Imagine you’re told to take a pill every morning to control your blood pressure. You do it for a week, then skip a few days because you felt fine. A month later, you’re back in the hospital. Was it your fault? Or was the system set up to fail you?
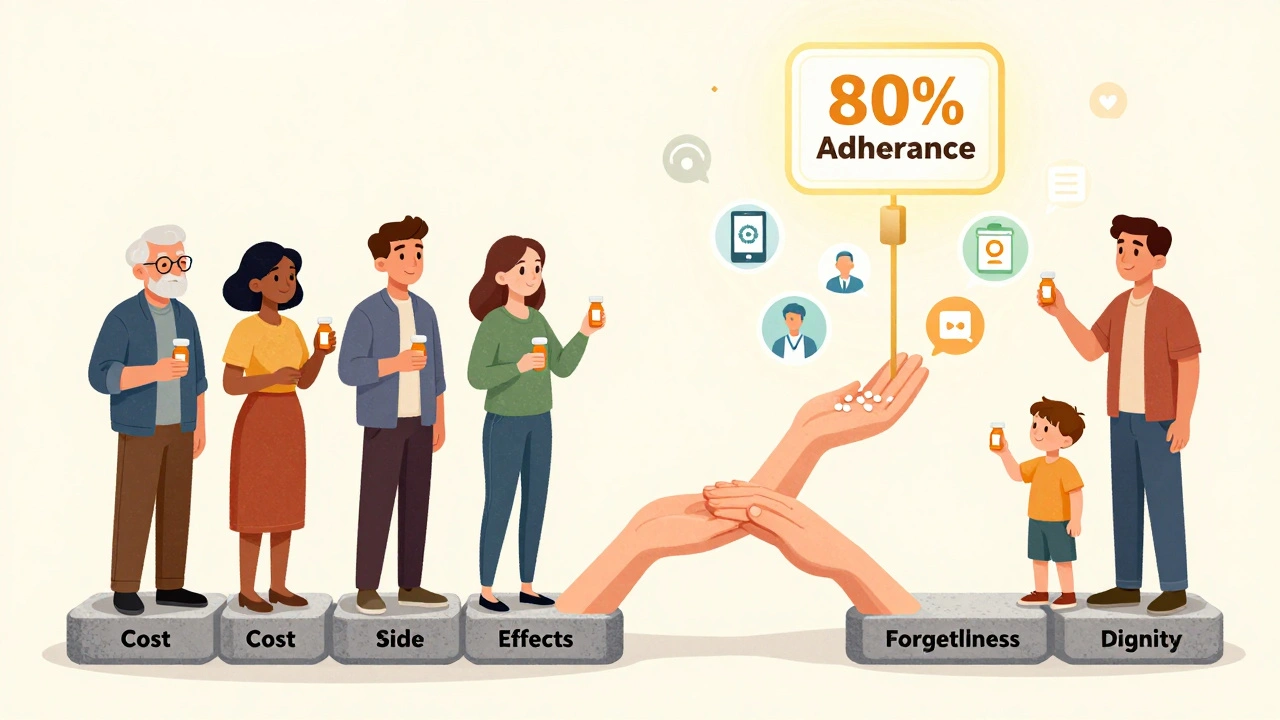
This isn’t just about forgetting pills. It’s about how we talk about medicine-and who gets blamed when it doesn’t work. For decades, doctors used the word compliance: "Did you follow the instructions?" It sounded simple. But it ignored the real reasons people stop taking their meds: cost, side effects, confusion, or just plain exhaustion. Today, the field has shifted. The right word is medication adherence. And that small change in language is saving lives.
What’s the Difference Between Adherence and Compliance?
At first glance, adherence and compliance seem like synonyms. Both describe whether someone takes their medicine as prescribed. But the difference is huge-and it changes everything.
Compliance means doing what you’re told. It’s a one-way street: doctor gives order, patient obeys. If you miss a dose, you’re labeled non-compliant. No questions asked. It’s like being told to clean your room and getting scolded if you don’t.
Adherence is different. It’s about partnership. The American Pharmacists Association defines it as "the extent to which a patient’s behavior matches agreed-upon recommendations." Notice the word "agreed-upon." That’s the key. Adherence assumes the patient has a voice. Maybe they can’t afford the pill. Maybe the side effects make them dizzy. Maybe they don’t believe it’s working. Adherence doesn’t blame them. It asks: Why?
