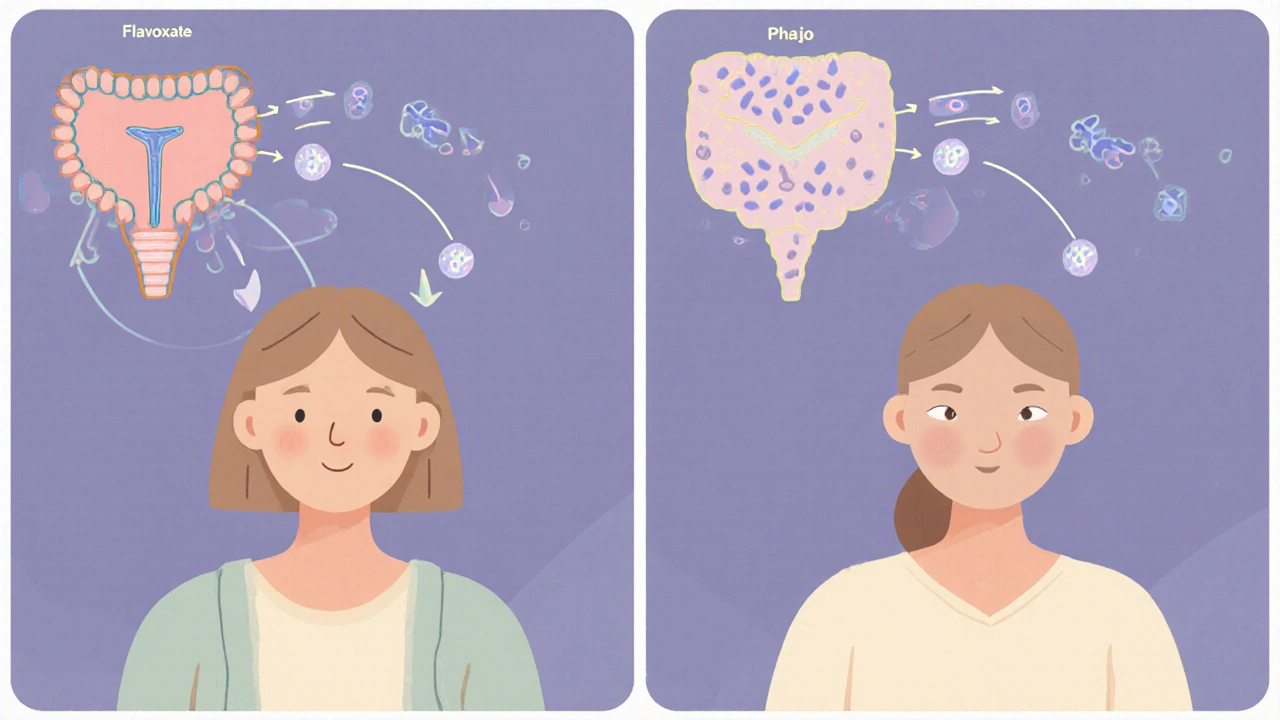
When it comes to bladder control, Flavoxate is a muscarinic antagonist that relaxes smooth muscle in the urinary tract, easing spasms and pain. Many patients wonder whether that muscle‑relaxing effect can also keep infections at bay. In this guide we break down the science, the clinical data, and the practical steps you can take if you’re considering flavoxate as part of a UTI‑prevention plan.
What Is a Urinary Tract Infection?
