When dealing with idiopathic pulmonary arterial hypertension, a rare, progressive disease marked by high blood pressure in the arteries that supply the lungs. Also known as IPAH, it primarily affects the small pulmonary arteries, leading to right‑heart strain and, if untreated, heart failure. Prostacyclin therapy, a class of potent vasodilators and platelet inhibitors is a cornerstone of modern care, while endothelin receptor antagonists, drugs that block the vasoconstrictive endothelin‑1 pathway and phosphodiesterase‑5 inhibitors, oral agents that boost nitric‑oxide signaling to relax pulmonary vessels round out the therapeutic toolbox. The disease idiopathic pulmonary arterial hypertension encompasses elevated pulmonary artery pressure, requires precise diagnosis, and demands lifelong medication management.
Understanding the condition starts with recognizing that IPAH is not caused by another disease; it arises spontaneously, making early detection tricky. The diagnostic pathway usually begins with an echocardiogram, followed by right‑heart catheterization to confirm the pressure readings. This step is crucial because right‑heart catheterization, the gold‑standard test that measures pulmonary artery pressure directly also helps rule out secondary causes. Once confirmed, treatment protocols kick in. Prostacyclin therapy influences vascular tone by mimicking natural prostacyclin, thus preventing vasoconstriction and platelet aggregation. Meanwhile, endothelin receptor antagonists counteract endothelin‑1, a molecule that narrows pulmonary arteries, and phosphodiesterase‑5 inhibitors enhance the nitric‑oxide pathway, providing complementary vasodilation.
These drug classes don’t work in isolation; they often overlap to maximize benefit. For example, a patient might start on an oral endothelin receptor antagonist and later add a prostacyclin infusion if symptoms persist. The combination approach reflects the reality that IPAH requires multi‑modal therapy to slow disease progression, improve exercise capacity, and extend survival. Research shows that patients on triple therapy—prostacyclin, endothelin antagonist, and a PDE‑5 inhibitor—experience better outcomes than those on a single agent. This synergy illustrates the semantic triple: “Treatment of IPAH requires vasodilator therapy,” and “Endothelin receptor antagonists influence vascular tone in IPAH.”
Beyond medication, lifestyle adjustments play a supporting role. Patients are encouraged to engage in low‑intensity aerobic activity, maintain a healthy weight, and avoid high altitudes or air travel without supplemental oxygen. Managing comorbidities such as sleep apnea or systemic hypertension can also reduce the workload on the right ventricle. While the focus of this tag page is on drug comparisons, the broader context includes these non‑pharmacologic measures that complement the medication regimen.
The articles listed below dive deep into specific drugs that often appear in IPAH treatment plans. You’ll find side‑effect profiles, cost considerations, dosing tips, and when each medication is most appropriate. Whether you’re comparing a prostacyclin infusion to an oral endothelin antagonist, or weighing the pros of a new PDE‑5 inhibitor against older options, the collection offers practical guidance to help you make informed decisions.
In the next section, the curated posts break down the most common therapies, highlight emerging alternatives, and answer real‑world questions about managing idiopathic pulmonary arterial hypertension. Browse through the comparisons to find the data that matches your situation, and use the insights to discuss the best plan with your healthcare team.
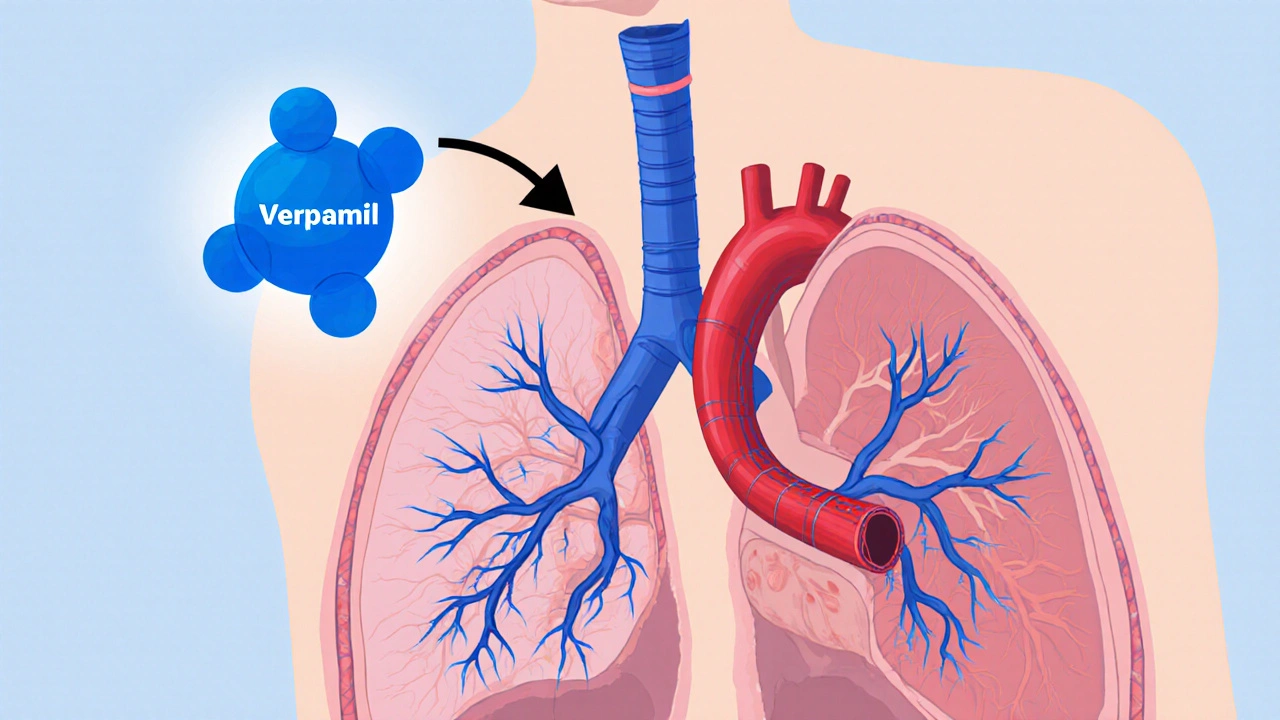
Explore how verapamil works for idiopathic pulmonary arterial hypertension, the evidence behind its use, patient selection, dosing, and future research.