The shift started in the late 1990s. Medical journals like the Journal of Clinical Pharmacy and Therapeutics and the Annals of Internal Medicine began pushing for the change. By the early 2000s, major health organizations had dropped "compliance" from their official language. Today, the FDA, EMA, and CDC all use "adherence." Even the American Medical Association now defines adherence as taking at least 80% of prescribed doses over time-not perfect, but close enough to matter.
Why Adherence Is the Standard Now
Compliance doesn’t work for chronic diseases. That’s the hard truth.
Think about diabetes, high blood pressure, or cholesterol. These aren’t illnesses you fix in a week. You take meds for years. And yet, the World Health Organization says about half of all patients stop taking their meds within the first year. Why? Because compliance doesn’t solve the problem-it just labels it.
Adherence, on the other hand, digs deeper. It looks at the whole picture:
- Initiation: Did the patient even start the medication?
- Implementation: Are they taking the right dose at the right time?
- Discontinuation: Did they quit because of side effects, cost, or fear?
Compliance only checks the middle part. Adherence looks at all three-and that’s why it works better.
A 2024 analysis by the AARDEx Group found that 68% of non-adherence isn’t about laziness. It’s about real barriers: forgetfulness, complex regimens, lack of understanding, or feeling dismissed by providers. When doctors treat patients like partners, not patients, adherence rates jump.
How Adherence Is Measured
How do we know if someone is adherent? It’s not as simple as asking.
There are four main ways:
- Pill counts: Pharmacists count leftover pills. Simple, but easy to fake.
- Prescription refill records: Did you refill your script on time? This is the most common method used by insurers and clinics.
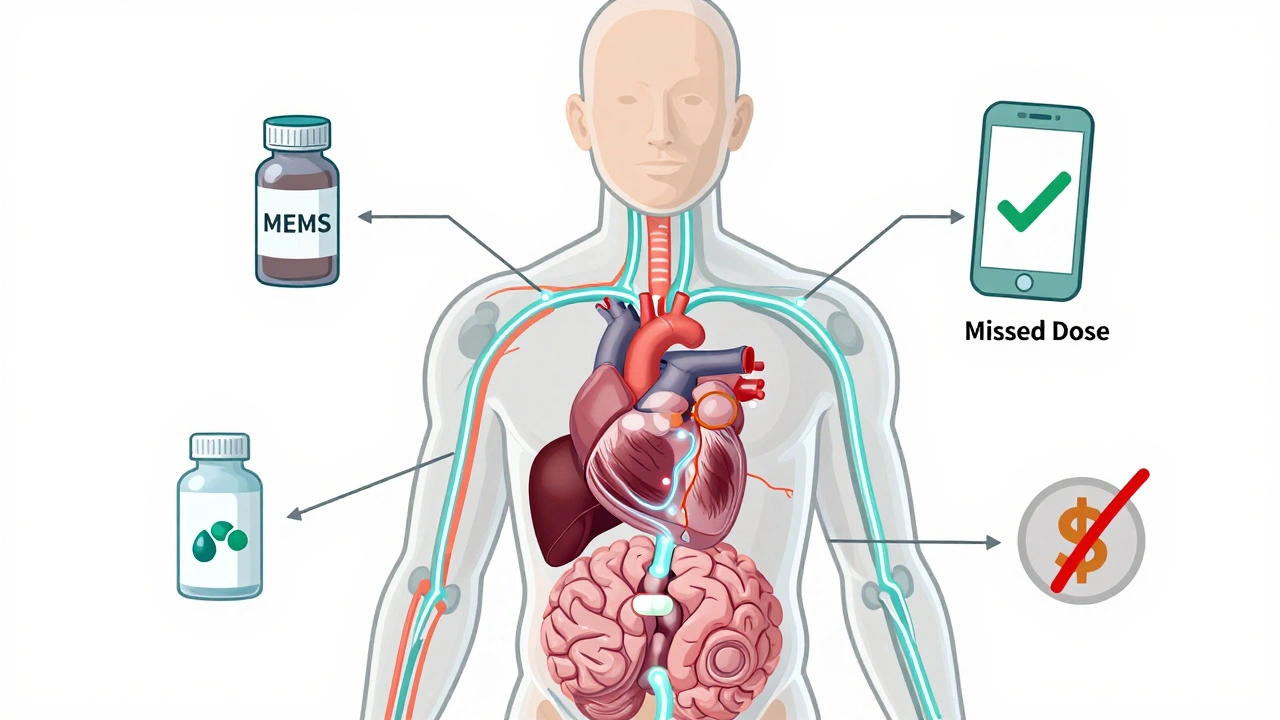
- Electronic monitoring: Smart pill bottles like MEMS caps record when they’re opened. This gives exact timing data-no guessing.