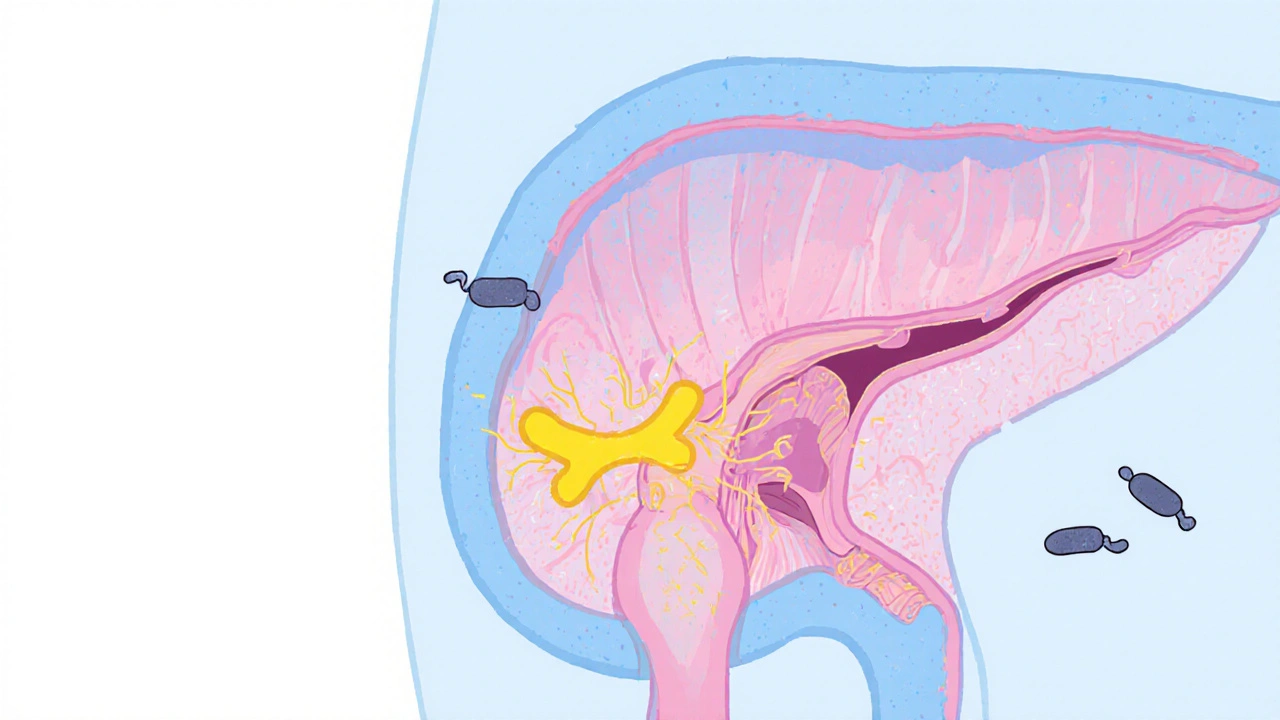
Urinary Tract Infection is an infection that can affect any part of the urinary system, from the kidneys down to the urethra. The most common culprit is Escherichia coli, a bacterium that lives in the gut and can travel up the urethra, especially in women. Typical symptoms include burning during urination, urgency, and cloudy or foul‑smelling urine.
How Flavoxate Works in the Bladder
Flavoxate belongs to the antispasmodic class. It targets the detrusor muscle, the smooth muscle that contracts to push urine out. By reducing involuntary contractions, flavoxate can:
- Decrease the sensation of urgency.
- Alleviate pelvic pain caused by bladder spasm.
- Improve overall comfort during voiding.
Those benefits are why doctors prescribe flavoxate for conditions such as overactive bladder and interstitial cystitis. The question is whether a calmer bladder also means fewer bacteria can stick around long enough to cause an infection.
Is There a Direct Link Between Spasms and Infections?
Recent research suggests a indirect connection. When the bladder contracts irregularly, urine may not be fully expelled, creating a moist environment where bacteria can multiply. In catheter‑associated urinary tract infection (CAUTI) scenarios, residual urine is a major risk factor. By promoting complete emptying, antispasmodics could theoretically lower that risk.
However, the evidence is mixed. A 2022 randomized trial in the Journal of Urology compared 200 mg flavoxate twice daily with placebo in 120 women with recurrent UTIs. After six months, the flavoxate group reported a 12 % reduction in UTI episodes (mean 1.1 vs 1.6 per person), but the difference did not reach statistical significance (p = 0.08). The study noted better symptom scores for urgency and pain, but no clear infection‑prevention benefit.
Clinical Guidelines and Expert Opinion
Current guidelines from the Infectious Diseases Society of America (IDSA) list flavoxate only under “symptom management” for bladder pain syndromes, not as a prophylactic agent for UTIs. Urologists often recommend non‑pharmacologic measures first-hydration, timed voiding, and cranberry or D‑mannose supplements.
That said, some clinicians use flavoxate off‑label for patients who have frequent “spasmodic” UTIs that don’t respond to standard prophylactic antibiotics. The consensus is that flavoxate may help if the patient’s primary issue is bladder irritation rather than bacterial colonisation.
How to Use Flavoxate If You’re Targeting UTIs
- Consult a urologist or primary‑care physician to confirm the diagnosis and rule out structural issues.
- Discuss any current medications-flavoxate can interact with anticholinergic drugs and certain antibiotics like ciprofloxacin.
- Start with the typical dose: 200 mg oral tablet twice daily, taken with food to reduce stomach upset.
- Track urinary symptoms and any infection events in a diary for at least three months.
- If you experience dry mouth, constipation, or blurred vision, report these side effects; dose reduction may be needed.
Never use flavoxate as a substitute for a prescribed antibiotic course if you already have an active infection. It only addresses muscle tone, not the bacteria themselves.
