Music can change your breathing, your mood, and even how much pain you feel. That's not just a nice idea — trained music therapists use songs, instruments, and guided listening to reach real medical goals like less anxiety, improved speech after a stroke, and calmer behavior in dementia.
Music therapy is a clinical practice led by a credentialed therapist. They use two main approaches: active (you play or sing) and receptive (you listen with intention). Sessions target measurable goals — for example, lowering heart rate during panic attacks, improving left-hand movement after a stroke, or reducing agitation in dementia wards. Clinical trials and controlled studies show consistent benefits for mood, anxiety, and certain rehab outcomes, though results vary by condition and program.
Typical sessions last 30–60 minutes. A therapist assesses your needs, picks music and activities, and measures progress over several weeks. Therapists often work with your doctor, speech therapist, or rehab team to fit music into an overall plan instead of replacing medicine or physical therapy.
If you have chronic pain, short guided-listening sessions during flare-ups can lower perceived pain and reduce opioid needs for some people. If anxiety or insomnia is the issue, try slow-tempo playlists synced to 5–7 minutes of deep breathing. For stroke recovery, rhythmic exercises (like tapping to a beat) help retrain motor timing and are commonly used in clinic-based programs.
For caregivers of people with dementia: familiar songs from the person’s youth often spark memories, reduce agitation, and improve engagement. Use short, predictable playlists and avoid sudden loud changes. Singing together can also help with swallowing and speech in people with neurological injury — therapists adapt songs to match comfortable pitch and breathing.
At home, start simple. Build three playlists: calming (slow, steady rhythms), energizing (upbeat but not chaotic), and familiar (songs tied to positive memories). Use headphones at safe volumes and limit sessions to 10–20 minutes at first. Notice changes in mood, sleep, or pain and share them with your clinician.
Safety matters. Music can trigger strong emotions; if someone has PTSD, psychosis, or severe depression, work with a trained therapist. Also protect hearing — keep volume moderate and stop if dizziness or ear pain appears.
Questions to ask a music therapist: What certification do you hold? Which conditions do you treat? How will progress be measured? Can this work alongside my medications or rehab plan? A short trial (2–4 sessions) usually shows whether it helps.
Music therapy won't replace medication when you need it, but it often improves outcomes and quality of life when used with standard care. If you want practical, low-cost ways to start, try tailored playlists and breathing exercises — and consider a professional if you need targeted recovery or behavioral support.
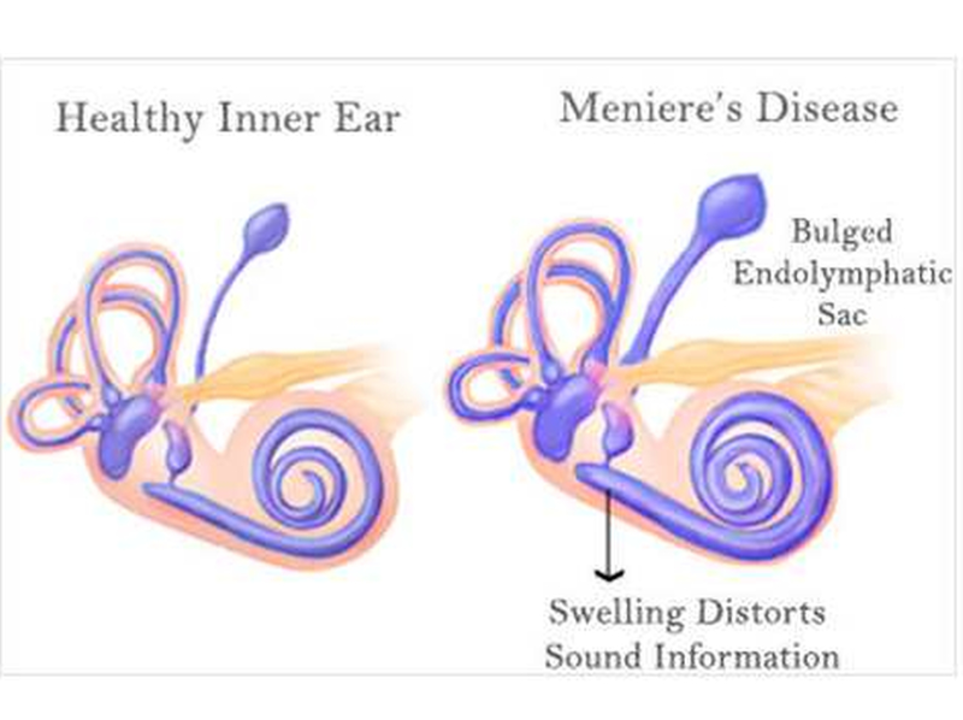
As a blogger, I recently came across a fascinating topic – Meniere's Disease and the role of music therapy in its treatment. Meniere's Disease is a debilitating condition that affects the inner ear, causing vertigo, tinnitus, and even hearing loss. I discovered that music therapy has been proven to be a promising complementary treatment for Meniere's patients. Through sound, it can alleviate the emotional stress associated with the disease while also helping to promote relaxation and well-being. I strongly believe in the therapeutic power of music and I am thrilled to share this breakthrough with my readers.