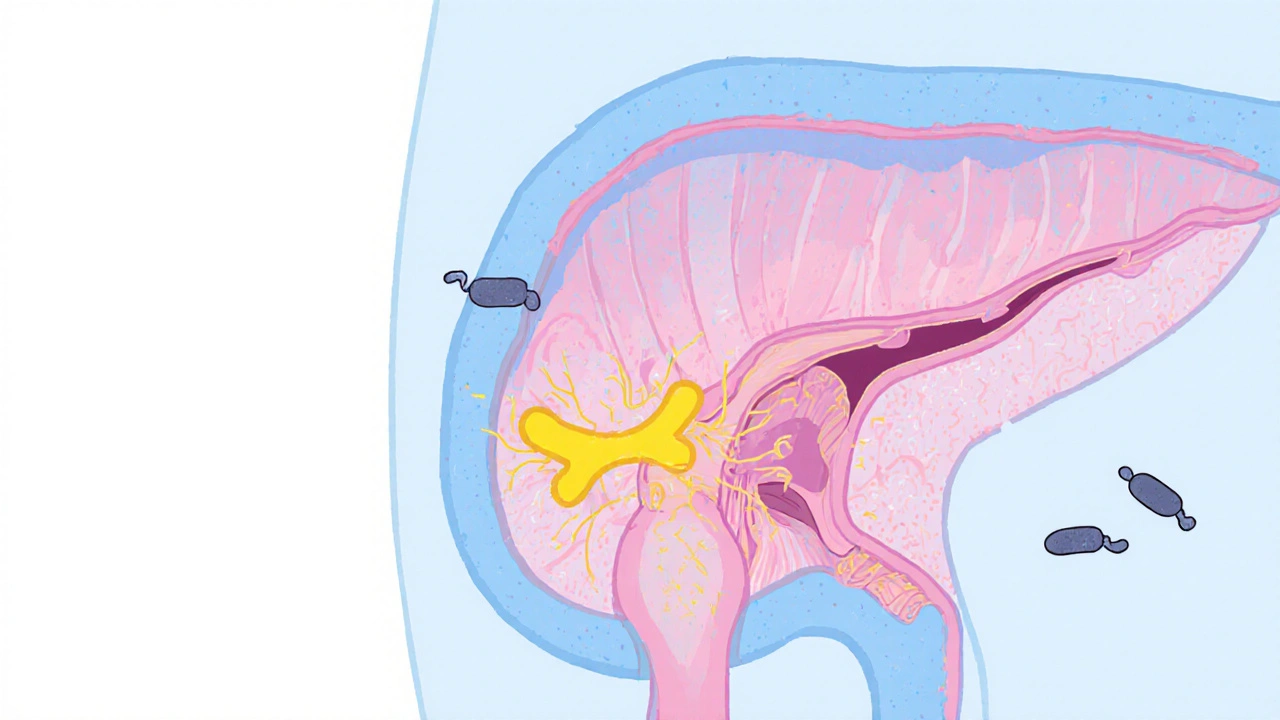
When dealing with involuntary muscle cramps, antispasmodic, a class of drugs that relax smooth muscle fibers in the gastrointestinal tract, urinary system, and other organs, also known as smooth muscle relaxant often become the go‑to option. These agents target the nerves or calcium channels that trigger spasm, helping the body return to a normal rhythm. Whether you’ve been prescribed one after a bout of IBS or are researching over‑the‑counter options, understanding the core idea behind antispasmodics saves you time and confusion.
Not all antispasmodics act the same way. Dicyclomine, an anticholinergic that blocks acetylcholine receptors in the gut is popular for ulcerative colitis and irritable bowel syndrome because it reduces both pain and cramping without strong sedation. In contrast, Hyoscine, also called scopolamine, works by inhibiting muscarinic receptors and is often used for motion‑sickness or bladder spasms. Then there are calcium‑channel blockers like Verapamil, which relaxes smooth muscle by limiting calcium influx, making it useful for certain esophageal spasms and even some types of hypertension. Each drug brings a distinct set of attributes—onset speed, side‑effect profile, and typical dosing—that match different clinical scenarios.
Here’s a quick snapshot of their core attributes:
Beyond the three highlighted, other agents like baclofen (a GABA‑B agonist) and mebeverine (a direct smooth‑muscle relaxant) expand the toolbox, especially for pelvic floor disorders or chronic abdominal pain. The common thread is they all aim to break the cycle of muscle contraction → pain → stress → more contraction.
When you combine an antispasmodic with lifestyle tweaks—fiber‑rich meals, regular exercise, stress‑management techniques—you often see a bigger payoff than medication alone. For instance, patients with functional dyspepsia who add a low‑dose antispasmodic to a high‑fiber diet report fewer post‑meal cramps and better overall comfort.
Safety is another pillar. Because many antispasmodics block acetylcholine, they can interact with antihistamines, antidepressants, or other anticholinergic drugs, raising the risk of constipation or blurred vision. Always flag existing meds to your prescriber. For older adults, start low and monitor for confusion or urinary retention—common red flags when the nervous system slows down.
Insurance coverage and cost also play a role. Generic dicyclomine and hyoscine are widely available at low prices, while brand‑name or IV‑only formulations of verapamil may cost more. Checking pharmacy price‑comparisons can shave dollars off a month‑long regimen.
From a prescribing standpoint, doctors often start with the least invasive option. That means an oral anticholinergic for mild IBS, moving to a calcium‑channel blocker if symptoms persist despite diet changes. If symptoms are linked to a specific organ—like the bladder—targeted agents such as oxybutynin (another anticholinergic) take priority.
Research continues to refine our toolbox. Recent small‑scale trials suggest that low‑dose mebeverine combined with probiotics cuts down on abdominal pain more effectively than either alone. Meanwhile, a 2023 meta‑analysis highlighted that hyoscine patches provide comparable relief to oral tablets for motion‑sickness with fewer systemic side effects.
What you take away from this is that antispasmodic therapy isn’t one‑size‑fits‑all. It hinges on the type of spasm, the patient’s overall health, and the balance between efficacy and tolerability. The next section of the site lists detailed comparisons of many of these drugs, from dosing charts to side‑effect breakdowns, so you can see exactly how they stack up.
Below you’ll find a curated collection of articles that dig into individual antispasmodic agents, compare them against alternatives, and offer practical guidance on when and how to use each one. Whether you’re a patient looking for clear answers or a clinician seeking up‑to‑date data, the posts ahead give you the factual backbone you need to make informed choices.
Explore whether flavoxate can lower urinary tract infection rates, its mechanism, evidence, safety, and practical tips for using it alongside proven prevention methods.