When evaluating hormonal contraception safety, the process of reviewing risks, side‑effects, and health impacts of hormone‑based birth control methods. Also known as birth control safety, it helps patients and clinicians balance effectiveness with individual health concerns.
The most common category, combined oral contraceptive, contains both estrogen and progestin. Its key attribute is the estrogen dose, which influences clot‑formation risk, blood‑pressure changes, and migraine patterns. Women with a history of thrombosis or smoking over age 35 face higher odds of serious events, so careful screening is essential. This connection creates the triple: combined oral contraceptive requires estrogen dose monitoring.
Another major option is the progestin‑only pill, often called the mini‑pill. Its primary attribute is the lack of estrogen, which reduces clot risk but can cause irregular bleeding. Users need to take it at the same time each day; missed doses quickly reduce effectiveness. This leads to the triple: progestin‑only pill influences bleeding patterns, and adherence affects contraceptive efficacy.
A longer‑acting alternative is the hormonal intrauterine device. Its attributes include a steady low‑dose release of levonorgestrel and a lifespan of three to five years. Benefits are high efficacy and reduced user error, while side effects may include spotting and rare perforation. The device demonstrates the triple: hormonal IUD provides continuous contraception, and local hormone release limits systemic side‑effects.
Beyond the product type, demographics shape safety profiles. Younger women, those with obesity, or individuals with migraine with aura have distinct risk matrices. For example, migraine with aura combined with estrogen‑containing pills increases stroke probability, prompting clinicians to favor progestin‑only or non‑hormonal options. This illustrates the triple: patient characteristics affect method suitability.
Guidelines from major health organizations recommend a stepwise assessment: review medical history, evaluate contraindications (like uncontrolled hypertension or clotting disorders), discuss lifestyle factors, and then match the safest method. Regular follow‑up appointments allow monitoring of blood pressure, lipid changes, and any emerging side effects. The relationship here is: clinical guidelines guide risk assessment, which supports informed choice.
Understanding hormonal contraception safety means looking at hormone type, dosage, delivery system, and personal health factors—all together shaping the risk‑benefit balance. Below you’ll find a curated collection of articles that break down each method, compare side‑effects, and offer practical tips for making the right decision for your life.
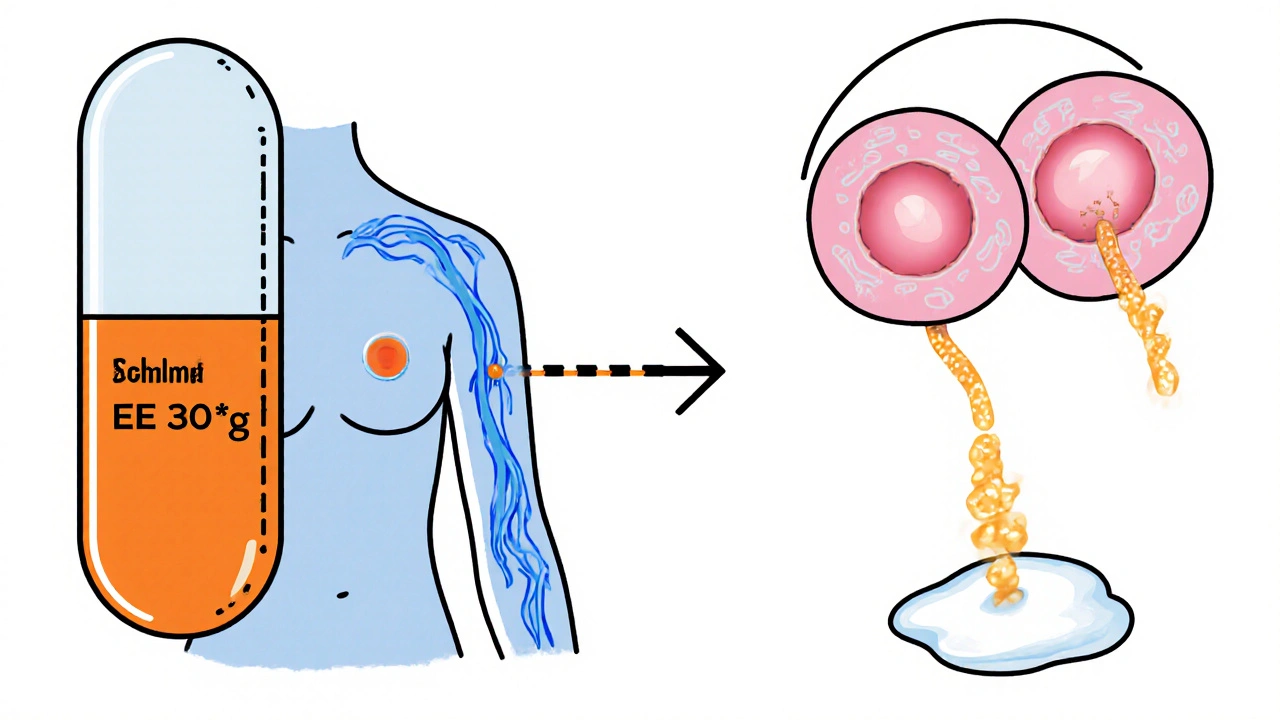
Learn how ethinylestradiol in birth‑control pills affects breastfeeding, safe start times, infant exposure, and alternative contraceptive options for nursing moms.