When you hear generic medication comparison, the process of evaluating whether a non-brand drug performs the same as its brand-name counterpart. Also known as drug substitution analysis, it's not just about saving money—it's about making sure your treatment stays safe and effective. Millions of people switch to generics every year because they cost less, but not all generics are created equal. Some work perfectly. Others need extra care, especially if you’re taking drugs where even a tiny change in blood levels can cause problems.
This is where bioequivalence studies, rigorous tests that measure how fast and how much of a drug enters your bloodstream. Also known as pharmacokinetic testing, these studies are the foundation of generic drug approval come in. The FDA requires these tests to prove a generic matches the brand in how your body absorbs and uses it. But here’s the catch: some drugs, like NTI drugs, narrow therapeutic index medications where the difference between a helpful dose and a dangerous one is very small. Also known as narrow window drugs, examples include warfarin, levothyroxine, and certain seizure meds, don’t always play nice with substitutions. Even if a generic passes the standard tests, your doctor might still recommend therapeutic drug monitoring, regular blood tests to check drug levels and avoid toxicity or treatment failure. Also known as TDM, this is a safety net for high-risk meds. It’s not about distrust—it’s about precision.
Why does this matter to you? Because switching from a brand to a generic isn’t just a price change—it’s a change in your treatment. Some people notice a difference in side effects, energy, or symptom control. That doesn’t mean the generic is bad. It might mean your body is sensitive, or your condition needs tighter control. That’s why knowing which drugs are safe to swap and which need watchful eyes makes all the difference. You’ll find real-world examples below: how lisinopril stacks up against other blood pressure pills, why Exelon and donepezil behave differently in dementia patients, and how fluoroquinolones can turn dangerous when mixed with common painkillers. These aren’t theoretical debates. They’re stories from people managing chronic conditions, dealing with side effects, or trying to cut costs without risking health. What you’ll see here isn’t marketing. It’s what happens when real patients and real science meet.
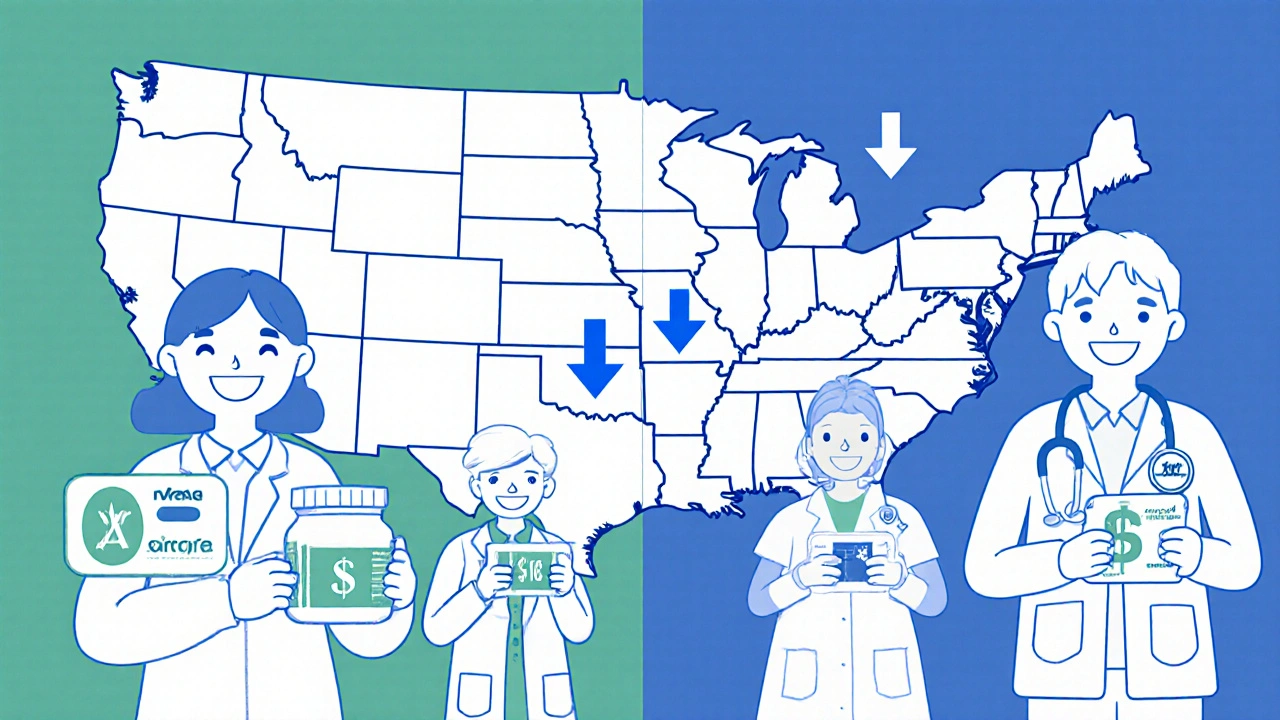
U.S. generic drug prices are 33% lower than in other wealthy countries, but brand-name drugs cost up to five times more. Here's how global pricing works - and what it means for your prescriptions.