Verapamil Vasoreactivity Response Calculator
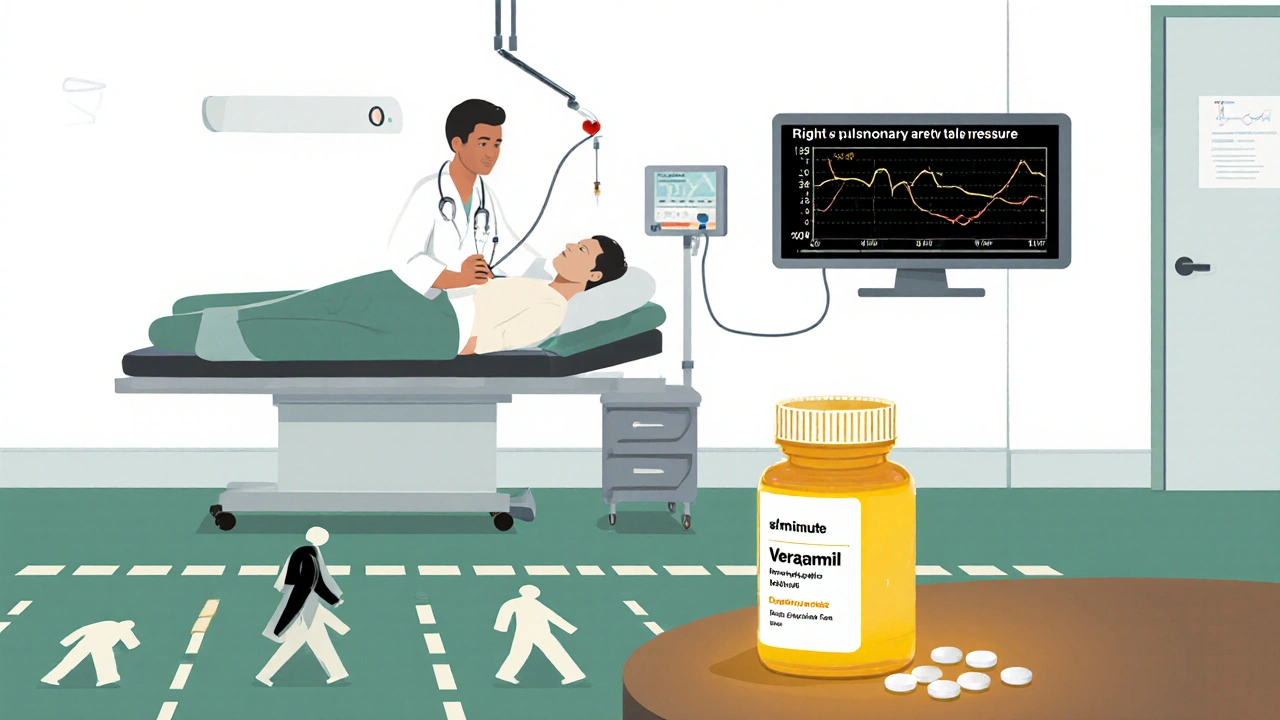
This calculator estimates potential treatment outcomes for idiopathic pulmonary arterial hypertension (iPAH) patients who demonstrate acute vasoreactivity. Verapamil should only be considered for patients who show a positive response during right heart catheterization testing.
The calculator uses clinical trial data showing verapamil reduces mean pulmonary artery pressure by approximately 6 mmHg and improves 6MWD by about 30 meters in responsive patients.
Results will appear here after calculation
When you hear the term verapamil in the context of pulmonary hypertension, you might wonder if a classic heart‑rate‑lowering drug can really help a rare lung disease. This article breaks down the science, digs into the trial data, and shows you when and how doctors actually use verapamil for idiopathic pulmonary arterial hypertension (iPAH).
