When you’re prescribed an antibiotic, you probably don’t think about whether it’s a single drug or a mix of two or more. But many of the most effective treatments for serious infections aren’t just one antibiotic-they’re antibiotic combination products. These are medicines that combine two or more active ingredients, like piperacillin and tazobactam, to fight bacteria more effectively than either drug alone. The big question now is: are these combination drugs available as generics? And if so, what does that mean for your wallet and your health?
What Are Antibiotic Combination Products?
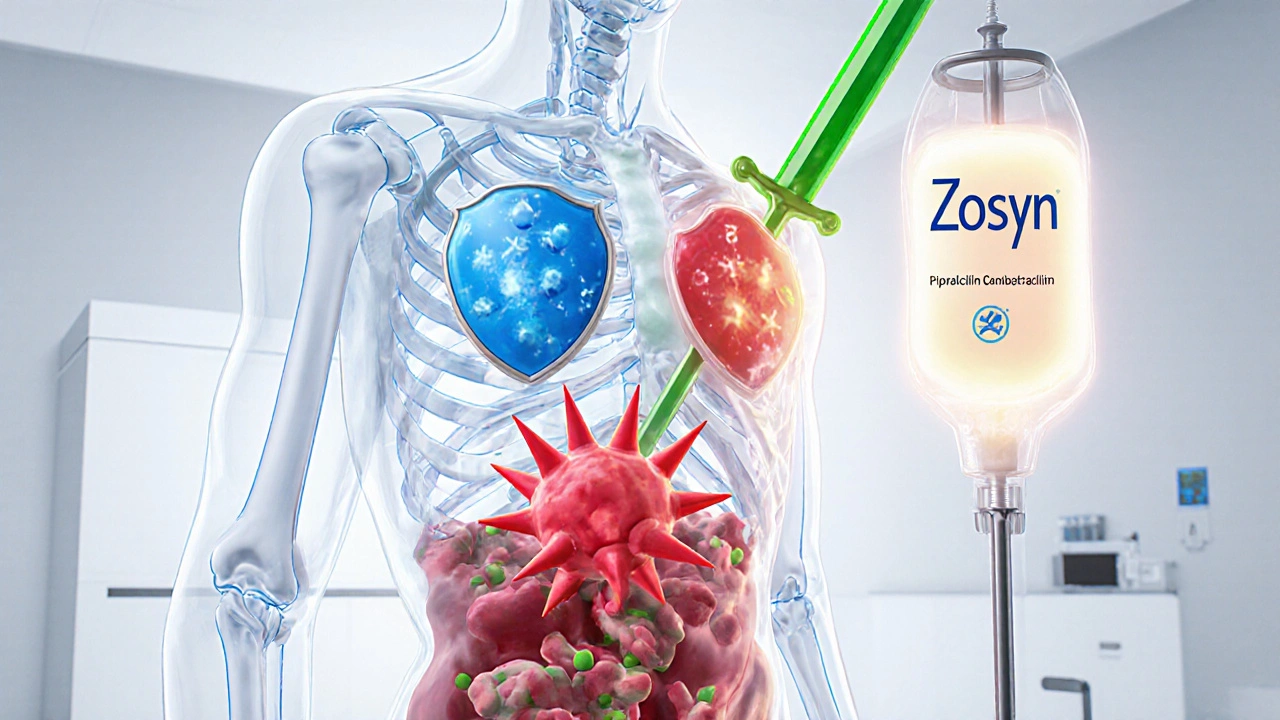
Antibiotic combination products aren’t just two pills in one bottle. They’re carefully designed formulations where two or more antibiotics-sometimes an antibiotic plus a helper compound-are blended to work better together. For example, piperacillin (an antibiotic) and tazobactam (a beta-lactamase inhibitor) are paired so that tazobactam blocks the bacteria’s defense mechanism, letting piperacillin kill the infection more efficiently. These combinations are used for hospital-acquired pneumonia, complicated urinary tract infections, and other tough-to-treat conditions.The U.S. Food and Drug Administration (FDA) classifies these as combination products because they can include drugs, devices, or both. Some come in IV bags, others in prefilled syringes or inhalers. That complexity makes them harder to copy than a simple tablet.
