Statin intolerance isn’t rare - but it’s often misdiagnosed
If you’ve been told you can’t take statins because of muscle pain, you’re not alone. But here’s the thing: statin intolerance is way more complicated than it sounds. Most people who think they’re intolerant aren’t actually reacting to the drug - they’re reacting to fear, coincidence, or something else entirely.
The National Lipid Association’s 2022 definition is clear: true statin intolerance means you couldn’t tolerate two different statins - one at the lowest dose, another at any dose - because of symptoms that went away when you stopped the medication. It’s not just one bad experience. It’s a pattern.
And here’s what most doctors don’t tell you: 72 to 85% of patients labeled as statin-intolerant don’t actually have statin-related muscle symptoms. Their pain comes from osteoarthritis, vitamin D deficiency, fibromyalgia, or just aging. A study published in CCJM found that people had the same muscle aches on placebo as they did on statins. That’s the nocebo effect in action - your brain expecting side effects so badly, it makes you feel them.
What do real statin muscle symptoms actually feel like?
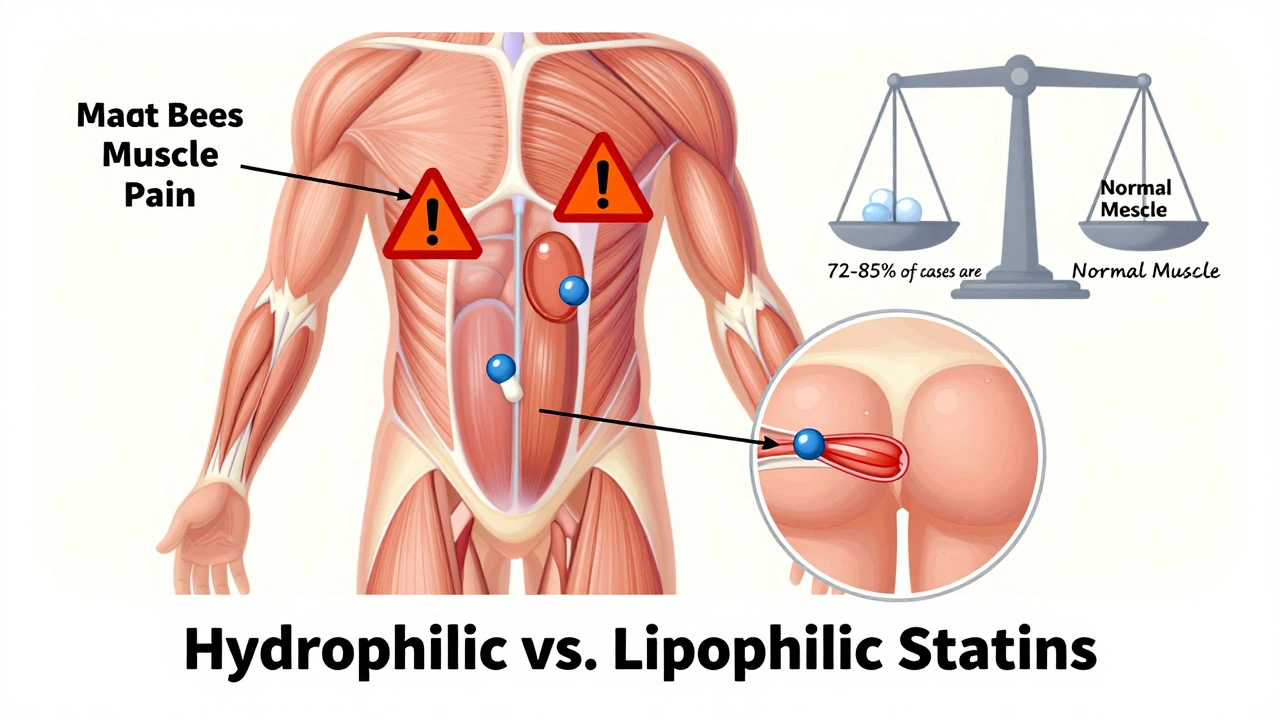
When statins do cause muscle issues, it’s not sharp pain. It’s not a pulled muscle. It’s a deep, heavy feeling - like your legs are filled with wet sand. You might feel stiffness when standing up from a chair, or struggle to raise your arms. The pain is usually in both sides at once: thighs, buttocks, back, shoulders. The PRIMO study found 78% of cases hit the thighs, 65% hit the buttocks.
These symptoms show up fast - 83% of people notice them within 30 days of starting or increasing a statin. But here’s the key: if you had muscle pain before you started the statin, it’s not statin-related. That’s a common mistake. People blame the pill for pain they’ve had for years.
And don’t panic about blood tests. Most people with statin-related muscle symptoms have normal or only slightly elevated creatine kinase (CK) levels. True muscle damage - like myositis or rhabdomyolysis - is extremely rare. The FDA says there are only about 300 to 500 cases of rhabdomyolysis per year among 200 million statin users worldwide. That’s less than one in 400,000.