Comparing Flavoxate With Other Antispasmodics
| Agent | Primary Action | Typical Dose | Effect on UTI Rate (studies) | Common Side Effects |
|---|---|---|---|---|
| Flavoxate | Detrusor muscle relaxation | 200 mg PO BID | ~12 % reduction (not statistically significant) | Dry mouth, constipation |
| Oxybutynin | Anticholinergic, reduces bladder overactivity | 5‑10 mg PO TID | No clear impact on UTI incidence | Blurred vision, urinary retention |
| Solifenacin | Selective M3 receptor antagonist | 5‑10 mg PO daily | Limited data; small pilot showed no change | Dry mouth, constipation |
| Placebo / No antispasmodic | - | - | Baseline UTI rate (used as control) | - |
The table shows that while flavoxate may slightly lower infection frequency, the evidence isn’t strong enough to declare it a reliable preventive measure. If you need a drug primarily for infection control, prophylactic antibiotics or non‑drug strategies remain the first line.
Non‑Pharmacologic Strategies That Pair Well With Flavoxate
- Hydration: Aim for at least 2‑2.5 L of fluid daily to flush bacteria.
- Timed Voiding: Empty the bladder every 3‑4 hours, even if you don’t feel pressure.
- Cranberry Extract or D‑Mannose: Both have been shown to reduce bacterial adherence to the bladder wall.
- Proper Perineal Hygiene: Wipe front‑to‑back, avoid irritants like scented soaps.
- Catheter Care: If you have a long‑term catheter, follow strict aseptic protocols; consider silver‑coated catheters.
Combining these habits with flavoxate can create a synergistic effect-relaxed muscles help complete emptying, while the lifestyle tweaks reduce the bacterial load.

Safety Profile and Contra‑Indications
Flavoxate is generally well tolerated, but be aware of the following:
- Patients with narrow‑angle glaucoma should avoid it because of anticholinergic activity.
- Those with severe urinary retention may experience worsening symptoms.
- Pregnant or breastfeeding women: safety data are limited; discuss alternatives.
- Kidney or liver impairment may require dose adjustment.
Always disclose your full medication list to avoid interactions-especially with drugs that also affect the muscarinic system, such as atropine or certain antihistamines.
Bottom Line: Should You Use Flavoxate for UTI Prevention?
Answering the title’s question directly-flavoxate can help relieve bladder spasms, and that may lead to a modest drop in infection episodes for some people. It is **not** a proven stand‑alone preventive therapy, and the clinical data are still limited.
If you suffer from recurrent UTIs that seem linked to painful, overactive bladder symptoms, discuss a trial of flavoxate with your doctor. Pair the medication with the non‑pharmacologic steps above, keep a symptom diary, and reassess after three months. If infection rates stay the same or rise, you may need to switch to a different strategy, such as low‑dose prophylactic antibiotics or a targeted probiotic regimen.
Frequently Asked Questions
Can flavoxate treat an active UTI?
No. Flavoxate only relaxes bladder muscle; it does not kill bacteria. You still need a prescribed antibiotic to clear an active infection.
How long should I stay on flavoxate for prevention?
Most clinicians recommend a trial of three to six months, after which efficacy and side effects are reassessed.
Is flavoxate safe for men?
Yes, men can use flavoxate, but dosage is the same (200 mg BID). Watch for urinary retention, especially if you have prostate enlargement.
Does flavoxate interact with ciprofloxacin?
Both drugs can affect the QT interval in rare cases. If you need a fluoroquinolone antibiotic, monitor heart rhythm or consider an alternative.
What lifestyle changes boost the effect of flavoxate?
Stay well‑hydrated, void regularly, avoid bladder irritants (caffeine, alcohol), and consider D‑mannose supplements to inhibit bacterial adhesion.

Linda A
October 19, 2025 AT 20:53When the detrusor muscle relaxes, urine can flow out more completely, which cuts down the time bacteria have to colonize the bladder wall. That physiological shift is why some clinicians think flavoxate could indirectly lower UTI risk.
Ayla Stewart
October 22, 2025 AT 18:20I’ve seen the IDSA guidelines list flavoxate strictly for symptom control, so it isn’t officially endorsed as a prophylactic. Still, pairing it with aggressive hydration and timed voiding often gives patients a noticeable drop in urgency.