How Do Generic Versions Become Available?
Brand-name antibiotic combinations are protected by patents, usually for 20 years. Once those expire, manufacturers can apply to make a generic version using the Abbreviated New Drug Application (ANDA) process. But here’s the catch: unlike a plain tablet, a combination product with a delivery device-like a prefilled injector or an inhaler-requires extra proof.To get FDA approval, the generic version must show it’s therapeutically equivalent to the brand-name drug. That means:
- It delivers the same amount of each active ingredient into the bloodstream at the same rate
- It works the same way in the body
- It’s just as safe
- If it includes a device (like a syringe), the device doesn’t change how the drug is used or absorbed
Manufacturers don’t need to run new clinical trials. Instead, they submit detailed data showing the generic matches the original in chemistry, manufacturing, and performance. The FDA’s Office of Combination Products (OCP) reviews these applications and decides which center-drug or device-leads the evaluation based on the Primary Mode of Action (PMOA).
When Did Generic Antibiotic Combinations First Hit the Market?
The first major milestone came on October 26, 2010, when Hospira launched the first generic version of piperacillin-tazobactam for injection in the U.S. That was a big deal. Before that, patients and hospitals were paying hundreds of dollars per dose for the brand-name Zosyn. The generic version slashed the cost by more than 70% almost overnight.Since then, more generic antibiotic combinations have entered the market. But progress has been slow. Why? Because each combination product is unique. A simple oral antibiotic like amoxicillin is easy to copy. But a combination delivered through a complex inhaler or infusion pump? That’s a whole different challenge. Manufacturers need to prove every part-the drug, the container, the delivery mechanism-works identically to the original. That takes time, money, and regulatory expertise.

Do Generic Antibiotic Combinations Actually Save Money?
Yes. And the savings are massive.A 2021 study in Nature Communications found that when generic versions of antibiotics entered the market, prices dropped by 30% to 80%. Between 2010 and 2020, generic drugs saved the U.S. healthcare system an estimated $2.2 trillion. Antibiotic combinations contributed significantly to that number.
For patients, that means lower out-of-pocket costs. For hospitals, it means more budget flexibility. For public health, it means more people can afford the treatment they need. Studies show that when drug prices fall, adherence improves. People are more likely to finish their full course of antibiotics when they don’t have to choose between paying for meds and paying for groceries.
Why Aren’t All Antibiotic Combinations Available as Generics?
It’s not just about patents expiring. There are real barriers.First, the regulatory process is complicated. If a combination product includes a device-like a pre-filled syringe or a nasal spray device-the FDA requires extra documentation. Manufacturers must prove that the device doesn’t alter how the drug is absorbed or used. Even small changes in the syringe’s plunger or the vial’s seal can trigger a red flag.
Second, state laws don’t always allow pharmacists to substitute generic combination products. In many states, substitution laws were written for simple pills and don’t account for complex delivery systems. So even if a generic is approved, a pharmacist might not be allowed to swap it in without a new prescription.
Third, market demand plays a role. If a combination product is only used in a small group of patients-like those with cystic fibrosis-manufacturers may not see enough profit to justify the cost of developing a generic. That’s why some antibiotics, like aztreonam, saw a spike in prescriptions after generics arrived: it was being used in new ways for cystic fibrosis patients, and the lower cost made it more accessible.
What’s Changed Since 2020?
The FDA has been working to make the process clearer. In September 2024, the agency held a conference called REdI, focused on “Combination Products: Updates and Best Practices.” They outlined new guidance for manufacturers on how to structure ANDA submissions for drug-device combinations.One key update: the FDA now encourages companies to use a six-phase development approach specifically designed for generic drug-device combination products (g-DDCPs). This framework helps manufacturers avoid costly missteps by identifying regulatory hurdles early.
