One inherited gene can change how you react to a common medicine. That’s not rare — it’s why two people can take the same drug and one feels fine while the other gets strong side effects or no benefit. If you care about safer medication use and better health decisions, paying attention to inheritance matters.
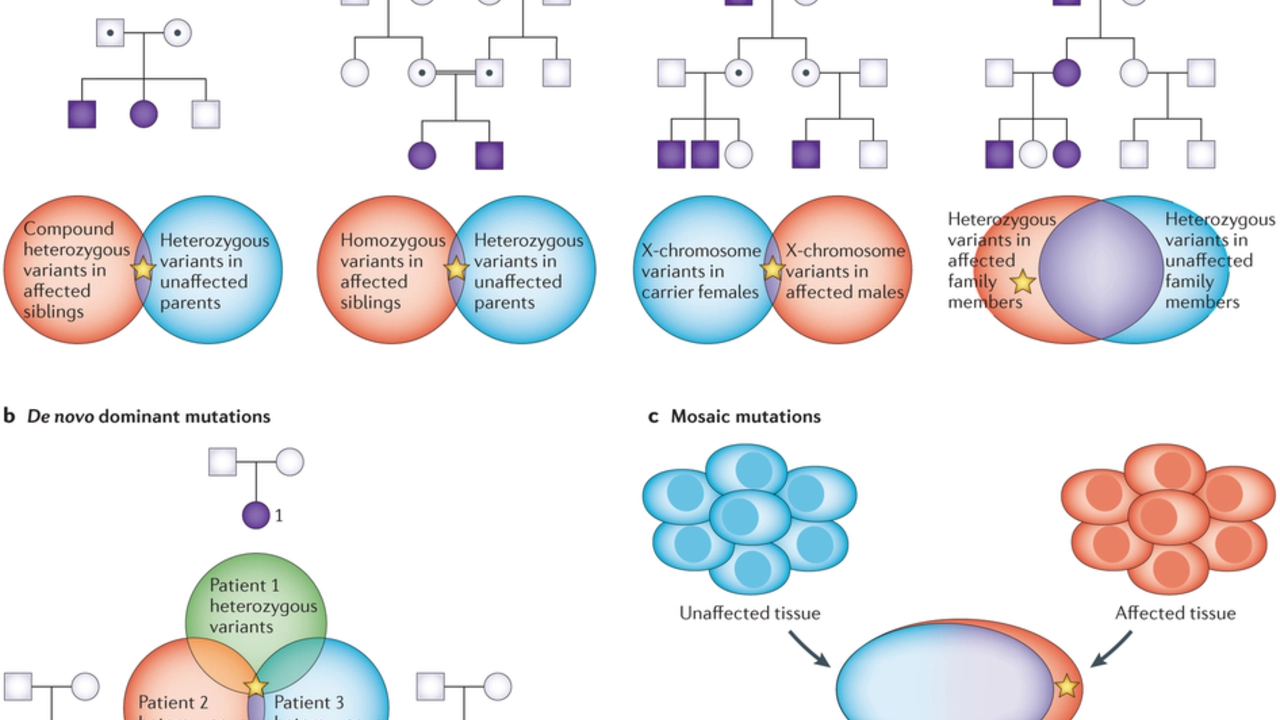
Inheritance simply means traits and risks passed down from parents to children. Some traits are obvious, like eye color. Others hide in DNA and affect disease risk, drug metabolism, or how your body handles nutrients. Knowing what runs in your family can help you and your clinician pick safer, more effective treatments.
Genes help build the proteins that break down drugs, carry them around the body, or make receptors that drugs bind to. Variations in those genes can speed up or slow down drug clearance, raise the chance of side effects, or make a drug ineffective. That’s the field of pharmacogenetics — matching medicines to your genes so treatment works better and risks drop.
Practical example: if a genetic test shows you metabolize a drug very slowly, your doctor might lower the dose or pick a different medicine. For other inherited conditions, like some forms of high cholesterol or blood clotting disorders, knowing your family history leads to earlier screening and targeted care.
Start with family history. Ask relatives about chronic diseases, sudden medical issues, bad reactions to drugs, or early-onset conditions. Tell your doctor what you learn. Bring specifics: names of conditions, ages at diagnosis, and any severe medication reactions.
Consider testing when it changes care. Pharmacogenetic panels and single-gene tests can be useful if you take certain medications or have a family history of inherited disease. A genetic counselor helps you understand test limits, privacy, and how results affect relatives. Tests aren’t always needed, but they’re worth it when results guide treatment choices.
Use trusted resources. Read medication guides and posts that explain drug risks and choices. For example, our articles on medications like Dilantin or Lamisil discuss use and safety — and family history or genetics can change how those drugs work for some people. If you’re trying new meds or managing chronic treatment, double-check whether genetics might play a role.
Privacy and planning matter. Genetic data is sensitive. Ask providers how results are stored and who sees them. If a test shows an inherited risk, think about family conversations and prevention steps, like earlier screening or lifestyle changes.
Final actionable tip: if you or close family members have unexplained diseases, strong drug reactions, or early-onset conditions, bring this up at your next medical visit. A simple conversation can lead to smarter testing, safer drugs, and clearer plans for your health and your family’s future.
As someone who has been researching juvenile arthritis, I've discovered that there is a strong connection between this condition and genetics. Studies have shown that children with a family history of arthritis are at a higher risk of developing juvenile arthritis. Certain genes, such as HLA genes, have been identified as key players in this connection. This knowledge has led to better understanding and treatment options for those affected by the disease. It's fascinating to learn how our genes can play such a significant role in determining our health outcomes.