Many people take turmeric for its anti-inflammatory benefits, thinking it’s just a harmless spice. But if you’re on a blood thinner like warfarin, clopidogrel, or rivaroxaban, turmeric - especially in supplement form - can be dangerous. The problem isn’t just theoretical. Real patients have ended up in emergency rooms with dangerously high INR levels, internal bleeding, and kidney damage after adding turmeric supplements to their daily routine.
How Turmeric Acts Like a Blood Thinner
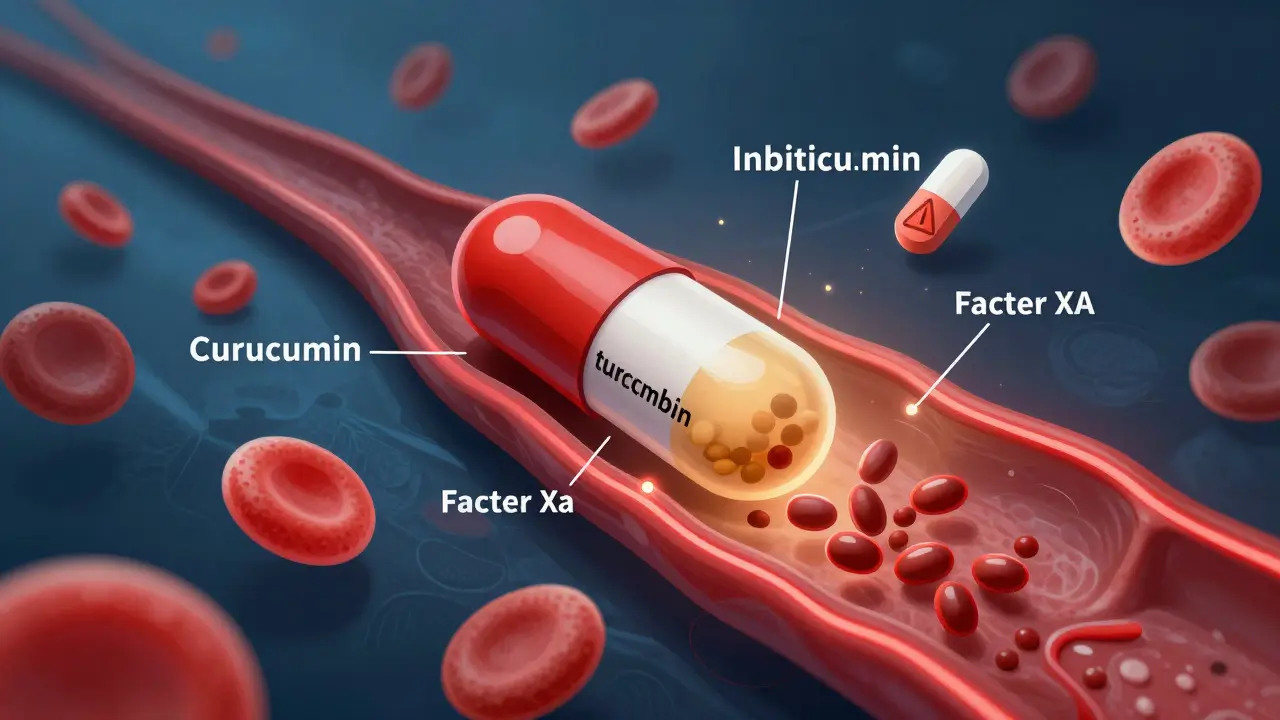
Turmeric gets its bright yellow color from curcumin, which makes up about 2-8% of raw turmeric powder. But it’s not just a colorant. Curcumin directly interferes with your blood’s ability to clot. Research shows it slows down two key steps in the clotting process: it inhibits thrombin and factor Xa, two proteins your body needs to form clots. It also reduces platelet aggregation - meaning your blood platelets stick together less easily. This is the same goal as prescription blood thinners, but without the precision. Unlike warfarin, which targets vitamin K metabolism, or DOACs like apixaban, which block factor Xa in a controlled way, curcumin hits multiple targets at once. That’s why its effects are harder to predict. One study published in PubMed found that curcumin’s anticoagulant effect was even stronger than its cousin compound, bisdemethoxycurcumin. That means the very structure of curcumin - the methoxy groups - makes it more potent at thinning blood.Real Cases: When Turmeric Almost Killed Someone
In 2018, Medsafe in New Zealand reported a case of a patient on stable warfarin therapy. Their INR - a measure of how long it takes blood to clot - had been steady at 2.5 for months. After starting a turmeric supplement, their INR jumped to over 10. The therapeutic range for warfarin is 2-3.5. Above 4.5, bleeding risk increases sharply. At 10, the risk of spontaneous bleeding - including brain hemorrhage - becomes life-threatening. This patient didn’t have a fall or injury. The blood thinning came from the supplement. Another case involved a kidney transplant patient taking tacrolimus, a drug that prevents organ rejection. They were consuming 15 or more spoonfuls of turmeric powder daily for ten days. Their tacrolimus levels spiked to 29 ng/mL - more than double the safe limit. The result? Acute kidney injury. Turmeric doesn’t just affect clotting; it interferes with liver enzymes (CYP3A4) that break down many medications. That means other drugs build up in your system, too. These aren’t rare anecdotes. They’re documented medical events. The Welsh Medicines Information Centre confirmed similar cases in 2021 and updated their warning again in October 2024. The message is consistent: turmeric supplements can cause serious harm when mixed with anticoagulants.Which Blood Thinners Are Riskiest With Turmeric?