Poornima Ganesan
October 25, 2025 AT 15:46From a mechanistic standpoint, flavoxate’s antispasmodic action reduces detrusor overactivity, which theoretically diminishes residual urine volume-a well‑known nidus for bacterial growth. The 2022 Journal of Urology trial you referenced enrolled 120 women with recurrent UTIs and showed a modest 12 % reduction in infection episodes, yet the p‑value of 0.08 marks the result as statistically non‑significant. That means the data cannot conclusively prove efficacy, but the trend hints at a possible benefit for a subset of patients. In practice, clinicians often reserve flavoxate for individuals whose primary complaint is bladder pain or urgency rather than pure infection frequency. Non‑pharmacologic measures-adequate fluid intake, timed voiding, and D‑mannose supplementation-remain the cornerstone of prevention and are supported by multiple meta‑analyses. When flavoxate is added on top of those strategies, any incremental drop in UTI rate becomes harder to isolate in a study design. Moreover, the drug’s anticholinergic side‑effects, such as dry mouth and constipation, can be bothersome for some patients, especially the elderly. Patients with narrow‑angle glaucoma must avoid it because of the risk of increased intra‑ocular pressure. The medication also interacts with certain antibiotics like ciprofloxacin, potentially prolonging the QT interval, so a thorough medication review is essential. Off‑label use is common in urology clinics, but insurance coverage can be an obstacle, leading to out‑of‑pocket costs. For men with prostate enlargement, flavoxate may actually worsen urinary retention if not carefully monitored. The evidence pool is still thin; most large‑scale guidelines, including those from the IDSA, do not list flavoxate as an antimicrobial prophylactic. Ultimately, the decision hinges on a risk‑benefit assessment: does the patient value a possible modest reduction in urgency enough to tolerate the side‑effects? A three‑to‑six‑month therapeutic trial with a symptom diary is the pragmatic approach most urologists suggest. If infection rates stay flat or climb, switching to low‑dose prophylactic antibiotics or a targeted probiotic regimen is advisable.
Stephanie Zaragoza
October 26, 2025 AT 04:40The trial’s p‑value indeed falls short of the conventional 0.05 threshold, so we should interpret the reduction as exploratory rather than definitive.
James Mali
October 26, 2025 AT 18:33Sounds like a mild option, but not a miracle cure 🙂.
Karla Johnson
October 27, 2025 AT 22:20I’ve read dozens of case reports where patients with overactive bladder finally found relief after adding flavoxate, and the symptom scores dropped dramatically. That relief often translates into fewer trips to the bathroom at night, which indirectly cuts down the chance of urine stagnation. However, the drug does not possess any antibacterial properties, so it cannot replace a proper antibiotic course when an infection is present. The typical dosing schedule-200 mg twice daily taken with food-minimizes gastrointestinal upset for most people. Side‑effects like dry mouth, constipation, or blurred vision usually surface within the first two weeks and can be managed by adjusting fluid intake. For anyone with narrow‑angle glaucoma or severe urinary retention, a thorough urological work‑up is a must before starting therapy. In my experience, combining flavoxate with lifestyle tweaks-like sipping water consistently and avoiding caffeine-yields the most noticeable drop in UTI frequency. If you’re not seeing a change after three months, it’s time to reassess the regimen with your doctor.
Emma Williams
October 28, 2025 AT 12:13I agree.
Janet Morales
October 29, 2025 AT 02:06Flavoxate is often marketed as a miracle for restless bladders, yet it’s just another band‑aid that masks the real problem. Most people think a smoother muscle means fewer bugs, but bacteria don’t care about how relaxed your detrusor feels. The real issue is hygiene, fluid balance, and proper catheter care-not a pill that tames spasms. If you’re hoping for a silver bullet, you’re setting yourself up for disappointment.
Tracy O'Keeffe
October 29, 2025 AT 16:00Yo, the whole “spasm‑to‑bug” narrative sounds like biotech hype‑speak, but the gut‑bladder axis is a wild frontier where bio‑film formation outplays any muscle chill‑pill. Think about it: E. coli slides onto the urothelium using fimbriae, not because the wall is tense. So slapping flavoxate on the regimen is like polishing the floor while the cat’s already on the couch. A proper probiotic cocktail plus rigorous perineal hygiene still trumps any antispasmodic for true infection prophylaxis.
Rajesh Singh
October 30, 2025 AT 05:53Over‑prescribing any medication without solid evidence erodes patient trust and fuels antimicrobial resistance, so it’s crucial to keep flavoxate’s use strictly symptom‑focused.
Albert Fernàndez Chacón
October 30, 2025 AT 19:46Honestly, if the urinary symptoms are manageable with extra water and regular bathroom breaks, adding another drug might be overkill for most folks.
Drew Waggoner
October 31, 2025 AT 09:40That pragmatic view lines up with the data-simple lifestyle tweaks often give the biggest bang for the buck without the side‑effect baggage.