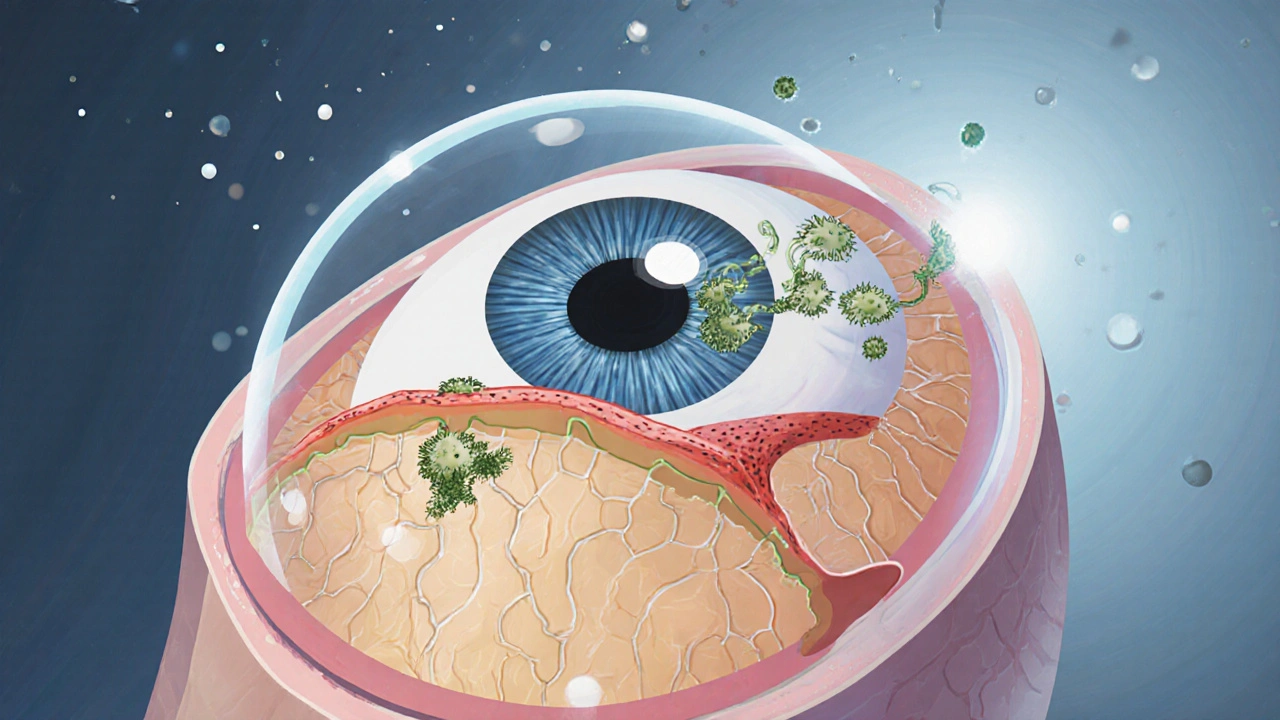
When dealing with itraconazole eye infection, a fungal infection of the eye treated with the antifungal drug itraconazole. Also known as fungal keratitis, this condition can threaten vision if not addressed promptly.
Another key player is itraconazole, an oral and topical antifungal medication that interferes with fungal cell membrane synthesis. It’s often formulated as eye drops or oral tablets, depending on infection severity. eye infection, any invasion of the ocular surface by pathogens, can be bacterial, viral, or fungal, but fungal cases demand a drug that can penetrate the cornea efficiently.
Fungal keratitis usually starts after trauma with plant material, contact lens misuse, or underlying eye disease. The fungus colonizes the corneal stroma, causing pain, redness, and blurred vision. Itraconazole eye infection treatment hinges on three facts: the fungus must be identified, the drug must reach therapeutic levels in the eye, and side effects must be monitored. Itraconazole’s mechanism—blocking ergosterol production—weakens the fungal cell membrane, allowing the immune system to clear the infection.
Practical dosing varies. For mild cases, ophthalmic solutions (1% or 2%) are applied every 2‑4 hours for the first 48‑72 hours, then tapered. Severe infections may need oral itraconazole at 200‑400 mg daily, combined with topical drops. Blood level monitoring is advised when using systemic therapy because itraconazole can affect liver enzymes.
Patients often ask about safety. Common side effects include mild burning, itching, or a transient yellowing of the skin with oral use. Rarely, liver toxicity occurs, so baseline liver function tests and periodic follow‑ups are wise. Interactions with certain heart medications, such as calcium channel blockers, can raise itraconazole levels—talk to your pharmacist before mixing drugs.
Beyond the drug itself, supportive care speeds recovery. Using preservative‑free artificial tears keeps the ocular surface moist, reducing discomfort. A protective shield at night prevents accidental rubbing, which could spread the fungus. If contact lenses are worn, they should be discarded until the infection clears.
When it comes to preventing recurrence, hygiene matters. Rinse hands before handling eyes, clean contact lens cases with hydrogen peroxide, and avoid swimming with lenses in. For agricultural workers, wearing safety goggles reduces trauma‑related fungal entry.
The collection of articles below dives deeper into each of these aspects. You’ll find comparisons between itraconazole and other antifungals, dosing calculators, patient stories, and step‑by‑step guides on managing side effects. Whether you’re a patient, caregiver, or eye‑care professional, the posts will give you the details you need to act confidently.
Ready to explore the full range of resources? Browse the list ahead to see practical advice, detailed drug comparisons, and real‑world tips for handling itraconazole eye infection effectively.
Learn how itraconazole treats fungal eye infections, with dosage guidelines, safety monitoring, and practical tips for patients and doctors.