When you take a pill, it doesn’t just disappear—it enters your bloodstream, travels to where it’s needed, and eventually leaves your body. This whole process is called drug levels, the concentration of a medication in your blood over time. Also known as plasma concentration, it’s not just a number on a lab report—it’s what decides if your medicine works, causes side effects, or becomes dangerous. Too low, and it won’t help. Too high, and it can hurt you. That’s why doctors sometimes check drug levels, especially for meds like lithium, digoxin, or certain antibiotics.
Drug levels are tied to something called pharmacokinetics, how your body absorbs, distributes, metabolizes, and gets rid of a drug. This isn’t the same for everyone. Age, liver health, kidney function, and even what else you’re taking can change how fast or slow a drug builds up in your system. For example, mixing drug interactions, when two or more medicines affect each other’s behavior in your body like MAOIs and cold meds can spike drug levels dangerously. Or taking fluoroquinolones with NSAIDs can push kidney stress beyond safe limits, even if each drug is fine alone.
There’s a sweet spot called the therapeutic range, the blood concentration where a drug works best without causing harm. For some drugs, like epilepsy meds or antidepressants, staying in this range means fewer seizures or better mood control. For others, like antibiotics, it’s about killing bacteria without wrecking your gut or kidneys. That’s why you can’t just double up on a pill if you don’t feel better—your drug levels might already be at risk.
Some meds need close monitoring because their therapeutic range is narrow. Others? Not so much. That’s why you’ll see drug level checks for drugs like warfarin or cyclosporine, but not for your daily ibuprofen. But even common drugs can build up if you have kidney trouble or take them with other meds that slow clearance. That’s why posts here talk about things like butylscopolamine tapering, levodopa clashes with antipsychotics, or why fluconazole dosing matters in immune-compromised patients. It’s all connected to how your body handles the medicine.
Understanding drug levels isn’t about memorizing numbers. It’s about knowing why timing, dose, and combinations matter. It’s why you shouldn’t skip doses, why alcohol can make some pills more toxic, and why your doctor might ask for blood tests months after you started a new med. The posts below show real cases—how drug levels affect Parkinson’s treatment, why certain antibiotics can damage nerves, how steroids like dexamethasone behave differently than prednisone, and why mixing OTC cold meds with MAOIs can land you in the ER. You’ll see how these concepts play out in actual treatment decisions, not just theory.
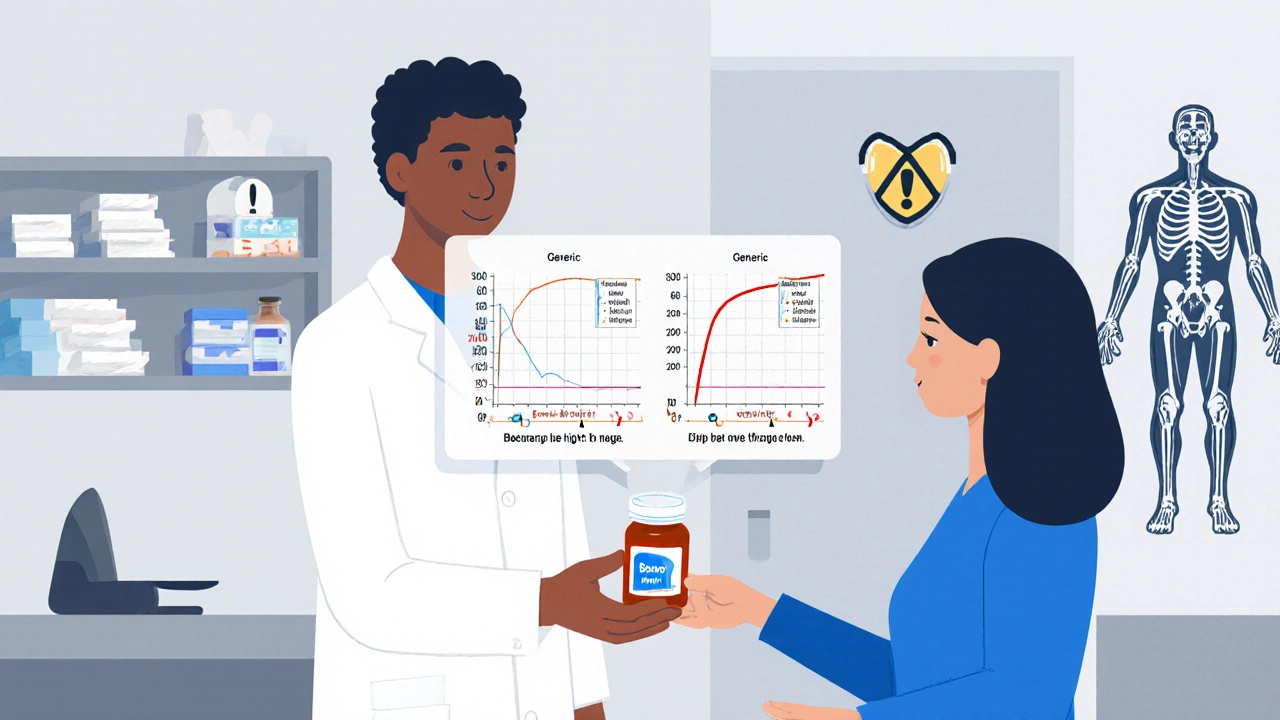
Therapeutic Drug Monitoring is critical for patients on generic narrow therapeutic index (NTI) drugs, where small changes in blood levels can cause toxicity or treatment failure. Learn when and why TDM saves lives.