When it comes to poison prevention, the practice of avoiding accidental or intentional exposure to harmful substances that can cause injury or death. Also known as toxic exposure control, it’s not just about keeping cleaning products out of reach—it’s about understanding how everyday medications can turn dangerous if misused, mixed, or taken in error. Every year, thousands of people end up in emergency rooms because of something as simple as taking two pills at once or splashing a cleaner in their eye. Most of these incidents are preventable.
Drug overdose, the accidental or intentional intake of a medication in excess of the recommended dose. Also known as medication toxicity, it’s one of the leading causes of injury-related death in the U.S. Think of levocetirizine or butylscopolamine—both are common prescriptions. Take too much, and you risk severe drowsiness, irregular heartbeat, or even breathing failure. The same goes for mixing MAOIs with cold medicine or fluoroquinolones with NSAIDs. These aren’t rare edge cases. They’re documented, life-threatening interactions that show up in real patient records. And they happen because people don’t know what’s in their medicine cabinet—or how it reacts with other things.
Chemical eye injury, damage to the eye from contact with corrosive substances like acids, alkalis, or solvents. Also known as ocular chemical burn, it’s one of the fastest ways to lose vision if you delay action. A splash from drain cleaner or even some eye drops can cause permanent harm in under a minute. That’s why immediate flushing for 20 minutes isn’t optional—it’s the difference between sight and blindness. And it’s not just chemicals. Some medications, like those causing photosensitivity, turn your skin and eyes into targets for UV damage. Sunscreen alone won’t cut it if you’re on a drug that makes you burn faster.
Poison prevention isn’t about fear. It’s about awareness. It’s reading the FDA Medication Guide that comes with your prescription. It’s knowing that generic drugs aren’t always interchangeable, especially with narrow therapeutic index drugs where tiny changes in blood levels can trigger toxicity. It’s realizing that herbal supplements like green tea extract or turmeric can cause liver damage just like prescription drugs. And it’s understanding that long-term care insurance won’t cover your meds—Medicare Part D might, but only if they’re on the formulary.
You don’t need to be a pharmacist to stay safe. You just need to know what to look for: the Boxed Warning on labels, the interaction warnings on the bottle, the signs of overdose before it’s too late. The posts below give you real, practical guidance on exactly that—how to spot risks before they happen, what to do when something goes wrong, and how to make sure your medicine works for you, not against you.
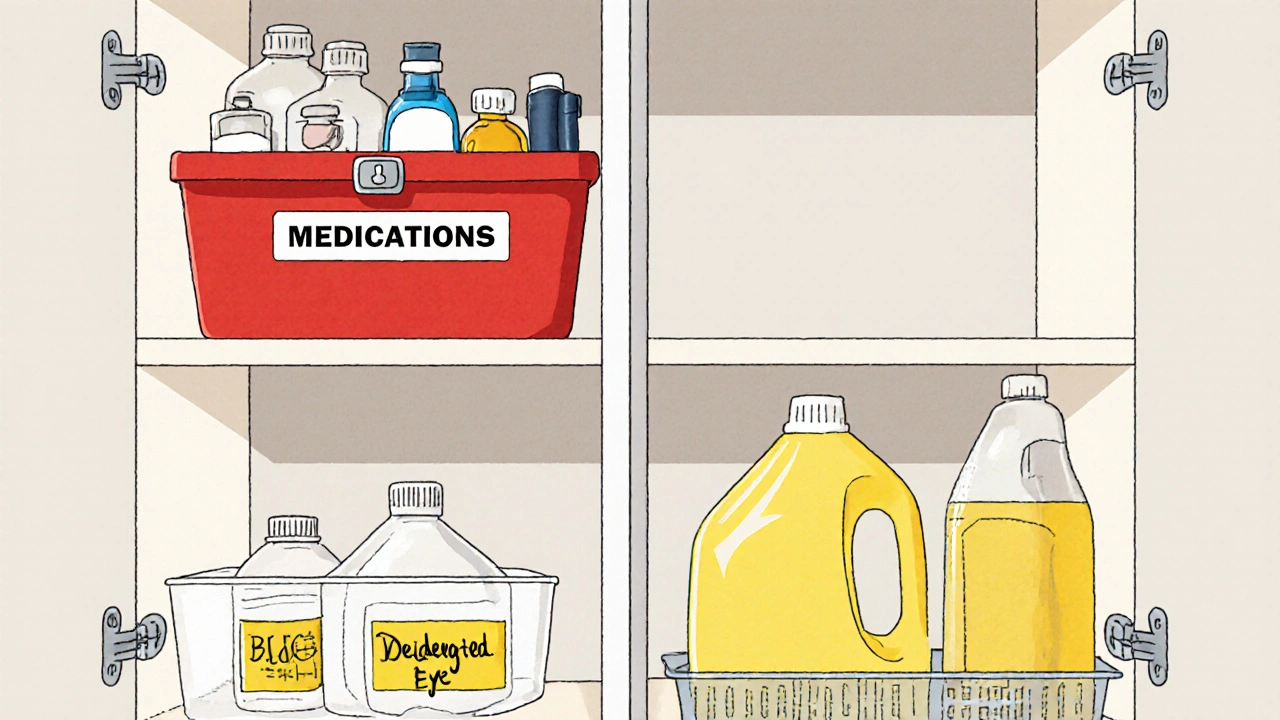
Learn how to safely store medications away from household chemicals to prevent accidental poisoning, protect medicine effectiveness, and keep your family safe. Simple steps for every home.