Meniere's disease causes sudden vertigo attacks, hearing changes, tinnitus and a feeling of fullness in the ear. If you're getting spinning spells that come with hearing loss or buzzing, Meniere's is one possible cause to explore with a doctor. It's not contagious and it usually affects one ear at first, though both ears can be involved over time.
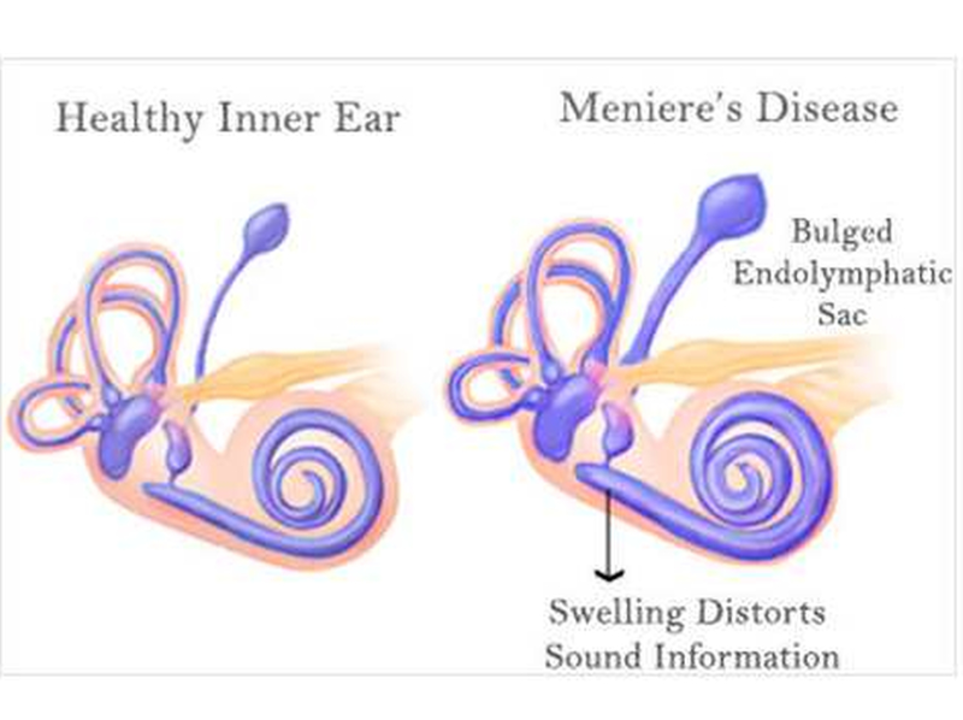
Doctors think Meniere's results from abnormal fluid buildup in the inner ear. That fluid messes with balance signals and sound processing. We don't have a single clear cause—factors like viral infection, immune response, allergies or head injury might play a role. Genetics can matter for some people, too.
Typical symptoms include: sudden vertigo that lasts 20 minutes to several hours, fluctuating low-frequency hearing loss, ringing (tinnitus), and ear pressure. Attacks can be severe and leave you nauseous or unable to stand. Between attacks many people feel unsteady or have lasting hearing changes. A doctor will ask about attack patterns, do hearing tests, and may order balance tests or MRI to rule out other problems.
There's no cure, but several treatments help control attacks and protect hearing. Doctors often start with lifestyle changes: cut salt to reduce fluid buildup, avoid caffeine and nicotine, and limit alcohol. During attacks, resting in a quiet, dark room and using anti-nausea or vertigo meds can help. Diuretics sometimes reduce fluid, and steroid or gentamicin injections into the middle ear are options for persistent cases. Surgery is rare but available if symptoms are disabling and other treatments fail.
Balance rehab (vestibular therapy) teaches your brain to cope with inner ear changes. Hearing aids help when hearing loss becomes stable. Manage stress—anxiety can make symptoms worse—try breathing exercises and stable sleep routines. Keep a symptom diary noting what you ate, sleep, stress and weather to find your triggers.
Practical safety tips matter: avoid driving or climbing during severe attacks; sit or lie down as soon as spinning starts. If you must move, go slowly and hold stable surfaces. Tell family or coworkers about your condition so they know how to help during an attack. Wear shoes with good grip and keep home lighting even to reduce falls.
When to see a doctor: get urgent care if a first attack is severe, if symptoms include double vision or numbness, or if hearing drops quickly. For ongoing care, work with an ENT (ear, nose and throat) specialist who knows Meniere's disease. They'll tailor treatment to your attack pattern and hearing goals.
At work, tell HR or your manager about accommodation needs like flexible breaks or remote days during flare-ups; simple changes — moving heavy tasks away from expected attack times and using supportive chairs — lower risk and keep you productive daily.
Living with Meniere's can be unpredictable, but many people find a mix of lifestyle changes, medication and therapy that makes life manageable. Track your symptoms, stay connected with a specialist, and build a simple plan so you can act fast when an attack starts.
As a blogger, I recently came across a fascinating topic – Meniere's Disease and the role of music therapy in its treatment. Meniere's Disease is a debilitating condition that affects the inner ear, causing vertigo, tinnitus, and even hearing loss. I discovered that music therapy has been proven to be a promising complementary treatment for Meniere's patients. Through sound, it can alleviate the emotional stress associated with the disease while also helping to promote relaxation and well-being. I strongly believe in the therapeutic power of music and I am thrilled to share this breakthrough with my readers.