blood thinner and have surgery coming up:- Know which drug you’re on - warfarin or a DOAC?
- Ask your doctor: “Do I have a mechanical mitral valve or a clot in the last 3 months?” If not, you don’t need bridging.
- Confirm your INR is stable if you’re on warfarin.
- Discuss timing: When should you stop your drug? When should you restart?
- Ask for a written plan - not just verbal instructions.
What If You’re Still on Warfarin?
If you’re still on warfarin - and you’re not in the high-risk group - consider switching to a DOAC. The benefits are clear: no INR checks, fewer drug interactions, and no need for bridging. Talk to your doctor about whether you’re a candidate. Warfarin isn’t bad. It’s just outdated for most people. DOACs are safer, simpler, and more predictable. And if you’re already on warfarin, make sure your INR is well-controlled before any procedure. A stable INR reduces the need for bridging even further.Final Thought: Less Is More
The biggest mistake in anticoagulation isn’t stopping too late - it’s restarting too soon, or bridging when you don’t need to. We’ve spent decades thinking we had to keep blood thinners running at all costs. Now we know: sometimes, the safest thing you can do is nothing at all. For most people, the best bridge isn’t a shot - it’s time. Let your body clear the drug naturally. Restart when it’s safe. And trust the data: bridging saves almost no one, but it hurts many.Do I need bridging therapy if I’m on Eliquis or Xarelto?
No. Direct oral anticoagulants (DOACs) like Eliquis and Xarelto clear from your system quickly - usually within 24 to 48 hours. You simply stop taking them 1-2 days before surgery and restart once bleeding risk is low. No injections, no bridging needed.
What if I have a mechanical heart valve?
If you have a mechanical valve in the mitral position, you’re still considered high risk for clots. Bridging with LMWH is usually recommended when stopping warfarin for surgery. DOACs are not approved for mechanical valves, so warfarin remains the standard - and bridging may still be necessary.
How long before surgery should I stop warfarin?
Stop warfarin 5-6 days before surgery. This allows your INR to fall below 1.5. Your doctor may check your INR 2-3 days before stopping to confirm it’s trending down. Don’t stop earlier without guidance - too soon can raise your clot risk.
Can I skip the LMWH injection if I’m worried about bleeding?
If you’re not in the high-risk group (no mechanical mitral valve or recent clot), then yes - skipping bridging is the safer choice. The BRIDGE trial showed no increase in clots when bridging was skipped in most patients. Talk to your doctor about your individual risk - don’t assume you need it.
What happens if I miss an LMWH injection during bridging?
Missing one dose is usually not catastrophic, but it increases your clot risk. If you miss a dose, call your anticoagulation clinic or surgeon immediately. Don’t double up. They may adjust your schedule or delay your procedure. Consistency matters - bridging requires precise timing.
Is bridging therapy covered by Medicare or PBS in Australia?
Yes. Low molecular weight heparins like enoxaparin are covered under the Pharmaceutical Benefits Scheme (PBS) in Australia when prescribed for bridging therapy. You’ll pay the standard PBS co-payment. However, if you’re on a DOAC and don’t need bridging, you avoid these costs entirely.
Can I switch from warfarin to a DOAC before my surgery?
Yes - and it’s often the best move. If you’re on warfarin and planning surgery, ask if switching to a DOAC is an option. It eliminates the need for bridging, INR checks, and dietary restrictions. Your doctor will check your kidney function and make sure you’re not at risk for clots before making the switch.
Next Steps
If you’re preparing for surgery and on a blood thinner:- Write down your current medication and dose.
- Know your INR if you’re on warfarin.
- Ask your doctor: “Am I in the 10-15% who need bridging?”
- Request a written plan - including stop/restart dates.
- If you’re on warfarin and not high risk, ask about switching to a DOAC.