- Self-reporting: Patients answer questions like, "In the past week, how many doses did you miss?" Surprisingly, this is often accurate when patients feel safe being honest.
The gold standard? A Medication Possession Ratio (MPR) of 80% or higher. That means you had enough pills to cover at least 80% of the days you were supposed to take them. It’s not perfect, but it’s the benchmark the AMA and CMS use.
Compliance, by contrast, only checks if pills were taken on specific days-usually during clinic visits. That’s why it’s useless for long-term conditions. You can’t watch someone 24/7.
Why This Matters for Your Health
Non-adherence isn’t just inconvenient. It’s deadly.
When people skip heart meds, their risk of stroke doubles. Missed diabetes pills lead to kidney failure. Skipping asthma inhalers lands people in the ER. The Agency for Healthcare Research and Quality found that adherence-focused care improves treatment success by 20-50% compared to compliance-based approaches.
And the cost? In the U.S. alone, poor medication adherence causes an estimated $300 billion in avoidable healthcare spending each year. That’s hospital stays, ER visits, and emergency care-all preventable.
It’s not just about money. It’s about quality of life. A 2025 WHO report estimates that if adherence improved globally, we could prevent 850,000 premature deaths in low- and middle-income countries by 2030. That’s not a number. That’s families. Grandparents. Parents.
What Works: Real Solutions That Help
So how do we fix this?
It’s not about nagging. It’s about support.
Here’s what actually moves the needle:
- Motivational interviewing: Instead of saying, "You need to take this," providers ask, "What’s making it hard for you?" This builds trust and uncovers hidden barriers.
- Personalized education: One-size-fits-all pamphlets don’t work. Tailoring info to a patient’s literacy level, culture, and daily routine does.
- Technology: Apps like Hero Health and Dose Packer send reminders, track doses, and alert caregivers if a pill is missed. One Kaiser Permanente study showed a 42% drop in missed doses with these tools.
- Simplified regimens: Fewer pills per day = better adherence. Doctors are now prescribing combination pills and once-daily options whenever possible.
- Pharmacist involvement: Community pharmacists who check in with patients after a new prescription see adherence rates rise by 37.6%, according to the National Community Pharmacists Association.
It’s not magic. It’s just better communication.
The Financial Shift: Insurance and Policy Are Catching Up
Money talks-and healthcare is finally listening.
In January 2024, the Centers for Medicare & Medicaid Services (CMS) started tying 8% of hospital reimbursements to medication adherence metrics for chronic conditions. If your patients keep ending up in the hospital because they skipped meds, your hospital gets penalized.
The American Medical Association responded by creating new billing codes in 2025: 99487-99489. These let doctors get paid for spending time counseling patients on adherence. Before, they got paid for the pill, not the conversation. Now, they’re rewarded for the relationship.
Even big tech is jumping in. Google Health’s 2024 study used AI to predict who’s likely to stop taking their meds-by analyzing 27 factors like income, transportation access, past refill patterns, and even social media mentions of side effects. Their algorithm was 83.7% accurate. That’s not sci-fi. That’s healthcare’s future.
What’s Still Holding Back Progress
Change isn’t universal.
While 87% of major health systems switched to adherence language by mid-2024, correctional facilities still use "compliance" in 63% of cases. Why? Because they’re still run like prisons, not clinics.
Some providers still resist. It’s harder to have a conversation than to write a prescription. And it takes time-15 to 25 extra minutes per visit, according to the American Academy of Family Physicians. But that time pays off. One 2023 study showed patients who had adherence-focused visits were 2.57 times more likely to stay on their meds.
There’s also bias. Too often, patients who miss doses are called "non-compliant" or "difficult." That shuts down communication. Adherence asks: "What’s going on?" instead of "Why won’t you listen?"
What You Can Do
If you’re taking meds long-term:
- Ask your pharmacist: "Can you help me simplify this regimen?"
- Use a pill organizer or app. Even a basic one with alarms helps.