Idiopathic pulmonary arterial hypertension is a progressive disorder characterised by elevated pressure in the pulmonary arteries without an identifiable cause. The condition leads to right‑ventricular strain, early fatigue, and, if untreated, a median survival of about three years. Diagnosis hinges on right heart catheterisation, which measures mean pulmonary artery pressure ≥25 mmHg at rest, pulmonary vascular resistance >3 Wood units, and a normal pulmonary capillary wedge pressure.
How Verapamil Works as a Calcium‑Channel Blocker
Verapamil is a non‑dihydropyridine calcium‑channel blocker (CCB) that inhibits L‑type calcium channels in both cardiac and vascular smooth muscle. By reducing intracellular calcium, it lowers systemic vascular resistance and slows heart‑rate conduction. In a subset of iPAH patients who display acute vasoreactivity during catheter‑based testing, this vasodilatory effect can translate into meaningful drops in pulmonary artery pressure.
Clinical Evidence: What the Trials Say
Randomised controlled trials (RCTs) and registry analyses form the backbone of our understanding. The pivotal 1997 RCT by Rich and colleagues enrolled 46 vasoreactive iPAH patients and randomised them to oral verapamil (80‑240 mg daily) or placebo. After 12 weeks, the verapamil arm showed a mean reduction of 6 mmHg in mean pulmonary artery pressure and a 30‑meter increase in six‑minute walk distance (6MWD). A 2008 follow‑up of the same cohort reported improved WHO functional class in 55% of responders.
More recent data from the REVEAL registry (2023 update) identified 212 vasoreactive patients on long‑term CCB therapy; 68% remained on treatment after five years, with survival rates comparable to those on targeted endothelin‑receptor antagonists. Importantly, patients who failed acute vasoreactivity testing showed no survival benefit from verapamil, underscoring the need for careful patient selection.
Comparing Verapamil with Other PAH Therapies
| Drug class | Typical first‑line use | Mechanism | Effect on 6MWD (median) | Common side‑effects |
|---|---|---|---|---|
| Calcium‑channel blocker (verapamil) | Vasoreactive patients only | L‑type calcium channel inhibition | +30 m | Constipation, bradycardia, edema |
| Endothelin‑receptor antagonist (bosentan) | All‑comers (often combination) | Endothelin‑1 blockade | +45 m | Elevated liver enzymes, anemia |
| Phosphodiesterase‑5 inhibitor (sildenafil) | All‑comers (often combination) | cGMP pathway enhancement | +40 m | Headache, dyspepsia, flushing |
| Prostacyclin analogue (epoprostenol) | High‑risk or refractory disease | Vasodilation via IP receptor | +60 m | Infusion site pain, thrombocytopenia |
The table makes it clear: verapamil’s niche is narrow but valuable. Its oral route, low cost, and modest efficacy are attractive when a patient demonstrates acute vasoreactivity during right heart catheterisation.
Practical Considerations: Dosing, Monitoring, and Safety
- Starting dose: 80 mg once daily, titrated up to 240 mg based on tolerance and haemodynamic response.
- Monitoring: Repeat right heart catheterisation after 12 weeks, assess mean pulmonary artery pressure, cardiac output, and 6MWD. Baseline ECG and liver function tests are recommended.
- Side‑effects: Look out for bradyarrhythmias, constipation, and peripheral edema. In patients with pre‑existing AV block, a permanent pacemaker may be required before initiating therapy.
- Drug interactions: Verapamil is metabolised by CYP3A4; co‑administration with strong inhibitors (e.g., ketoconazole) can raise plasma levels and increase toxicity.
Because CCBs can lower systemic blood pressure, clinicians often hold other antihypertensives during the uptitration phase to avoid symptomatic hypotension.
Patient Selection and Expected Outcomes
Acute vasoreactivity testing uses inhaled nitric oxide (10 ppm) or intravenous epoprostenol. A positive response is defined as a ≥10 mmHg fall in mean pulmonary artery pressure to an absolute value <40 mmHg without a drop in cardiac output. Roughly 10‑15% of iPAH patients meet this criterion.