The interaction isn’t the same across all blood thinners, but the danger is real with nearly all of them:- Warfarin (Coumadin): Highest risk. Warfarin has a narrow therapeutic window - a tiny change in dose or metabolism can push you from safe to life-threatening. Turmeric alters how warfarin is broken down, causing levels to rise unpredictably.
- DOACs (rivaroxaban, apixaban, dabigatran): These newer drugs don’t require regular INR checks, but that doesn’t make them safer with turmeric. Curcumin inhibits factor Xa - the exact target of rivaroxaban and apixaban. Combining them doubles the effect.
- Aspirin, clopidogrel (Plavix): These are antiplatelet drugs, not anticoagulants, but turmeric adds to their effect. The combination increases bruising, nosebleeds, and gastrointestinal bleeding.
- Enoxaparin (Lovenox), dalteparin (Fragmin): These injectable heparins are often used after surgery or for deep vein clots. Turmeric can push their effect into dangerous territory.
- NSAIDs (ibuprofen, naproxen, diclofenac): These painkillers already raise bleeding risk. Turmeric doesn’t just add to that - it multiplies it.

Why Supplements Are Worse Than Spice
Eating turmeric in curry is unlikely to cause problems. A teaspoon of ground turmeric contains maybe 20-40 mg of curcumin. That’s not enough to significantly affect clotting in most people. But supplements? That’s a different story. A single capsule can contain 500 mg of curcumin - and some high-potency extracts are up to 95% pure curcumin. That’s 10 to 50 times more than you’d get from food. And there’s no standardization. Two bottles labeled “1000 mg turmeric extract” can have wildly different curcumin levels. One might have 50 mg. Another might have 950 mg. You can’t know what you’re getting. Doctors can monitor warfarin doses with blood tests. They can adjust your pill count if your INR creeps up. But they can’t adjust for turmeric supplements because they don’t know if you’re taking them - and even if you say you are, they can’t measure the dose.What Medical Experts Say
The warnings are getting stronger:- Medsafe (New Zealand, 2018): “Concurrent use… should be avoided.”
- Welsh Medicines Information Centre (2024): “Raised INR to a level associated with serious bleeding risk was reported.”
- Mayo Clinic Health System (2023): “Turmeric in large doses can act like a blood thinner, causing bleeding or dangerously enhancing the effects of blood-thinning medications.”
- British Heart Foundation (2023): “High doses of turmeric supplements could have blood-thinning effects that may interact with both DOACs and warfarin.”

What You Should Do
If you’re on a blood thinner and taking turmeric:- Stop the supplement immediately. Don’t wait for symptoms. Bleeding can start without warning.
- Tell your doctor or pharmacist. Even if you think it’s “just a natural remedy,” they need to know. Many patients don’t mention supplements because they assume they’re safe.
- Get an INR test. If you’re on warfarin, your doctor should check your INR within a few days of stopping the supplement to see how your levels respond.
- Don’t restart without approval. Even if you feel fine, the risk doesn’t disappear. One dose can push your INR into danger.
- Consider alternatives. If you’re taking turmeric for joint pain or inflammation, ask your doctor about safer options like fish oil (in controlled doses) or physical therapy.
- Ask your doctor if you’re on any other medications - especially for diabetes, thyroid, or immune conditions. Turmeric can interact with those too.
- Never take high-dose extracts without medical supervision.
- Remember: “Natural” doesn’t mean safe. Many deadly poisons come from plants.