Legal experts are also pushing for change. A 2023 analysis pointed out that current substitution laws were built for oral drugs and are now outdated. The author argued that without federal and state-level reforms, patients will continue to face unnecessary barriers to affordable combination therapies.
What Should Patients and Providers Know?
If you’re prescribed an antibiotic combination:- Ask if a generic version is available. It might be cheaper and just as effective.
- Check with your pharmacist. Even if a generic exists, your state might not allow substitution.
- Don’t assume all combination products are the same. Piperacillin-tazobactam isn’t the same as amoxicillin-clavulanate. Each has its own dosing, delivery, and approval status.
- If cost is an issue, ask your doctor about alternatives. Sometimes switching to a single-agent antibiotic or a different combination can reduce expenses without sacrificing effectiveness.
For prescribers, it’s important to understand that not all generic combinations are created equal. Some may have different excipients, packaging, or delivery methods. These differences don’t affect safety or efficacy-but they can affect how the drug is used in practice. Always verify the product’s FDA-approved labeling.
What’s Next for Generic Antibiotic Combinations?
The number of combination products is growing. New ones are being developed for resistant infections, chronic lung diseases, and even cancer-related infections. As these products become more common, the pressure to fix the regulatory and legal gaps will increase.Experts predict that within the next five years, we’ll see more streamlined approval pathways for g-DDCPs. The FDA is likely to adopt more flexible standards for device equivalence, especially for products with well-established drug components. That could mean faster access to cheaper versions of new combination therapies.
But progress depends on more than regulation. It needs collaboration between manufacturers, pharmacists, insurers, and policymakers. Without changes to state substitution laws and better education for prescribers, even approved generics might not reach the patients who need them.
For now, the message is clear: generic antibiotic combination products are here, they’re saving money, and they’re working. But the system around them still has holes. Fixing those holes isn’t just about cost-it’s about making sure everyone who needs these life-saving treatments can actually get them.
Are generic antibiotic combination products as effective as brand-name ones?
Yes. The FDA requires generic antibiotic combination products to prove they are therapeutically equivalent to the brand-name version. That means they deliver the same amount of each active ingredient, work the same way in the body, and have the same safety profile. Manufacturers don’t need to run new clinical trials-they must show bioequivalence through detailed lab and manufacturing data. If the product includes a device (like a syringe), it must also perform identically in use.
Why aren’t all antibiotic combinations available as generics?
Several factors limit availability. First, complex delivery systems-like inhalers or infusion pumps-make manufacturing and approval harder and more expensive. Second, state laws often don’t allow pharmacists to substitute combination products, even when generics exist. Third, if a combination is used for a rare condition, manufacturers may not see enough demand to justify the cost of development. Finally, patent extensions or legal challenges can delay generic entry.
Can I ask my pharmacist to switch me to a generic antibiotic combination?
It depends on your state’s laws and the specific product. In many states, substitution laws only apply to simple oral drugs. If your prescription is for a combination product with a device (like a prefilled syringe), your pharmacist may not be legally allowed to substitute it-even if a generic is available. Always ask your pharmacist if substitution is permitted and check your prescription label for the brand name.
How much money can I save with a generic antibiotic combination?
Savings vary, but studies show price drops of 30% to 80% after generic entry. For example, the generic version of piperacillin-tazobactam cost over 70% less than the brand-name version when it launched. For patients paying out of pocket, that could mean hundreds of dollars saved per course of treatment. Insurance plans also benefit, which can lead to lower premiums and copays over time.
Do generic antibiotic combinations have different side effects?
No. The FDA requires generic versions to have the same active ingredients and meet the same safety standards as the brand-name product. Any differences in inactive ingredients (like fillers or preservatives) must not affect safety or performance. Side effects should be identical. If you experience a new or unusual reaction after switching to a generic, report it to your doctor-it’s rare, but possible.

