Introduction to Inflammatory Bowel Disease and Acotiamide
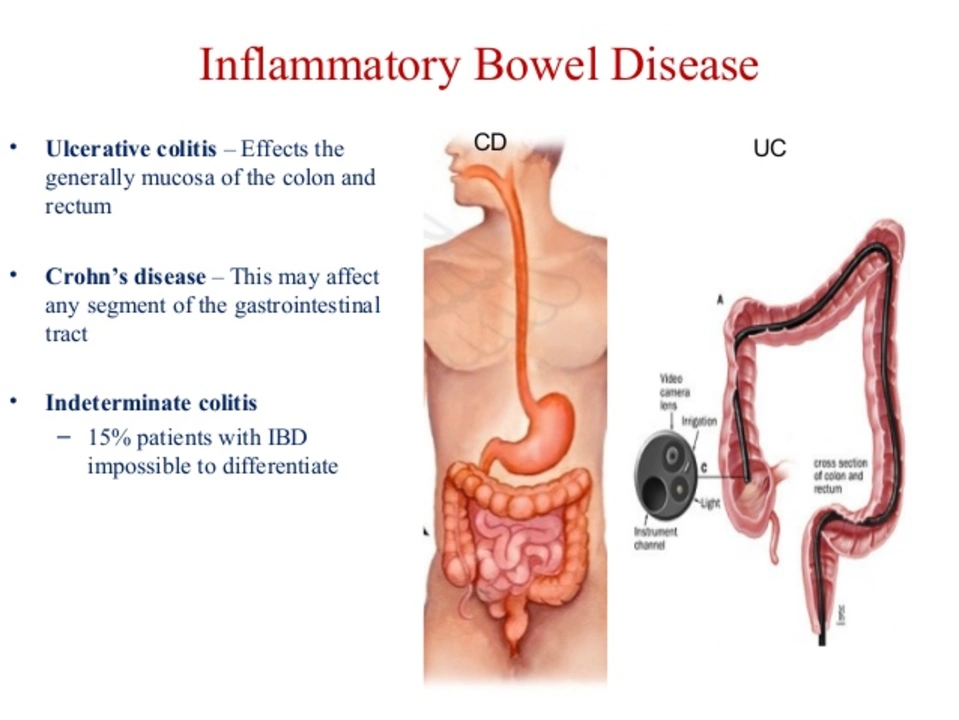
Inflammatory Bowel Disease (IBD) is a chronic condition that affects millions of people worldwide. It is characterized by inflammation in the gastrointestinal tract, leading to symptoms such as abdominal pain, weight loss, diarrhea, and fatigue. As someone who has experienced the debilitating effects of IBD, I understand how important it is to find effective treatments to manage this condition. One promising treatment option that has recently emerged is Acotiamide. In this article, I will discuss the role of Acotiamide in the management of IBD and explore its potential benefits in improving the quality of life for those who suffer from this chronic illness.
Understanding the Mechanism of Action of Acotiamide
The first aspect we need to understand is how Acotiamide works in the body. Acotiamide is a gastroprokinetic agent, which means it helps improve the movement and function of the gastrointestinal tract. It does this by inhibiting the enzyme acetylcholinesterase, which in turn increases the levels of acetylcholine, a neurotransmitter that controls the contractions of smooth muscles in the digestive system. By enhancing the motility and coordination of the gastrointestinal tract, Acotiamide can potentially alleviate some of the symptoms associated with IBD, such as abdominal pain, bloating, and constipation.
Acotiamide's Effects on Gastrointestinal Motility and IBD Symptoms
One of the major challenges in managing IBD is the disruption of normal gastrointestinal motility, which can lead to a variety of uncomfortable symptoms. Acotiamide has been shown to improve overall gastrointestinal motility, which can help reduce these symptoms. In clinical studies, patients with IBD who received Acotiamide treatment experienced significant improvements in their abdominal pain, bloating, and constipation. This suggests that Acotiamide could be a valuable addition to the current treatment options for IBD patients.
