Understanding Juvenile Arthritis
Juvenile arthritis, or juvenile idiopathic arthritis (JIA), is a term used to describe a group of long-lasting, chronic joint conditions that affect children aged 16 and under. It is an autoimmune disorder, meaning that the immune system mistakenly attacks the body's own tissues, causing inflammation, pain, and stiffness in the joints. There are several types of juvenile arthritis, including oligoarticular, polyarticular, and systemic JIA, each with its own unique set of symptoms and challenges. In this article, we will explore the connection between juvenile arthritis and genetics, as well as what this means for affected children and their families.
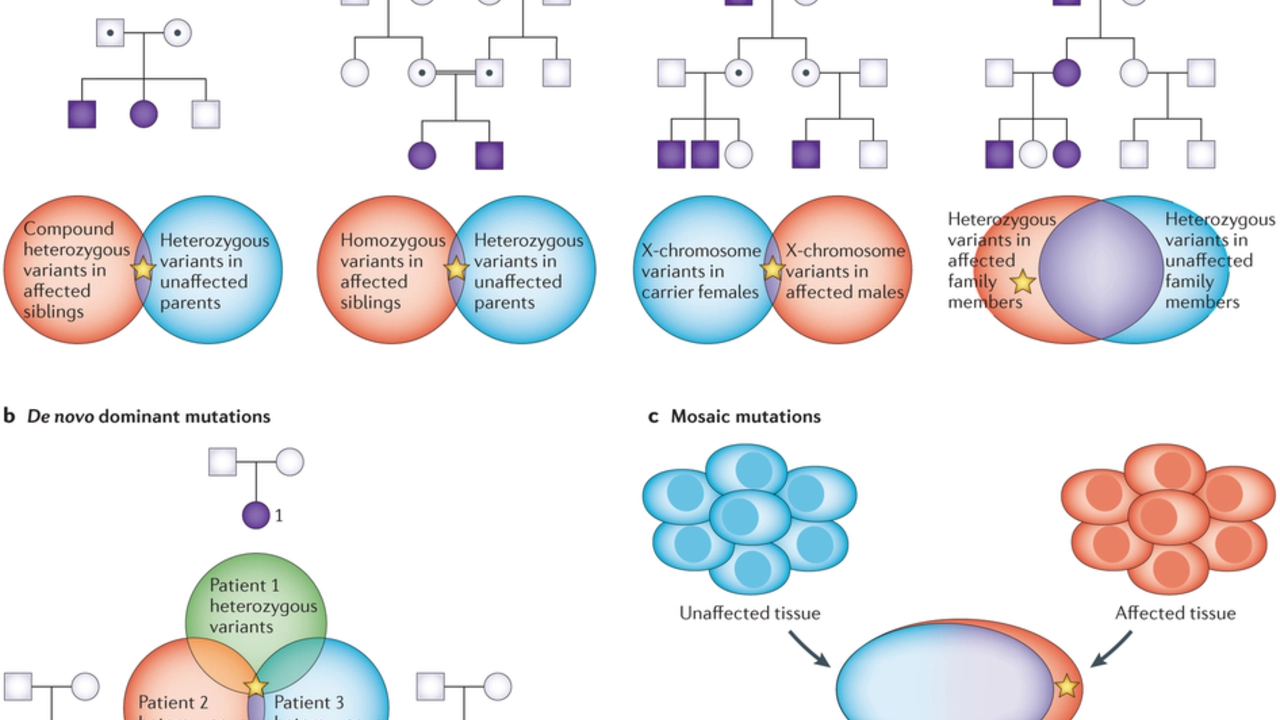
Genetic Factors in Juvenile Arthritis
While the exact cause of juvenile arthritis is still unknown, research has shown that genetics play a significant role in determining who will develop the condition. Several genes have been identified as being associated with an increased risk of juvenile arthritis, including those involved in the immune system and inflammation. These genes are passed down from parents to their children, making it more likely for a child to develop juvenile arthritis if they have a family history of the condition. However, it is important to note that having these genes does not guarantee a child will develop juvenile arthritis, as environmental factors also contribute to the development of the disease.
Environmental Triggers of Juvenile Arthritis
In addition to genetic factors, environmental triggers are believed to play a role in the development of juvenile arthritis. These triggers can include infections, injuries, and exposure to certain chemicals or allergens. For example, some studies have suggested that children who have experienced a severe infection may be more likely to develop juvenile arthritis later in life. However, more research is needed to fully understand the relationship between environmental factors and juvenile arthritis.
The Role of Epigenetics in Juvenile Arthritis
Epigenetics is the study of how genes can be turned on or off without changing the underlying DNA sequence. This process can be influenced by both genetic and environmental factors and is thought to play a significant role in the development of juvenile arthritis. For example, certain environmental triggers, such as infections or exposure to chemicals, may cause changes in gene expression that lead to the development of the disease. Understanding the role of epigenetics in juvenile arthritis may help researchers develop more targeted treatments for the condition.
Diagnosing Juvenile Arthritis: The Importance of Family History
Given the strong connection between juvenile arthritis and genetics, it is important for doctors to take a detailed family history when diagnosing a child with the condition. This information can help healthcare professionals determine whether a child is at an increased risk of developing juvenile arthritis and identify any potential environmental triggers that may be contributing to the disease. Additionally, understanding a child's family history can help doctors make more informed treatment decisions and provide better support for the child and their family.