For responders, longitudinal data show:
- Improvement in WHO functional class by at least one level in 60% of cases.
- Mean 6MWD increase of 25‑35 m over the first year.
- Five‑year survival approaching 80%, comparable to modern combination therapy.
Non‑responders should be transitioned to targeted therapies promptly; delaying escalation has been linked to a 30% rise in mortality over two years.
Future Directions: Ongoing Trials and Combination Strategies
Two phase‑III trials are currently recruiting (2025‑2028):
- VERA‑PAH: evaluates low‑dose verapamil plus sildenafil in vasoreactive patients, aiming to see additive improvements in 6MWD.
- CCB‑PLUS: tests verapamil together with an endothelin‑receptor antagonist for patients with borderline vasoreactivity.
Preliminary data suggest that modest vasodilation from verapamil may prime the pulmonary vasculature for better response to phosphodiesterase‑5 inhibition, but definitive results are still pending.
Take‑Home Points
- Verapamil is only effective in iPAH patients who exhibit acute vasoreactivity.
- Clinical trials report a mean 6MWD gain of ~30 m and survival rates similar to modern targeted agents when used appropriately.
- Regular haemodynamic monitoring and dose titration are essential to maximise benefit and limit side‑effects.
- For the majority of iPAH patients, combination therapy with endothelin‑receptor antagonists or phosphodiesterase‑5 inhibitors remains first‑line.
- Ongoing research may expand the role of verapamil beyond the strict vasoreactive subgroup.
What is acute vasoreactivity testing?
It is a short‑term challenge performed during right heart catheterisation, using inhaled nitric oxide or intravenous epoprostenol, to see if pulmonary pressures drop significantly. A positive test identifies patients who may respond to calcium‑channel blockers like verapamil.
How long does it take to see improvement with verapamil?
Most studies report measurable improvements in six‑minute walk distance and haemodynamics after 12 weeks of stable dosing, although some patients may need up to six months for maximal benefit.
Can verapamil be combined with other PAH drugs?
Yes, especially in research settings. Clinically, combination with endothelin‑receptor antagonists or phosphodiesterase‑5 inhibitors is being studied, but routine co‑administration should follow specialist guidance to avoid hypotension.
What are the most common side‑effects of verapamil in PAH patients?
Constipation, bradycardia, peripheral edema, and mild hypotension are reported. Monitoring ECG and blood pressure is essential, especially during dose escalation.
Is verapamil suitable for all PAH patients?
No. Only the small subgroup (≈10‑15%) who are vasoreactive benefit. For non‑responders, targeted therapies provide better outcomes.

Diane Thurman
October 22, 2025 AT 17:19Verapamil is only for a tiny slice of iPAH patients, and most folks get no benefit at all. The drug demands strict vasoreactivity testing, otherwise you’re just tossing pills. If you’re not in that responsive group, you’ll waste time and risk bradycardia. The guidlines are crystal clear about this narrow niche.
Iris Joy
October 28, 2025 AT 11:12When you’re managing idiopathic pulmonary arterial hypertension, the first step is always to confirm vasoreactivity; without that, verapamil is just another oral antihypertensive. The beauty of a calcium‑channel blocker is its oral administration, which many patients find far more convenient than an infusion. Starting at 80 mg once daily gives you a safe foothold, and you can titrate up to 240 mg as long as the heart rate and blood pressure stay stable. Regular ECGs are essential because you don’t want to slip into a high‑grade AV block unnoticed. Keep an eye on the six‑minute walk distance; a 30‑meter bump is a realistic goal in responders. Repeat right‑heart catheterisation after three months will show you whether the mean pulmonary artery pressure has dropped by that coveted ten millimeters of mercury. If the numbers don’t move, it’s time to consider switching to an endothelin receptor antagonist or a phosphodiesterase‑5 inhibitor. Monitoring liver function tests is also wise, even though verapamil isn’t notorious for hepatotoxicity, because many patients are on multiple agents. Educate patients about the potential for constipation; a fiber supplement can make a big difference. Don’t forget to assess peripheral edema, especially if they’re also on diuretics. In practice, you’ll see that only about 10‑15 % of the iPAH population qualifies as acute vasodilator responders. That small percentage, however, enjoys a survival curve that looks almost as good as patients on more expensive targeted therapies. The cost‑effectiveness of verapamil can’t be overstated for those who are truly eligible. Keep the medication list clean; strong CYP3A4 inhibitors like ketoconazole should be avoided or doses adjusted. Finally, have a frank discussion with your patients about the uncertainties and the need for close follow‑up, because shared decision‑making drives better adherence.
