When someone hears voices, feels paranoid, or loses touch with reality, antipsychotics, a class of medications designed to reduce symptoms of psychosis. Also known as neuroleptics, these drugs help restore balance in brain chemistry—especially in conditions like schizophrenia and severe bipolar disorder. They don’t cure these illnesses, but they can make daily life possible again.
Not all antipsychotics are the same. Some, like risperidone, a second-generation antipsychotic commonly prescribed for schizophrenia and irritability in autism, are less likely to cause movement issues than older ones like haloperidol. Others, like clozapine, a powerful option for treatment-resistant psychosis, require regular blood tests because of rare but serious side effects. Then there are drugs like quetiapine, often used for bipolar depression and insomnia alongside psychosis, which carry sedation as a common trade-off. Each has its own profile—dosing, risks, and who it works best for.
Antipsychotics don’t work the same for everyone. Some people feel better within days. Others need weeks, or even months, to see results. And while many tolerate them well, side effects like weight gain, drowsiness, tremors, or metabolic changes can make people stop taking them. That’s why doctors often pair these meds with therapy, lifestyle changes, or other treatments to keep patients on track. You’ll also find posts here about how these drugs interact with other medications—like when antipsychotics clash with cold medicines or painkillers, raising risks of dangerous reactions. Some people even need therapeutic drug monitoring, a blood test to check levels and avoid toxicity, especially if they’re on generics or multiple meds.
There’s no one-size-fits-all approach. What works for one person might not work for another—and what helps today might need adjusting tomorrow. That’s why real-world experiences matter: how people manage side effects, what alternatives they tried, and when switching meds made all the difference. Below, you’ll find practical guides on comparing antipsychotics, understanding their risks, and learning how to use them safely alongside other treatments. No fluff. Just clear, tested info from people who’ve been there.
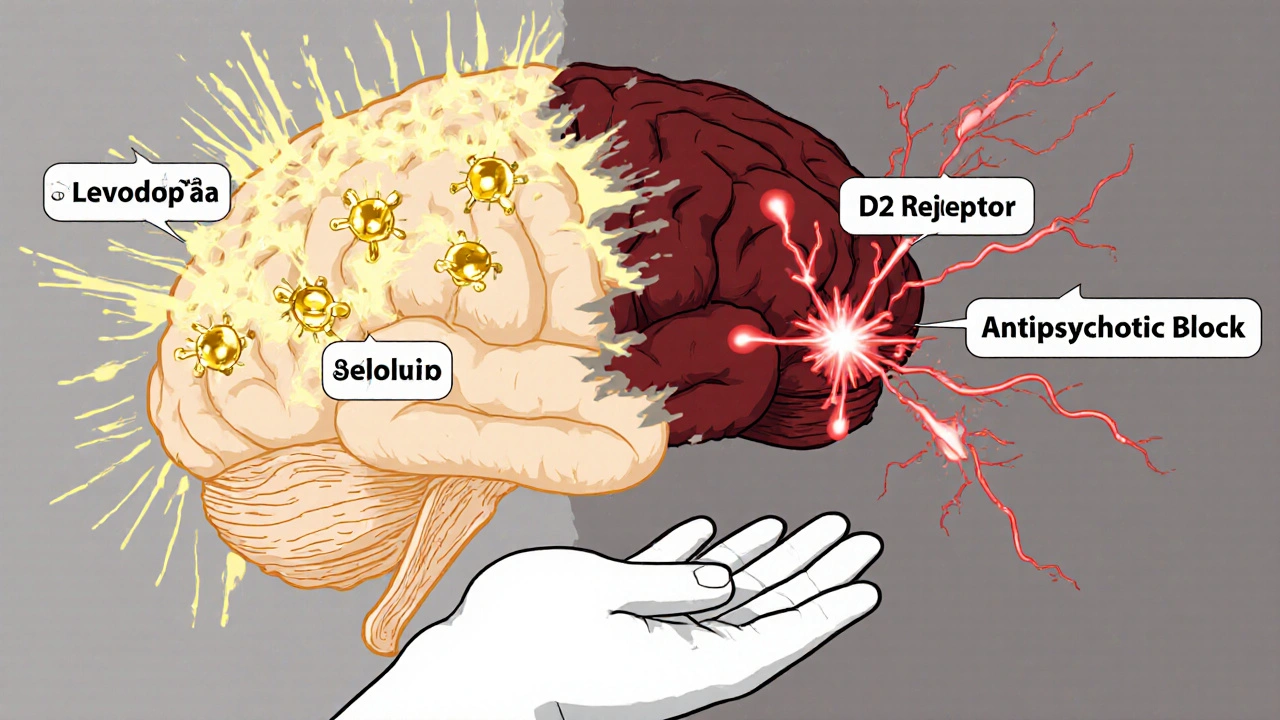
Levodopa and antipsychotics have opposing effects on dopamine, making it dangerous to use them together. This interaction can worsen Parkinson's symptoms or trigger psychosis, creating a difficult treatment dilemma for patients and doctors.