Charlotte N
January 5, 2026 AT 08:19I never thought about how turmeric in pill form could be so different from the spice in my curry
My grandma always said natural doesn't mean harmless but I never listened until now
I've been taking turmeric capsules for my arthritis and now I'm terrified
Just checked my meds list and I'm on Eliquis
Guess I'm stopping it tomorrow
Vicki Yuan
January 6, 2026 AT 13:05This is one of those posts that should be mandatory reading for anyone taking supplements
It's not just about turmeric - it's about the entire supplement industry's lack of regulation
People think because it's plant-based, it's safe - but foxglove is a plant too
And we don't hand out digitalis pills at yoga studios
Doctors need to be proactive about asking about supplements, not waiting for patients to volunteer
The fact that this is still a hidden danger in 2024 is a systemic failure
Jennifer Glass
January 6, 2026 AT 17:13Interesting how we treat food differently than pills
Would you eat 50 teaspoons of turmeric powder in one sitting? Probably not
But take a capsule with 500mg? Totally fine, right?
It's the same compound - just concentrated
And concentration is what turns medicine into poison
Reminds me of how we used to think vitamin C could cure colds - until we realized megadoses just made your kidneys work overtime
Same pattern, different molecule
bob bob
January 6, 2026 AT 18:52Bro I took turmeric for years and never had an issue
But now that I'm on blood thinners after my stent? I cut it out cold turkey
My doc didn't even bring it up - I had to Google it myself
Shoutout to this post - saved my life
Also, curry is still my jam - just no capsules
Live long and spice smart
Uzoamaka Nwankpa
January 8, 2026 AT 18:28I’ve been taking turmeric supplements for 3 years now. I have no idea what’s in them. I buy them because they’re cheap and the label says ‘pure.’ I’m scared now. I don’t know what to do. I feel like I’ve been poisoned and no one told me.
Catherine HARDY
January 10, 2026 AT 09:21Did you know the FDA doesn’t regulate supplements at all? They don’t test them before they hit shelves
Companies can put anything in there - fillers, heavy metals, even actual blood thinners
And they don’t have to list it
They call it ‘natural’ to avoid scrutiny
But the real truth? Big Pharma doesn’t want you taking turmeric - it’s free
They make billions off warfarin and DOACs
So they let the warnings stay quiet
They want you dependent - not healed
Think about it - why are these warnings only coming out now?
Why wasn’t this on the front page of every news site?
Because they profit from your ignorance
Chris Cantey
January 11, 2026 AT 06:46Curcumin inhibits thrombin and factor Xa - yes
But isn't that just mimicking evolution? Nature designed plants to interfere with clotting to deter predators
So we're not fighting biology - we're fighting our own arrogance
We think we can extract molecules and control them like widgets
But biology doesn't work that way
It's a symphony, not a machine
And we're the ones who broke the tuning fork
Abhishek Mondal
January 11, 2026 AT 23:10Actually, the real issue here is the over-medicalization of natural substances - you people act like turmeric is a drug because you've been conditioned to believe only pharmaceuticals have potency
But in Ayurveda, turmeric has been used for millennia - with no reported bleeding events
Perhaps the problem isn't turmeric - it's the Western obsession with isolating compounds and dosing them like insulin
Curcumin in isolation is not the same as turmeric root in context
And you're ignoring the entire pharmacological framework that makes traditional use safe
Also - your citation from Medsafe? That was one case - you're turning anecdote into dogma
Correlation ≠ causation - and you're ignoring confounding variables
Maybe that patient was also drinking grapefruit juice - or taking St. John's Wort - or had undiagnosed liver disease
But no - it's easier to blame the spice
Terri Gladden
January 12, 2026 AT 12:01OMG I JUST TOOK A TURMERIC CAPSULE YESTERDAY AND IM ON PLAVIX IM GONNA DIE IM GONNA DIE IM GONNA DIE
MY HANDS ARE TINGLING IS THIS THE BLEEDING?? I CAN'T BREATHE
MY DOCTOR ISNT ANSWERING MY TEXTS I HATE THE SYSTEM
WHY DIDNT ANYONE TELL ME?? I JUST WANTED MY JOINTS TO STOP HURTING
WHY IS EVERYTHING SO DANGEROUS??
WHY CAN'T I JUST BE HAPPY??
Jack Wernet
January 13, 2026 AT 06:26Thank you for sharing this with such clarity and care - it's rare to see a post that balances scientific rigor with human urgency.
As someone who works in public health, I’ve seen too many patients assume ‘natural’ means ‘no risk’ - and too few providers ask about supplements during medication reviews.
What worries me most isn’t the science - it’s the silence.
Supplement labels don’t carry warnings like prescription drugs. No black box alerts. No pharmacist counseling. No mandatory disclosure.
And yet, millions take them daily alongside life-sustaining medications.
We need standardized labeling - like the ‘May interact with anticoagulants’ warnings on OTC painkillers.
We need pharmacy alerts when turmeric supplements are purchased with warfarin or DOACs.
We need education campaigns that don’t just say ‘avoid’ - but explain why, in plain language.
This isn’t about fearmongering. It’s about equity.
Everyone deserves to know what’s in their body - and what it might do to their medicine.
Thank you for being the voice that breaks the silence.