Sarah Riley
November 3, 2025 AT 06:05Verapamil’s L‑type calcium channel antagonism yields modest hemodynamic improvement in vasoreactive cohorts, yet its therapeutic index is narrow. Off‑label extrapolation to non‑responsive iPAH subpopulations is pharmacologically untenable.
Joe Waldron
November 9, 2025 AT 00:59Verapamil, when judiciously selected, offers a viable oral alternative; however, clinicians must adhere to strict vasoreactivity criteria, thereby minimizing exposure of non‑responders; routine hemodynamic reassessment at twelve weeks is indispensable, ensuring that mean pulmonary artery pressure trends downward; concomitant monitoring of bradyarrhythmic events, hepatic enzymes, and peripheral edema is mandatory; a multidisciplinary team approach optimizes patient outcomes.
Tim Blümel
November 14, 2025 AT 19:52Absolutely, the team effort makes the difference 😊. Even a modest drop in pressure can translate to better daily stamina, and that’s worth celebrating 🎉. Keeping an eye on side‑effects while titrating feels like walking a tightrope, but the payoff is real.
Joanne Ponnappa
November 20, 2025 AT 14:45Verapamil works best with the right test results 👍. It’s easy to take and not too pricey 💊.
Michael Vandiver
November 26, 2025 AT 09:39Got it, simple and cheap 😎
Don Goodman-Wilson
December 2, 2025 AT 04:32Oh great, another cheap pill for a deadly disease, as if that’ll magically fix everything. The pharma crowd loves to push these half‑baked solutions while they line their pockets. If you’re not a vasoreactive miracle, you might as well be sipping vitamin water.
Bret Toadabush
December 7, 2025 AT 23:25They dont tell u that most of the data is funded by the drug companies themselves, so the results are skewed. Looks like a big push to keep the profits rolling, dont ya think?
Sajeev Menon
December 13, 2025 AT 18:19It's true that industry funding can bias studies, however, the vasoreactivity criteria are well established in clinical guidelines. The long‑term registries still show a decent survival benefit for true responders. So while scepticism is healthy, the data isn’t all smoke and mirrors.
Emma Parker
December 19, 2025 AT 13:12Nice summry!
Wade Grindle
December 25, 2025 AT 08:05The pharmacodynamics of verapamil are well characterized; its effect on pulmonary vascular resistance is modest but measurable. In patients who meet the strict vasoreactivity definition, the drug can be a cost‑effective component of therapy.
Jai Reed
December 31, 2025 AT 02:59While the statement is accurate, clinicians must also consider individual tolerability and potential drug interactions. Ignoring these factors can lead to suboptimal outcomes.
Sameer Khan
January 5, 2026 AT 21:52From a pathophysiological standpoint, verapamil’s inhibition of L‑type calcium influx attenuates smooth muscle contractility, thereby reducing pulmonary arterial pressure in a subset of vasoreactive subjects. Nevertheless, the heterogeneity of endothelial dysfunction across the iPAH population limits its universal applicability. Future mechanistic studies should aim to delineate biomarkers predictive of responsiveness.
WILLIS jotrin
January 11, 2026 AT 16:45In the grand scheme, each therapeutic choice reflects a balance between efficacy, safety, and patient preference. Verapamil exemplifies how a classic cardiovascular agent can find a niche in modern pulmonary hypertension management.