When you’re on a long-term medication like warfarin or a direct oral anticoagulant (DOAC) and need surgery or a procedure, you can’t just stop it cold. That’s where bridging therapy, a temporary treatment used to maintain protection against blood clots when a long-term anticoagulant is paused. Also known as anticoagulant bridge, it’s a critical safety step for people at high risk of clots during treatment gaps. This isn’t just about swapping one pill for another—it’s about timing, risk levels, and knowing exactly when to start and stop each drug. Think of it like switching lanes on a highway: you don’t just cut off your current speed. You ease in, match the flow, and avoid a crash.
Bridging therapy most often involves injections like heparin or low molecular weight heparin (LMWH), given daily or twice daily, to fill the gap while your main blood thinner is paused. It’s not for everyone. People with mechanical heart valves, recent clots, or certain types of atrial fibrillation are the most common candidates. But studies show that for many, the risks of bleeding from bridging can outweigh the benefits. That’s why doctors now use tools like the CHA₂DS₂-VASc score to decide who truly needs it. This decision ties directly into medication adherence, how consistently patients follow their prescribed treatment plan. If you miss a bridge injection or restart your main drug too early, you’re at risk. That’s why clear instructions and documentation—like those covered in posts about safety alerts, official warnings about drug risks that must be tracked on medication lists—are so vital.
It’s also connected to drug interactions, when one medication changes how another works in your body. For example, if you’re on an antibiotic that affects how your liver breaks down warfarin, your bridge dose might need adjusting. Or if you’re taking a painkiller that increases bleeding risk, your doctor has to weigh that against the clot danger. These aren’t theoretical concerns—they show up in real patient stories, like those in posts about lisinopril-HCTZ combinations or levodopa-antipsychotic conflicts. Bridging therapy sits at the intersection of these issues: it’s a temporary fix that demands precision, communication, and awareness of your full medication history.
What you’ll find below are practical guides that connect directly to this topic. From how to document safety alerts on your medication list, to handling missed doses without doubling up, to understanding how generic drugs behave differently in your body—each post gives you tools to navigate these transitions safely. Whether you’re a patient preparing for surgery, a caregiver managing meds at home, or a healthcare worker updating protocols, the information here is meant to reduce guesswork and prevent avoidable errors.
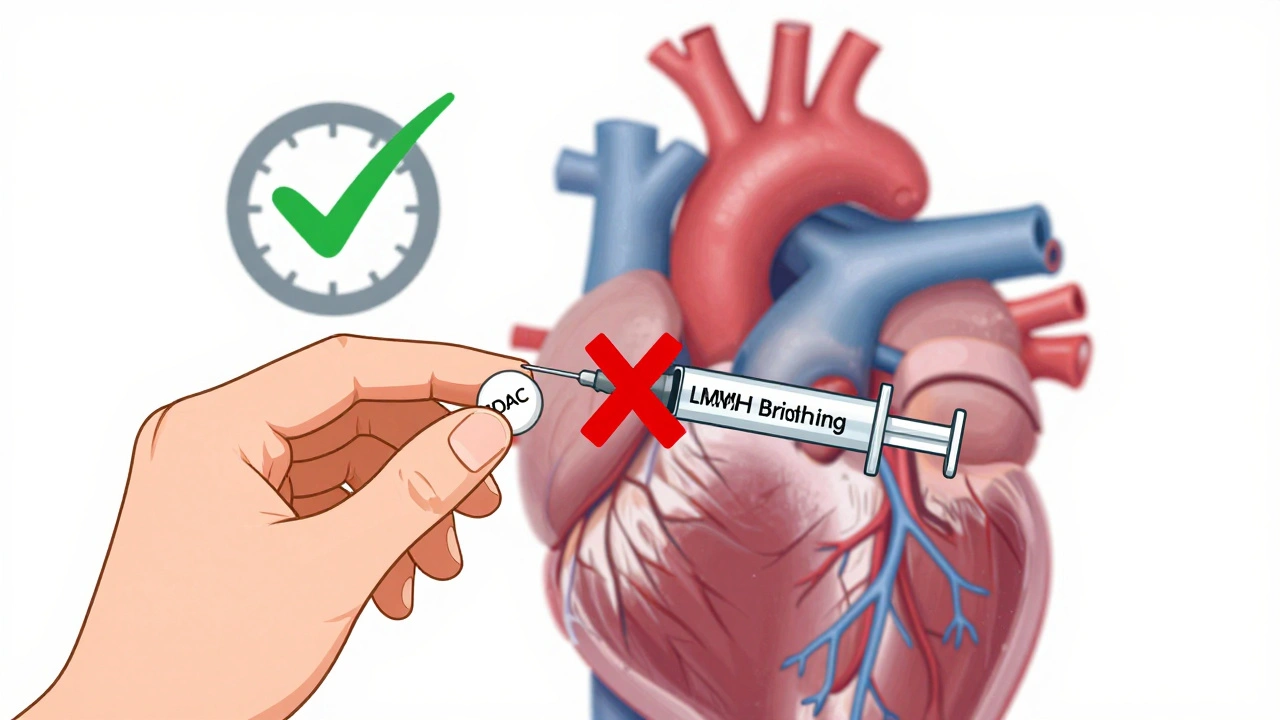
Learn when bridging therapy is truly needed when switching between blood thinners. Most patients don’t require it anymore - especially those on DOACs. Discover the latest guidelines, risks, and safe protocols for warfarin and newer anticoagulants.