When dealing with balance issues, a feeling of unsteadiness or difficulty staying upright that can stem from many health conditions. Also known as balance problems, it often signals an underlying problem that needs attention. Dizziness, a sensation of light‑headedness or spinning that can accompany balance problems and Vertigo, a specific type of dizziness where the environment feels like it’s moving are frequent companions. Both can arise from inner ear disorders, conditions affecting the vestibular system such as Ménière’s disease or vestibular neuritis. In addition, medication side effects, adverse reactions to drugs that can impair proprioception or inner‑ear function are a leading but often overlooked trigger.
Why does this matter? Understanding the web of causes helps you pinpoint the right treatment. For example, if a new prescription is causing medication side effects, a simple dosage adjustment may restore stability. If inner ear disorders are the culprit, vestibular rehabilitation exercises and specific medications can reduce the spinning sensation of vertigo. Recognizing the subtle difference between general dizziness and true vertigo often determines whether a patient needs a ENT specialist or a neurologist.
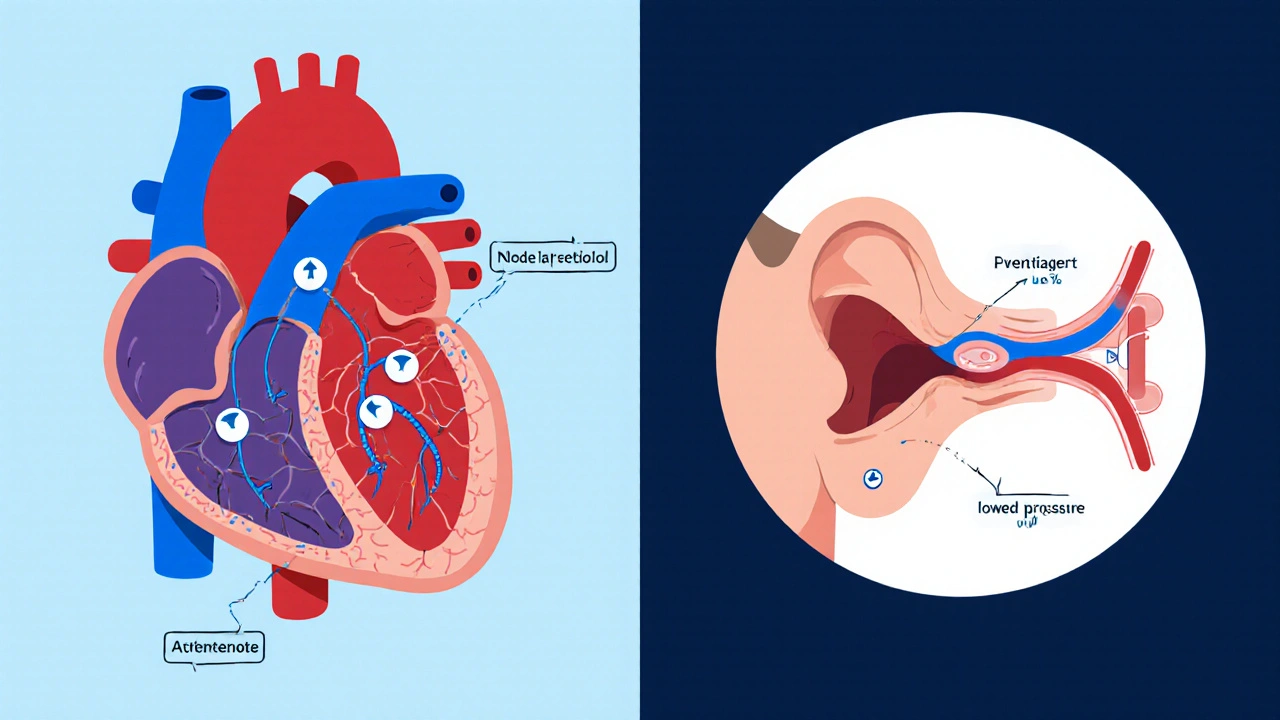
First, the vestibular system—tiny structures in the inner ear—acts as the body’s gyroscope. When these structures are inflamed or filled with excess fluid, the brain receives mismatched signals, leading to balance issues. Second, the central nervous system integrates input from vision and proprioception; diseases like diabetes or multiple sclerosis can disrupt this integration, making a person feel off‑balance even with normal ear function. Third, many common medications—antibiotics such as azithromycin, antihistamines like promethazine, and even blood pressure drugs like lisinopril—list side‑effects that include dizziness or impaired coordination.
Another layer involves age‑related changes. As we age, the hair cells in the inner ear degenerate, and muscle strength declines, both of which raise the risk of falls. Lifestyle factors matter too: dehydration, alcohol, and lack of sleep can all tip the balance scale. The good news is that you can often mitigate these risks with simple actions: staying hydrated, limiting alcohol, using assistive devices when needed, and reviewing any new prescriptions with a pharmacist.
When you suspect your balance issues are medication‑related, start by listing every drug you take—prescription, over‑the‑counter, and supplements. Look for known culprits such as antihistamines, certain antibiotics, and some blood pressure agents. A quick chat with your healthcare provider can uncover safer alternatives or dosage tweaks. If the problem feels more like sudden spinning, it’s likely vertigo from an inner‑ear disturbance, and specific tests like the Dix‑Hallpike maneuver can confirm the diagnosis.
Finally, managing balance problems isn’t just about fixing the cause. Rehabilitation programs that combine balance training, eye‑movement exercises, and strength building are proven to reduce fall risk by up to 40 % in older adults. Physical therapists can tailor a plan that targets your specific deficits, whether they stem from inner ear dysfunction or systemic issues. In many cases, a multidisciplinary approach—doctor, pharmacist, therapist—delivers the best outcomes.
Below you’ll find a curated collection of articles that dive deeper into individual factors linked to balance issues. From how specific antibiotics may tip your equilibrium to practical tips on choosing safer antihistamines, these resources give you actionable insight to protect your stability and confidence.
Explore how atenolol can affect balance, why dizziness happens, who’s most at risk, and practical steps to stay safe while using the medication.