Does your child limp, have a swollen knee, or complain of morning stiffness? Those can be signs of juvenile arthritis (often called JIA). This page gives clear, practical steps for spotting problems, getting the right tests, and easing day-to-day life so kids can keep playing and learning.
Juvenile arthritis shows up in different ways. Common signs are persistent joint pain, swelling, warmth, stiffness (especially in the morning), limping, and unexplained fevers. Some kids have eye redness or blurred vision — that can be a sign of uveitis and needs fast attention.
Your pediatrician will listen to symptoms and check joints. Expect simple blood tests (like ESR, CRP, ANA, sometimes rheumatoid factor) and X-rays or ultrasound to look for inflammation. Many children are referred to a pediatric rheumatologist who specializes in JIA for a clear diagnosis and treatment plan.
Treatment focuses on reducing inflammation, controlling pain, and keeping joints working well. Options often include NSAIDs (ibuprofen or naproxen) for pain, disease-modifying drugs like methotrexate, and biologic medicines (for example, TNF inhibitors) when needed. Steroid injections can help a single swollen joint quickly.
Non-drug care matters a lot. Regular physical therapy helps keep muscles strong and joints flexible. Occupational therapy can suggest tools and school accommodations so kids can do classwork without pain. Simple home tips—warm baths before activity, cold packs after play, and gentle stretching—can cut flare-up time.
Eye checks are part of care for some kids with JIA. If your child’s subtype raises uveitis risk, the rheumatologist will schedule regular eye exams even when there are no eye symptoms. Growth and development should also be tracked—long-term inflammation or some medicines can affect growth, so doctors keep an eye on height and weight.
Practical daily tips: keep a symptom diary (time, activity, pain level), set a medicine routine tied to meals or bedtime, and talk with school staff about rest breaks or modified PE. Encourage low-impact exercise—swimming and cycling are great—and keep social activities going so your child doesn’t feel left out.
If pain suddenly gets worse, a joint becomes very red or hot, or your child has a high fever, call your doctor. For steady care, work with a pediatric rheumatologist to tailor medicines and therapies to your child’s life.
Want help finding reliable info or preparing questions for your next visit? Write down recent symptoms, note any medicine side effects, and bring that list to the appointment. Good communication with the care team makes daily life with juvenile arthritis easier for both kids and parents.
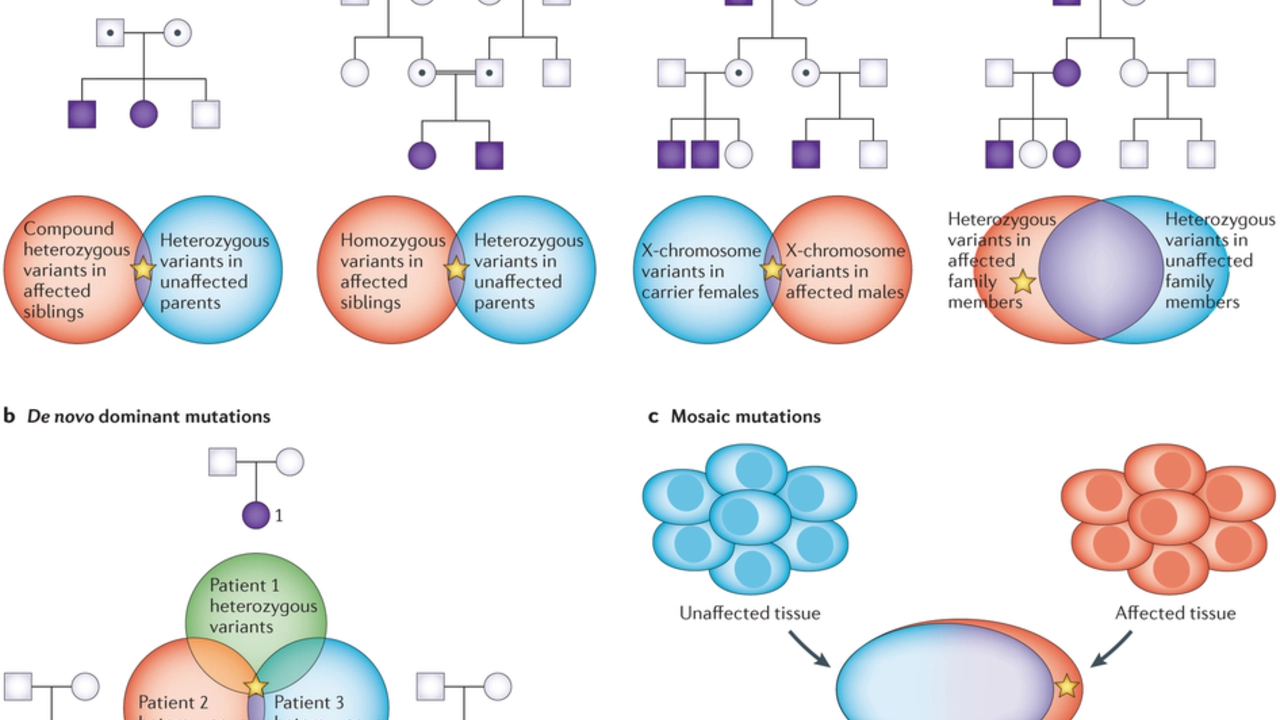
As someone who has been researching juvenile arthritis, I've discovered that there is a strong connection between this condition and genetics. Studies have shown that children with a family history of arthritis are at a higher risk of developing juvenile arthritis. Certain genes, such as HLA genes, have been identified as key players in this connection. This knowledge has led to better understanding and treatment options for those affected by the disease. It's fascinating to learn how our genes can play such a significant role in determining our health outcomes.