Reducing Inflammation with Acotiamide
Another potential benefit of Acotiamide in the management of IBD is its ability to reduce inflammation. Inflammation is a major factor in the development and progression of IBD and contributes to the chronic symptoms experienced by patients. Recent research has shown that Acotiamide can significantly reduce the production of pro-inflammatory cytokines, which are proteins that promote inflammation in the body. This anti-inflammatory effect could help alleviate the chronic inflammation associated with IBD, leading to improved symptom management and overall better health.
Acotiamide's Safety and Tolerability in IBD Patients
When considering any new treatment, it's essential to evaluate its safety and tolerability. In clinical trials, Acotiamide has been found to be well-tolerated by patients with IBD, with few reported side effects. The most common side effects include mild gastrointestinal symptoms, such as nausea and diarrhea, which are generally manageable and resolve on their own. This favorable safety profile makes Acotiamide a promising option for patients with IBD who may be seeking alternative treatments to help manage their symptoms.
Enhancing Quality of Life for IBD Patients with Acotiamide
Living with IBD can have a significant impact on an individual's quality of life. The chronic symptoms, as well as the emotional and social challenges that come with this condition, can be overwhelming. By improving gastrointestinal motility and reducing inflammation, Acotiamide has the potential to enhance the quality of life for patients with IBD. Improved symptom management can lead to better overall well-being, allowing patients to enjoy a more active and fulfilling life despite their chronic illness.
Combining Acotiamide with Other IBD Treatments
One of the key aspects of managing IBD is finding the right combination of treatments that work best for each individual patient. Acotiamide could be a valuable addition to a comprehensive IBD treatment plan. It may be used alongside other medications, such as anti-inflammatory drugs, immunosuppressants, and biologic therapies, to help improve symptom management and overall health. It's important for patients to discuss their treatment options with their healthcare provider to determine the best approach for their unique needs.
Future Research and Development of Acotiamide for IBD
While the initial findings on Acotiamide's potential benefits for IBD patients are encouraging, more research is needed to fully understand its role in the management of this chronic condition. Future studies should focus on long-term efficacy, safety, and tolerability, as well as the potential for Acotiamide to be used in combination with other IBD treatments. Additionally, research should explore the potential benefits of Acotiamide for specific subtypes of IBD, such as Crohn's disease and ulcerative colitis, to determine if it may be more effective for one type over another.
Conclusion: The Potential of Acotiamide in IBD Management
In summary, Acotiamide holds promise as a novel treatment option for patients with IBD. Its ability to improve gastrointestinal motility, reduce inflammation, and provide a favorable safety profile make it an attractive option for those seeking additional treatments to help manage their symptoms. While more research is needed, the findings so far indicate that Acotiamide could play a valuable role in improving the quality of life for those living with IBD.

Janice Rodrigiez
April 27, 2023 AT 01:43Acotiamide works by boosting acetylcholine which helps the gut move smoothly and can ease bloating and pain for many IBD patients
Roger Cardoso
April 29, 2023 AT 03:08One must wonder why mainstream journals overlook the hidden agenda behind promoting Acotiamide as a miracle cure
barry conpoes
May 1, 2023 AT 04:32Patriotic doctors should push Acotiamide forward because our nation deserves the best gut health solutions
Kristen Holcomb
May 3, 2023 AT 05:57Hey folks, just wanted to add that those dosing guidelines look solid – make sure to double‑check with your doc and keep track of any side‑effects
justin davis
May 5, 2023 AT 07:22Wow!!! Acotiamide is the *latest* thing!!! Who needs traditional meds when you can just wave a pill and hope for the best???
David Lance Saxon Jr.