- Be honest with your doctor. If you’re skipping doses because of cost, say so. There are often patient assistance programs.
- Don’t stop meds just because you feel better. That’s how relapses start.
If you’re a caregiver or family member:
- Don’t nag. Ask questions: "What’s the hardest part about taking your pills?"
- Help them set reminders. Link pill-taking to daily habits-like brushing teeth or eating breakfast.
- Advocate for them. If they’re struggling, call their doctor together.
Final Thought: It’s Not About Obedience. It’s About Partnership.
Medication adherence isn’t about control. It’s about care.
The old model-"Do as you’re told"-failed because it treated people like machines. The new model-"Let’s figure this out together"-works because it treats people like humans.
Adherence recognizes that your life matters. Your schedule. Your budget. Your fears. Your beliefs. Your dignity.
And that’s why it matters-not just for statistics, but for the person taking the pill every morning.
Is medication adherence the same as compliance?
No. Compliance means following orders without question. Adherence means working with your provider to follow a treatment plan you understand and agree to. Adherence includes your reasons, barriers, and choices. Compliance does not.
What percentage of people are truly adherent to their meds?
Only about half of patients with chronic conditions are adherent. The World Health Organization estimates 50% stop taking their prescribed medications within the first year. For some conditions like high blood pressure, adherence rates can be as low as 30% after 12 months.
What is the 80% adherence rule?
The American Medical Association defines an adherent patient as someone who takes at least 80% of their prescribed doses over a given period. This is measured using Medication Possession Ratio (MPR), which looks at how many pills you had available versus how many you were supposed to take. It’s not about perfection-it’s about consistency.
Can technology help with medication adherence?
Yes. Smart pill bottles, mobile apps, and automated reminders have been shown to reduce missed doses by 30-42% in clinical studies. Tools like Hero Health and Dose Packer track when pills are taken and alert caregivers if doses are skipped. Some even integrate with electronic health records to give providers real-time data.
Why do doctors still use the word 'compliance' sometimes?
Some providers still use 'compliance' out of habit or because they work in systems that haven’t fully transitioned-like correctional healthcare, where 63% of facilities still use the term. Others may not be aware of the shift. But major organizations like the FDA, AMA, and WHO have officially moved to 'adherence' since the early 2000s, and it’s now the standard in patient-centered care.
How can I talk to my doctor about adherence without sounding like I’m not following orders?
Say something like: 'I want to take my meds as prescribed, but I’ve been having trouble with [cost/side effects/forgetting]. Can we talk about what might make this easier?' This opens the door for real solutions-not judgment. Providers trained in adherence-focused care will appreciate your honesty and work with you.


Pavan Kankala
December 5, 2025 AT 21:22They say 'adherence' now to make us feel less guilty, but let's be real-this is just corporate buzzword bingo. The system still doesn't care if you're broke, tired, or scared. They just swapped the label so they can bill better. 80% adherence? That’s not a standard, it’s a loophole for insurers to stop paying for your side effects.
Martyn Stuart
December 6, 2025 AT 09:21Finally! Someone’s talking about the language shift properly. 'Compliance' is a relic of paternalistic medicine-it implies obedience, not partnership. 'Adherence' acknowledges agency, context, and lived experience. It’s not semantics-it’s ethics. And yes, the WHO, FDA, and AMA have been clear since the early 2000s. If your clinic still says 'compliance,' they’re operating in 1998.
Jessica Baydowicz
December 6, 2025 AT 21:56Yessss! This is the kind of post that makes me wanna hug my pharmacist. I used to skip my blood pressure meds because I felt fine-until I passed out at the grocery store. My doc didn’t yell. She asked, 'What’s stopping you?' Turns out, the pill cost $120/month. We switched to a generic. Now I take it with my morning coffee. No guilt. Just care. 💪
Shofner Lehto
December 8, 2025 AT 16:48Adherence isn’t just a buzzword-it’s a clinical paradigm shift. The data is overwhelming: when patients are involved in co-creating their treatment plan, persistence increases by 30–60%. Pill counts and refill records are crude tools. Electronic monitoring and motivational interviewing are the future. The real win? When providers stop seeing non-adherence as a failure of the patient and start seeing it as a failure of the system.
