When dealing with Bladder Spasms, involuntary contractions of the bladder wall that cause sudden urges to urinate. Also known as bladder contractions, they can interrupt daily life and often signal an underlying urinary issue.
One of the most common companions of bladder spasms is Overactive Bladder, a condition marked by frequent urges, nighttime trips, and occasional leakage. Overactive bladder encompasses symptoms like urinary urgency, increased frequency, and nocturia, all of which can be driven by the same muscle hyper‑activity that creates spasms. Another key player is Anticholinergic Medication, drugs that relax the bladder muscle by blocking acetylcholine signals. These meds often appear in treatment discussions because they directly target the nerve signals causing the spasms. Finally, Pelvic Floor Therapy, a set of exercises and manual techniques designed to strengthen the muscles supporting the bladder works hand‑in‑hand with medication, helping patients gain better control over involuntary contractions.
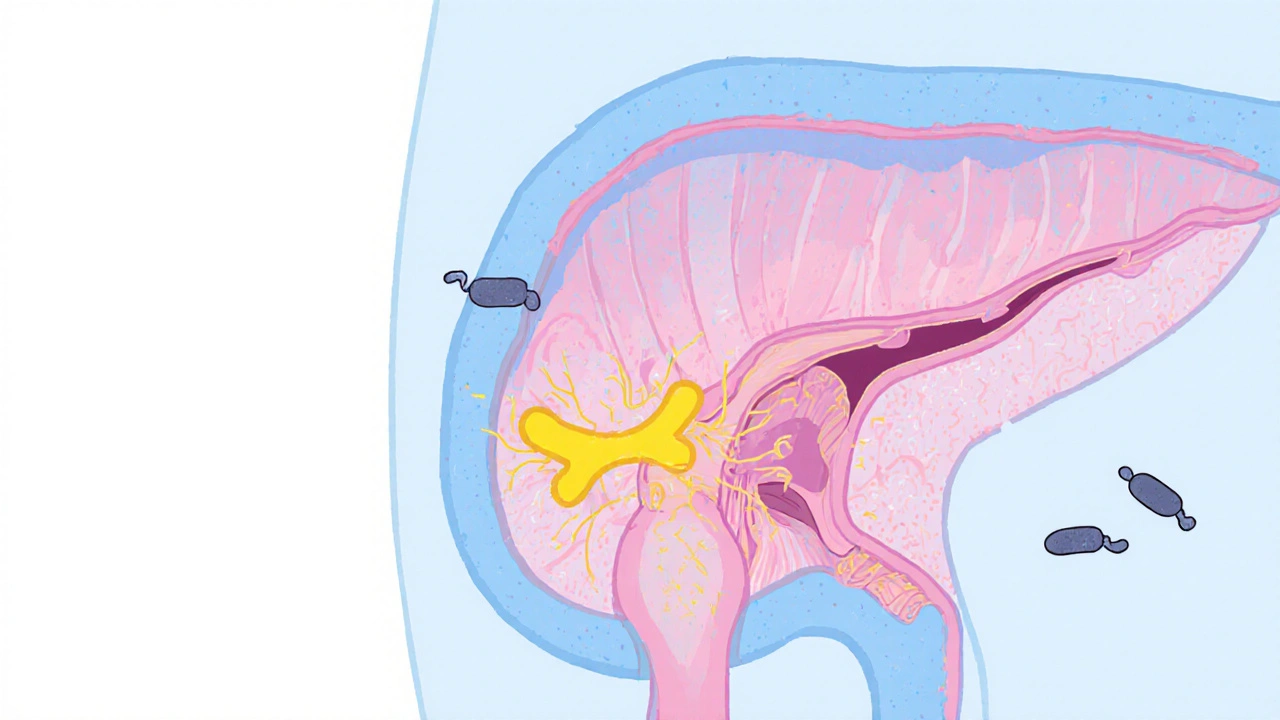
Bladder spasms require a clear diagnosis to avoid mistaking them for infections or stones. Doctors typically start with a symptom checklist: sudden urgency, a feeling of incomplete emptying, and occasional dribbling. A simple urine test rules out infection, while an ultrasound can spot structural problems. If those are clear, the focus shifts to the muscle itself—this is where the link to overactive bladder becomes crucial. Understanding that overactive bladder influences the frequency and intensity of spasms helps clinicians choose the right treatment path.
Medication guides on our site, such as the comparison of Phenazopyridine (often used for urinary pain) and common diuretics like Furosemide, illustrate how different drugs affect bladder dynamics. Phenazopyridine eases discomfort without altering muscle tone, whereas diuretics can increase urine volume and sometimes trigger more spasms if not managed correctly. By looking at these drug profiles, readers can see which options might calm the bladder or, unintentionally, make it twitchier.
Beyond pills, lifestyle tweaks play a big role. Reducing caffeine, staying hydrated but not over‑hydrated, and timing bathroom visits can lower the chances of a sudden spasm. For many, pelvic floor therapy enables better muscle coordination, decreasing the reflex that leads to spasms. Physical therapists often combine biofeedback with targeted exercises, teaching patients to recognize and halt an impending contraction before it erupts.
When a spasm episode does happen, quick relief options exist. Over‑the‑counter analgesics like Pyridium (phenazopyridine) can soothe burning, while a warm sit‑z bath may relax the bladder wall. If spasms are frequent, a doctor may prescribe anticholinergic drugs such as oxybutynin or revise an existing regimen, perhaps swapping a weaker agent for a newer, more bladder‑specific option.
Our collection below pulls together detailed drug comparisons, dosage guides, and practical tips that fit right into this treatment puzzle. Whether you’re curious about the pros and cons of a specific medication, need a side‑by‑side look at diuretics, or want to explore non‑drug approaches like pelvic floor therapy, the articles ahead give you the facts you need to make an informed decision.
Ready to dive deeper? Browse the posts below to see how each medication or therapy option relates to bladder spasms, and find actionable advice you can start using today.
Explore whether flavoxate can lower urinary tract infection rates, its mechanism, evidence, safety, and practical tips for using it alongside proven prevention methods.