May 7, 2023 AT 08:46From a mechanistic standpoint, Acotiamide functions as a selective acetylcholinesterase inhibitor, thereby augmenting cholinergic neurotransmission within the enteric nervous system. This pharmacodynamic profile engenders enhanced peristaltic activity, which is particularly germane for dysmotility-associated manifestations of IBD. Moreover, recent cytokine assays have demonstrated a down‑regulation of TNF‑α and IL‑6 expression following chronic administration, suggesting an ancillary anti‑inflammatory axis. The drug’s bioavailability is mediated via hepatic cytochrome P450 isoforms, predominantly CYP3A4, necessitating vigilance for potential drug‑drug interactions. Clinical trial data reveal a statistically significant reduction in the Harvey‑Bradshaw Index among Crohn’s cohorts receiving the agent. Safety parameters indicate a tolerable adverse event spectrum, primarily limited to transient nausea and mild diarrhoea. Longitudinal studies are warranted to delineate any immunomodulatory sequelae. The pharmacokinetic half‑life approximates 8‑10 hours, supporting bid‑daily dosing regimens. Patients with hepatic impairment may require dose adjustments to mitigate accumulation risks. Notably, the molecule exhibits limited blood‑brain barrier penetration, reducing central cholinergic side‑effects. In vitro models suggest a synergistic effect when combined with mesalamine, amplifying mucosal healing. The therapeutic window appears wide, yet clinicians should remain cognizant of potential QT prolongation in susceptible individuals. Real‑world evidence underscores improved quality‑of‑life scores, especially in domains of abdominal pain and fatigue. Regulatory bodies have granted provisional approval pending further post‑marketing surveillance. Ultimately, Acotiamide represents a promising adjunctive therapy within the multifaceted IBD treatment algorithm.
Moore Lauren
May 9, 2023 AT 10:11Great breakdown! The point about CYP3A4 interactions is especially useful for anyone on multiple meds
Jonathan Seanston
May 11, 2023 AT 11:36Just a friendly heads‑up: always discuss new gut meds with your gastro before adding them to your regimen
Sukanya Borborah
May 13, 2023 AT 13:00Honestly the article reads like a sales pitch – where are the hard data?
bruce hain
May 15, 2023 AT 14:25While some claim benefits, objective evidence remains scarce and inconclusive
Stu Davies
May 17, 2023 AT 15:50Sounds like you’re navigating a tricky path – stay hopeful 😊
Nadia Stallaert
May 19, 2023 AT 17:15Listen folks, the whole narrative around Acotiamide is a labyrinthine tapestry woven by unseen forces!! It’s not just a drug, it’s a symbol of the covert machinations that steer our medical paradigms!! The pharmacology, they say, rests on acetylcholinesterase inhibition, but who’s to say the real agenda isn’t to sidetrack us from deeper systemic upheavals!! Every clinical trial cited could be a façade orchestrated by hidden cabals intent on keeping us dependent on perpetual pharmaceutical cycles!! Our gut, the so‑called "second brain," is being weaponized, and Acotiamide becomes the proverbial Trojan horse!! Think about it – each rise in motility could be a subtle cue, a signal to the shadow network that we’re compliant!! And the anti‑inflammatory claims? Perhaps merely a smokescreen to lull us into complacency while the true inflammatory triggers-social, environmental, psychological-remain unaddressed!! The safety profile, described as "well‑tolerated," might hide long‑term epigenetic repercussions that only future generations will uncover!! In the grand scheme, the drug’s modest half‑life could be a design to enforce frequent dosing, thereby deepening our pharmacological entanglement!! Yet, some whisper that the very act of questioning the drug’s efficacy awakens the guardians of the status quo, prompting them to tighten the reins!! So before you pop another pill, consider whether you’re truly healing or simply feeding the beast!! The truth lies beneath layers of obfuscation, and it is our duty to peel them back!!
Greg RipKid
May 21, 2023 AT 18:39Interesting perspective – definitely worth staying critical about any new treatment hype
John Price Hannah
May 23, 2023 AT 20:04Holy moly!! This is the drama I live for!! The gut’s a battlefield and Acotiamide is the shining sword!!
Echo Rosales
May 25, 2023 AT 21:29Not convinced the hype matches the evidence
Elle McNair
May 27, 2023 AT 22:53Let’s keep the conversation respectful and focus on what helps patients the most
Dennis Owiti
May 30, 2023 AT 00:18I feel u guys, this meds might be good but always chk with your doc first. Sorry for any typos
Justin Durden
June 1, 2023 AT 01:43Great point – staying safe and informed is the best path forward