Erika Sta. Maria
November 20, 2025 AT 21:07soooooo... we're just supposed to trust that the FDA's 'therapeutic equivalence' isn't just corporate magic dust? 🤔 i mean, if the syringe plunger is 0.2mm longer, does that really NOT change absorption?? i've seen generic insulin that made people hypoglycemic-this feels like russian roulette with antibiotics. #TrustTheProcessNotTheFDA
Debanjan Banerjee
November 22, 2025 AT 02:06Let me clarify the regulatory reality: bioequivalence for combination products is rigorously validated through in vitro dissolution profiles, pharmacokinetic studies, and device performance testing. The FDA’s Office of Combination Products applies a risk-based approach-each component is assessed for its primary mode of action. Generic piperacillin-tazobactam has demonstrated identical AUC and Cmax values in multiple peer-reviewed studies. The 70% cost reduction is not anecdotal-it’s empirically documented in JAMA Internal Medicine, 2018. This isn’t speculation; it’s pharmacology.
Steve Harris
November 23, 2025 AT 15:24Debanjan’s right-this is solid science. But I also get why people are skeptical. I work in a rural ER, and last month a patient got the generic combo, but the prefilled syringe had a different tip cap. Nurse didn’t know how to prime it right, so the first dose was delayed. It’s not the drug-it’s the system. We need better training, not just better generics. Also, props to the FDA for the new six-phase framework. That’s actually a big step forward.
Michael Marrale
November 24, 2025 AT 09:45wait… so you’re telling me the FDA isn’t in bed with Big Pharma? 😏 i’ve got sources. Did you know the same company that makes Zosyn also owns a lobbying firm that writes FDA guidance? And the 'generic' syringe? It’s made in the same factory. They just relabeled it. The real savings? They go to shareholders. You think patients are saving? Nah. We’re just being fed cheaper versions of the same poison. 🕵️♂️💊
David vaughan
November 26, 2025 AT 00:16Just wanted to say… thank you for writing this. 🙏 I’ve been fighting with my insurance for months to get my dad’s generic piperacillin-tazobactam covered. They kept saying 'brand only.' I had to print out the FDA’s equivalence guidelines and send them a certified letter. It worked. He’s home now. And yes, the generic worked fine. No side effects. Just… cheaper. So thank you. 🌟
Cooper Long
November 27, 2025 AT 23:21Sheldon Bazinga
November 28, 2025 AT 08:49generic? more like genericus interruptus. 😂 we’re just letting China and India make our life-saving drugs now? next they’ll be printing our insulin on 3D printers in a basement in Bangalore. i mean, sure, it’s cheaper… but what’s the catch? you think these ‘equivalent’ syringes don’t leak? you think the ‘same’ bacteria don’t laugh at our generics? 🤡 #AmericaFirstAntibiotics
Sandi Moon
November 28, 2025 AT 18:07One must ask: if these combination products are so easily replicated, why did it take over a decade for the first generic to emerge? The answer lies not in science, but in the deliberate obstruction of patent evergreening and regulatory capture. The FDA’s 'six-phase framework' is merely a PR stunt. The real barrier? The medical-industrial complex. We are not patients-we are revenue streams. And generics? They’re the only thing keeping us from being priced into oblivion. The system is rigged. But at least the drugs work. For now.
Kartik Singhal
November 29, 2025 AT 14:06bro the fact that you think a generic syringe is the same as the brand one is wild. 😴 like… you know how many times i’ve seen the plunger stick? or the vial crack? i’m not saying it’s dangerous… just… why are we pretending this is rocket science? it’s not. it’s just a vial with two liquids. if you’re paying $800 for Zosyn, you’re being scammed. period. 🤷♂️💊 #genericisfine
Logan Romine
November 30, 2025 AT 12:19so let me get this straight… we spent 20 years patenting combinations so pharma could charge $1200 for a vial… then when generics finally drop, we act like we’re surprised it works? 🤦♂️ the real conspiracy isn’t that generics are unsafe-it’s that we let corporations decide who lives and who doesn’t based on a spreadsheet. and now we’re supposed to be grateful for crumbs? congrats, we’re all just NPCs in a healthcare simulation. 🌌