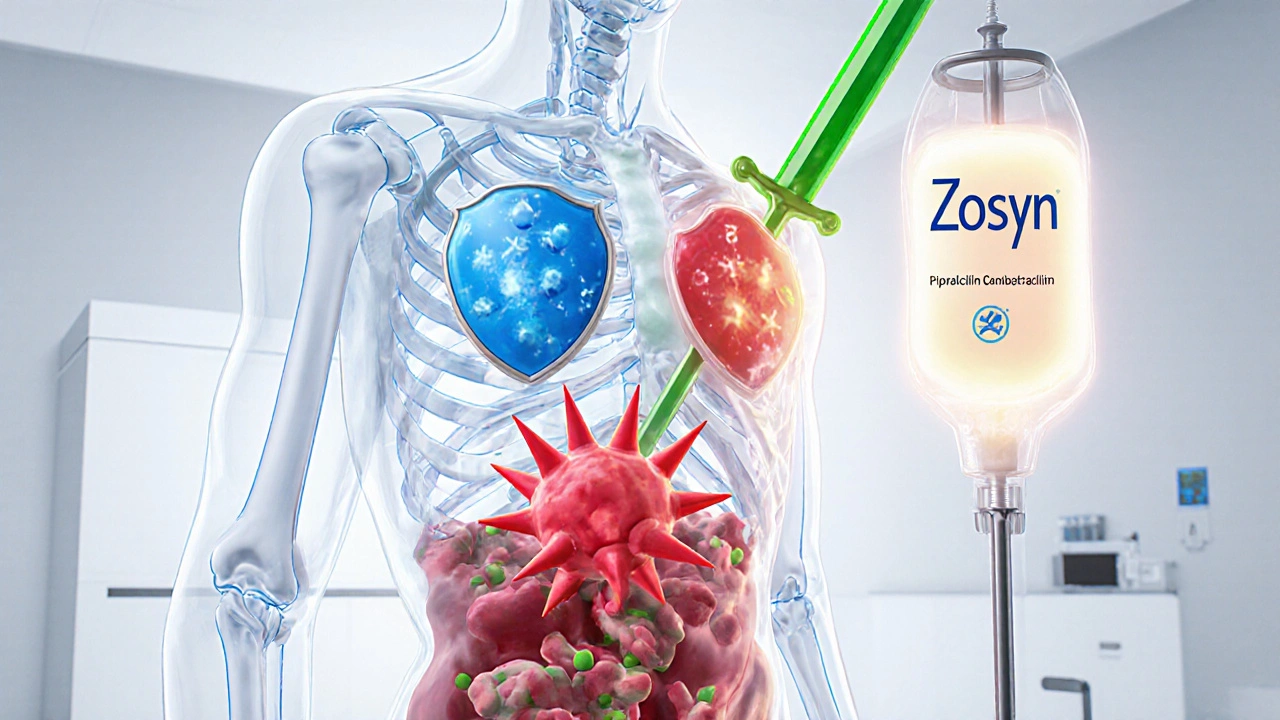
When a single antibiotic doesn’t cut it, doctors turn to antibiotic combination products, mixtures of two or more antibiotics designed to work together against stubborn infections. Also known as combination antibiotics, these drugs are often used for severe or resistant infections where bacteria have learned to dodge single-drug attacks. Think of it like using two different keys to unlock a door that one key can’t open anymore. These combinations aren’t random—they’re carefully chosen based on how each drug behaves in the body and how they boost each other’s power.
One common reason for using antibiotic combination products, mixtures of two or more antibiotics designed to work together against stubborn infections. Also known as combination antibiotics, these drugs are often used for severe or resistant infections where bacteria have learned to dodge single-drug attacks. is to prevent resistance. Bacteria evolve fast. If you use just one drug, the ones that survive can multiply and pass on their defenses. Add a second antibiotic that attacks in a different way, and you reduce the chance of survival. This is why you’ll often see combinations like amoxicillin-clavulanate or trimethoprim-sulfamethoxazole on prescriptions. They’re not just stronger—they’re smarter.
But it’s not all about power. Some combinations are used because one drug helps the other work better. For example, clavulanate doesn’t kill bacteria on its own, but it blocks the enzyme that breaks down amoxicillin. That’s why the combo lasts longer and works deeper. Other times, it’s about covering more ground—like using one drug for gram-positive bugs and another for gram-negative ones. This is common in hospital settings where the exact germ isn’t known yet. Still, these combos aren’t risk-free. Mixing antibiotics can increase side effects, especially on the kidneys or gut. And if used carelessly, they can fuel resistance even faster.
That’s why therapeutic drug monitoring, the process of measuring drug levels in the blood to ensure they’re in the safe and effective range. Also known as TDM, it’s especially important for narrow therapeutic index drugs like vancomycin or aminoglycosides when used in combo matters so much. Even small changes in blood levels can lead to toxicity or treatment failure. That’s why patients on these regimens often need regular blood tests. It’s not just about taking pills—it’s about knowing exactly how much is in your system.
And then there’s the issue of drug interactions, when one medication changes how another works in the body, sometimes dangerously. Also known as medication interactions, they can turn a helpful combo into a harmful one. For instance, combining certain antibiotics with NSAIDs like ibuprofen can spike the risk of kidney damage or nerve problems. You can’t just throw drugs together and hope for the best. Every combo has a reason—and every reason needs to be weighed against the risks.
What you’ll find in the posts below are real examples of how these combinations are used, when they backfire, and how patients and doctors navigate the fine line between saving lives and causing harm. From blood pressure pills that combine two drugs to antibiotics paired to fight resistant infections, these stories show how medicine doesn’t always work in singles—it often works in pairs. And sometimes, the difference between recovery and complication comes down to knowing which combo is right, when, and why.
Generic antibiotic combination products offer major cost savings and equal effectiveness to brand-name versions. Learn how they work, why they're not always available, and what patients and providers need to know about access and substitution.