Rachel Bonaparte
December 10, 2025 AT 05:46Let’s not pretend this is about care. This whole 'adherence' movement? It’s Big Pharma’s PR campaign dressed up in woke language. They know patients can’t afford these drugs-so they rebrand non-payment as 'barriers' so hospitals get reimbursed for 'counseling.' Meanwhile, the same companies jack up prices 200% every year. The word changed. The profit didn’t. Wake up.
And don’t get me started on 'smart pill bottles.' They’re tracking us. Every cap opening. Every missed dose. Who’s got access to that data? Insurers? Employers? The government? This isn’t healthcare. It’s surveillance with a stethoscope.
They want you to think it’s about dignity. It’s about liability. They need you to look like you’re trying so they don’t get sued when you die.
And yet-somehow, the real solution is still the same: universal healthcare. But that’s too radical for the AMA’s annual conference.
Michael Feldstein
December 11, 2025 AT 07:36I’ve worked in community health for 12 years. The biggest barrier isn’t cost or forgetfulness-it’s shame. Patients don’t tell their doctors they stopped taking meds because they’re embarrassed. They think they’re 'bad' for not following orders. That’s why the shift to 'adherence' matters. It removes the moral judgment. When we say, 'What’s making this hard?' instead of 'Why didn’t you take it?'-people open up. It’s not magic. It’s basic psychology.
And yes, pharmacists are the unsung heroes here. They’re the ones who notice when someone hasn’t picked up a script in 90 days. They call. They ask. They help. We need more of them in the loop.
Libby Rees
December 11, 2025 AT 21:25Interesting. The terminology shift from compliance to adherence reflects a broader movement toward patient-centered care. It is not merely semantic. It is structural. The distinction is well-documented in peer-reviewed literature since the late 1990s. The American Medical Association's definition of 80% adherence as clinically meaningful is pragmatic, not idealistic. Real-world behavior is imperfect. The goal is sustainability, not perfection.
Rudy Van den Boogaert
December 12, 2025 AT 18:47I’ve seen this play out in my mom’s care. She’s on five meds for diabetes, hypertension, and arthritis. Her doctor used to say, 'You need to be more compliant.' Then she switched to a new doc who asked, 'Which one’s the hardest?' Turns out, the arthritis pill made her nauseous at breakfast. We moved it to dinner. Cost dropped when we found a coupon. Now she takes them all. No lectures. Just teamwork.
It’s not about being perfect. It’s about being heard.
Gillian Watson
December 13, 2025 AT 16:56Love this. I’m a nurse in London and we’ve been using 'adherence' for years. Patients respond better. They feel like they’re part of the plan, not just a list of instructions. Even the older ones get it. It’s not about obedience. It’s about respect.
Jordan Wall
December 14, 2025 AT 10:10Adherence? More like 'medication compliance 2.0' with a side of AI surveillance and blockchain-enabled pill bottles 🤖💊. The pharma-industrial complex just needs a new buzzword to sell more wearables and 'counseling codes' while keeping insulin at $300 a vial. Also, 'MEMS caps'? That's a trademarked product, not a clinical standard. Don't get me started on Google Health's 'AI prediction model'-they trained it on Medicaid data and now they're selling 'risk scores' to insurers. We're not saving lives. We're monetizing vulnerability.
Gareth Storer
December 15, 2025 AT 07:57So now we’re supposed to feel good about taking pills because someone changed the word? Great. Next they’ll call smoking 'tobacco engagement' and call cancer 'resistance to nicotine cessation.' I’m just glad I don’t have to take any of this crap.
Karl Barrett
December 15, 2025 AT 18:07This is the most human thing I’ve read about healthcare in years. It’s not about pills. It’s about trust. When you treat someone like a partner-not a problem-you unlock something deeper. I’ve had patients cry when I asked, 'What’s stopping you?' because no one ever asked before. They thought they were failures. They weren’t. They were just drowning in a system that doesn’t see them. Adherence isn’t a metric. It’s a promise: 'Your life matters enough for us to listen.'
And yeah, the $300 billion in avoidable costs? That’s not a statistic. That’s 300,000 people who didn’t have to die alone in a hospital bed because no one asked if they could afford their medicine.
val kendra
December 15, 2025 AT 19:36My dad died because he stopped his heart meds-he thought they were making him dizzy. He never told anyone. We found out too late. This post? It’s the reason I became a pharmacist. Not to sell pills. To ask the hard questions. To sit with people. To say: 'It’s okay. Let’s fix this together.' No judgment. Just care.