When esophageal thrush, a fungal infection in the esophagus caused by Candida yeast. Also known as candida esophagitis, it isn’t just a sore throat—it’s a sign your body’s balance is off. This isn’t the same as the white patches you might see on your tongue (oral thrush), though they often come together. Esophageal thrush digs deeper, lining your food pipe with a fuzzy, inflamed coating that makes swallowing painful, sometimes even impossible. It doesn’t just happen to people with weak immune systems—it can sneak up after antibiotics, steroids, or even long-term acid reflux.
Most cases are tied to Candida albicans, the most common type of yeast that causes fungal infections in humans. But what makes it turn from harmless resident to problem child? When your immune system is down—due to HIV, chemotherapy, diabetes, or even chronic stress—it loses control. People on long-term inhaled steroids for asthma or COPD are also at higher risk, because the medication can linger in the throat and create a perfect breeding ground. And if you’ve been on antibiotics recently, you’ve likely wiped out the good bacteria that normally keep yeast in check. It’s not rare, but it’s often missed because symptoms mimic heartburn or a cold.
Left untreated, esophageal thrush doesn’t just hurt—it can spread. It might move into your stomach or lungs, especially if you’re immunocompromised. That’s why it’s not something to wait out. Treatment usually starts with antifungal pills like fluconazole, which work fast and well for most people. But if it comes back, or if you’re resistant to common drugs, doctors might switch to stronger options like itraconazole or nystatin swish-and-swallow. It’s not just about killing the fungus, though. You also need to fix what let it grow in the first place. That means managing blood sugar, reducing steroid use if possible, or switching to a spacer with your inhaler to keep the medicine out of your throat.
There’s no magic diet to cure it, but cutting back on sugar and refined carbs helps. Probiotics don’t replace meds, but they can support your gut’s natural defenses. And if you’re using mouthwashes or sprays with alcohol, stop—they dry out your mouth and make yeast thrive. This isn’t a one-size-fits-all issue. What works for a healthy 30-year-old might not help someone on immunosuppressants after a transplant. That’s why the best answers come from matching treatment to your specific health picture.
Below, you’ll find real-world guides on antifungal drugs, how they interact with other medications, and what to watch for when your body’s defenses are low. These aren’t generic advice pieces—they’re detailed comparisons and safety checks from people who’ve been there, and doctors who’ve treated them. Whether you’re dealing with recurring thrush, managing a chronic condition, or just want to understand why this keeps coming back, you’ll find clear, no-fluff answers here.
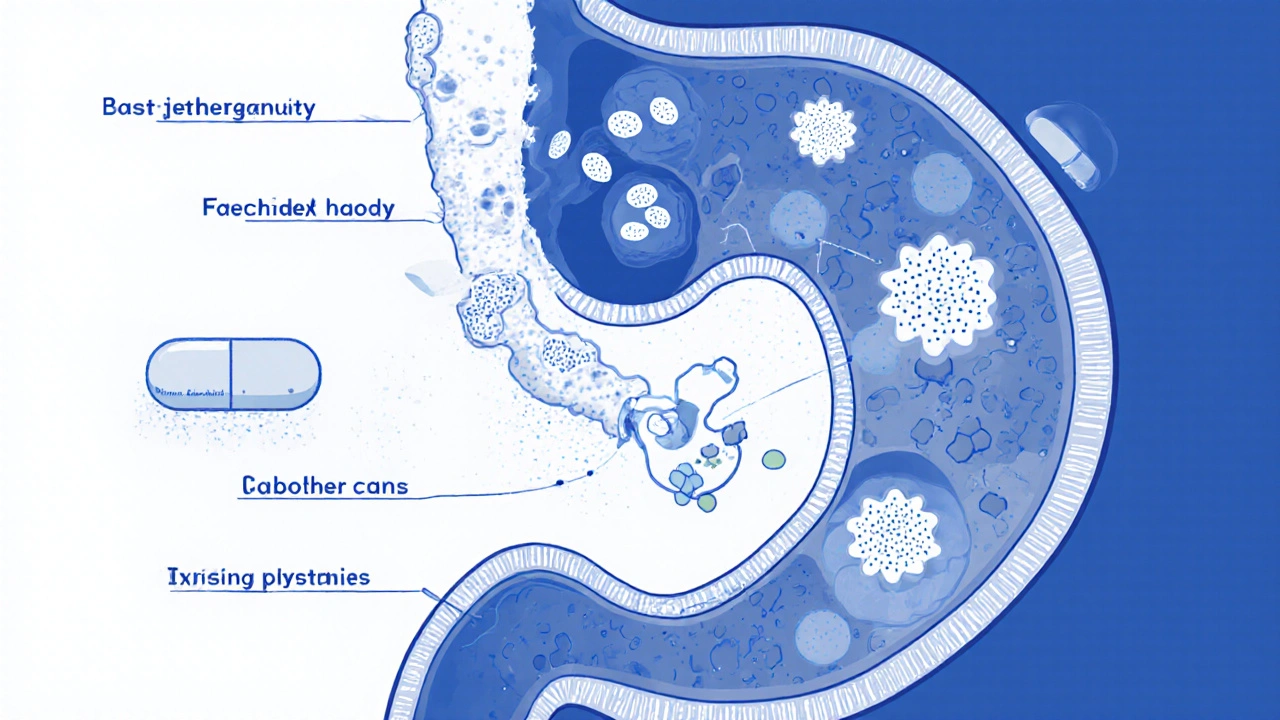
Fluconazole is the standard treatment for candida esophagitis, especially in immunocompromised patients. Learn how it works, proper dosing, what to expect, and how to prevent recurrence.