Katie Harrison
December 9, 2025 AT 21:01I’ve been on Xarelto for AFib for 3 years now, and when I had my knee arthroscopy last year, my cardiologist just told me to skip it the day before and restart the next day. No shots. No panic. No INR checks. It felt so… simple.
Mona Schmidt
December 9, 2025 AT 22:30It’s fascinating how medicine evolves-not because of flashy new tech, but because we finally stopped assuming that more intervention equals better outcomes. The BRIDGE trial was a quiet revolution. We didn’t need to inject people with heparin to keep them safe; we just needed to trust the pharmacokinetics.
Michael Robinson
December 11, 2025 AT 10:33Less is more. That’s all you need to remember. Stop the pill. Wait. Start again. Sometimes the best treatment is doing nothing at all.
Andrea Petrov
December 11, 2025 AT 12:01Of course they say bridging isn’t needed. Big pharma pushed DOACs hard. Who benefits? The companies that sell Eliquis. The data? Probably cherry-picked. My uncle had a stroke after skipping bridging-do you think they’ll tell you that?
Graham Abbas
December 12, 2025 AT 21:17God, I love this. It’s like we finally stopped treating patients like they’re fragile porcelain dolls that will shatter if you stop giving them drugs. We’ve been overmedicating for decades, convinced that if we don’t act, something terrible will happen. Turns out, sometimes, the universe just… works.
Chris Marel
December 13, 2025 AT 12:09I’m from Nigeria, and here, most people still use warfarin because DOACs are too expensive. But even in our clinics, we’re starting to ask: do we really need to bridge? The bleeding risk is real-especially when people can’t get follow-up INR tests. This post made me rethink how we manage anticoagulation here.
Nikhil Pattni
December 14, 2025 AT 02:20Wait, hold on-I’ve been on warfarin for 12 years and I’ve had 3 surgeries, all with bridging, and I’ve never bled! So what’s your point? You’re telling me I was lucky? That’s not science, that’s statistics! Also, I use fish oil, turmeric, and garlic supplements-do you think that affects INR? I bet your ‘guidelines’ don’t even mention that! And why is everyone so obsessed with DOACs? Because they’re expensive? Because your doctor gets kickbacks? I’ve read the BRIDGE trial and it had selection bias-patients were too healthy! My neighbor’s cousin’s dentist had a clot after skipping bridging and now he’s in a wheelchair! So don’t tell me it’s safe!
Angela R. Cartes
December 16, 2025 AT 00:40Ugh. Another ‘evidence-based’ post. I bet the author works for Pfizer. 😒 I mean, really? No bridging? I’m gonna skip my next surgery because some study says it’s ‘safe.’ 😴
Andrea Beilstein
December 16, 2025 AT 04:18DOACs changed everything. No more needles. No more labs. No more ‘what if.’ Just take it. Stop it. Start it. It’s almost too easy. And that’s the point-we stopped overcomplicating things. The body knows what to do. We just had to get out of the way.
Asset Finance Komrade
December 16, 2025 AT 19:10One must consider the socioeconomic implications of this paradigm shift. The displacement of warfarin, a low-cost, globally accessible agent, by proprietary DOACs, introduces a new form of pharmaceutical hegemony. While the clinical data may appear compelling, one must question whether this transition serves patient welfare-or merely shareholder value. The notion that ‘less is more’ is a bourgeois aphorism that ignores structural inequities in access to care.
Delaine Kiara
December 18, 2025 AT 10:24Okay but what if your surgeon is a total idiot and insists on bridging anyway? I had a doc last year who said ‘I don’t care what the guidelines say, I’ve seen too many clots’ and made me get 7 days of shots. I cried in the parking lot. 😭
Ruth Witte
December 19, 2025 AT 01:53YES YES YES! This is the kind of info everyone needs to hear! 🙌 Stop the shots, trust the science, and let your body breathe! DOACs are the future and I’m so glad we’re moving away from the ‘more is better’ mindset! 🚀❤️