Treatment Options for Juvenile Arthritis
Although there is currently no cure for juvenile arthritis, there are several treatment options available to help manage the symptoms and improve a child's quality of life. These treatments may include medication, physical therapy, and lifestyle changes, such as maintaining a healthy diet and getting regular exercise. In some cases, doctors may also recommend alternative therapies, such as acupuncture or massage, to help alleviate pain and inflammation. It is important for children with juvenile arthritis and their families to work closely with their healthcare team to develop a personalized treatment plan that best meets their needs.
Support for Children with Juvenile Arthritis and Their Families
Living with juvenile arthritis can be challenging for both children and their families. Fortunately, there are many resources available to help provide support and information on how to manage the condition. Organizations such as the Arthritis Foundation and the Childhood Arthritis and Rheumatology Research Alliance offer educational materials, online forums, and support groups for children with juvenile arthritis and their families. Additionally, healthcare professionals can provide guidance on navigating the healthcare system and accessing the necessary treatments and support services.
Future Research on Juvenile Arthritis and Genetics
As researchers continue to investigate the connection between juvenile arthritis and genetics, it is likely that we will gain a better understanding of the underlying causes of the disease and how to best treat it. This may include the development of more targeted therapies, as well as the identification of potential preventative measures for children at high risk of developing juvenile arthritis. By continuing to explore the relationship between genetics and juvenile arthritis, we can work towards improving the lives of affected children and their families.

Jason Montgomery
June 26, 2023 AT 08:50Hey everyone, just wanted to point out how important it is for families to stay positive and proactive. Knowing a family history of juvenile arthritis can be scary, but it also gives us a chance to catch symptoms early. Encourage regular check‑ups and keep an eye on any joint stiffness or pain. A supportive environment at home really makes a difference in managing the condition.
Wade Developer
June 27, 2023 AT 12:00The interplay between genetic predisposition and environmental exposures in juvenile idiopathic arthritis is a fascinating yet complex subject.
Current genome‑wide association studies have identified several HLA‑related loci that modestly increase susceptibility.
However, possessing these alleles does not equate to destiny; epigenetic modifications can either amplify or mitigate their impact.
For instance, DNA methylation patterns altered by early‑life infections have been shown to shift cytokine profiles toward a pro‑inflammatory state.
This mechanistic insight helps explain why two siblings with identical risk alleles may experience dramatically different disease courses.
Moreover, recent transcriptomic analyses suggest that microRNA dysregulation may serve as a molecular bridge between external triggers and gene expression.
From a clinical standpoint, taking a thorough family history remains indispensable, yet it should be complemented by a nuanced assessment of environmental risk factors such as viral exposures, trauma, and even dietary components.
In practice, early identification of at‑risk children allows for vigilant monitoring and, when appropriate, pre‑emptive lifestyle interventions.
Regular physical activity, for example, has been demonstrated to preserve joint function and potentially temper inflammatory pathways.
Likewise, ensuring adequate vitamin D levels may support immune regulation, although definitive causal evidence is still pending.
It is also worth noting that psychosocial stressors can exacerbate disease flares, highlighting the need for a holistic management plan.
Multidisciplinary teams that incorporate rheumatologists, physical therapists, and mental‑health professionals tend to achieve better long‑term outcomes.
As for therapeutic advances, biologic agents targeting specific cytokines such as IL‑1 and IL‑6 have already transformed the treatment landscape.
Ongoing trials are now exploring gene‑editing techniques and personalized vaccine strategies aimed at correcting underlying immunological dysregulation.
Ultimately, a deeper appreciation of both genetic and epigenetic contributors will pave the way toward truly individualized care for children living with JIA.
Sandra Perkins
June 28, 2023 AT 13:00Genetics is kool, but kids still need to play.
rama andika
June 29, 2023 AT 13:00Oh sure, the big pharma cabal probably engineered those "genetic" markers just to keep us buying their pricey biologics, right?
And let's not forget the shadowy lab rats that allegedly test every new drug on unsuspecting toddlers – because why not?
Meanwhile, the "environmental triggers" are just a convenient excuse for the government to push chemical exposure bans that never actually happen.
But hey, if you believe the glitter‑filled conspiracy, at least you have something exciting to talk about at family gatherings.
Just remember: the truth is out there, and it's probably hidden behind a wall of red tape and marketing brochures.
Kenny ANTOINE-EDOUARD
June 30, 2023 AT 13:00Building on Wade's comprehensive overview, I’d emphasize the practical steps clinicians can take today.
First, integrate a detailed pedigree analysis into the initial rheumatology visit; this data guides risk stratification.
Second, consider ordering HLA typing when the family history suggests a higher genetic load, remembering that results are probabilistic, not deterministic.
Third, employ early physical therapy referrals to preserve joint range of motion and prevent contractures.
Fourth, maintain vigilant monitoring for comorbidities such as uveitis, especially in oligoarticular presentations.
Fifth, discuss lifestyle modifications-balanced nutrition, regular low‑impact exercise, and adequate sleep-to complement pharmacologic therapy.
Finally, stay abreast of emerging epigenetic biomarkers, as they may soon inform personalized treatment algorithms.
By combining these evidence‑based measures, we can improve both short‑term symptom control and long‑term functional outcomes for children with JIA.