Why you might be able to take statins after all
Many people give up after one bad experience. But here’s the truth: 65% of people who can’t tolerate one statin can handle another. It’s not about the whole class - it’s about the specific molecule.
Hydrophilic statins like pravastatin and rosuvastatin are less likely to cause muscle issues because they don’t penetrate muscle tissue as easily. Lipophilic statins like simvastatin and atorvastatin do. In head-to-head trials, hydrophilic statins showed 28% lower intolerance rates.
Even better: low doses work better than you think. A 10mg daily dose of atorvastatin reduces LDL by about 32% and is tolerated by 89% of people who couldn’t handle higher doses. You don’t need to max out the dose to get results.
And if you’re on a drug that interferes with statin metabolism - like some antibiotics, antifungals, or grapefruit juice - that’s often the real culprit. A medication review can clear up 22% of so-called intolerance cases.
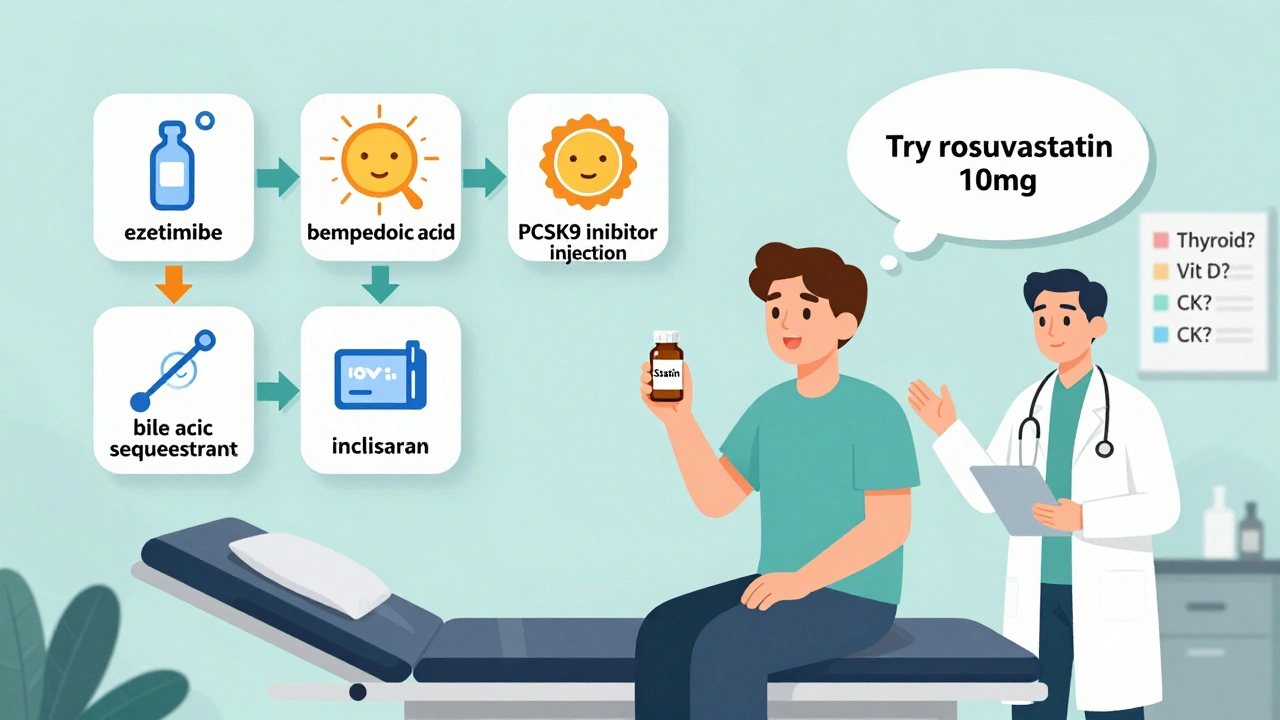
What to try when statins really won’t work
If you’ve truly tried two statins and still have symptoms, there are effective alternatives. You don’t have to give up on lowering your cholesterol.
- Ezetimibe (10mg daily): Reduces LDL by 18%, taken alone or with a low-dose statin. It’s well-tolerated - 94% of people stick with it after a year. No muscle pain. No major side effects.
- Bempedoic acid (180mg daily): Works in the liver like statins but doesn’t enter muscle cells. Lowers LDL by 17%, with 88% tolerability. It’s newer, but data shows it’s safe and effective.
- PCSK9 inhibitors (evolocumab, alirocumab): Injected every two weeks, these cut LDL by nearly 60%. They’re not for everyone - cost is high, and insurance often requires prior authorization. But for high-risk patients with genetic cholesterol disorders, they’re life-changing.
- Bile acid sequestrants (colesevelam): Pills that bind cholesterol in the gut. Lower LDL by 15-18%, but can cause bloating or constipation in 22% of users.
- Inclisiran: A twice-yearly injection that silences a gene involved in cholesterol production. In trials, it lowered LDL by 50% with 93% adherence. It’s not yet widely available, but it’s coming fast.
Most patients who switch to alternatives need 3 to 6 months to find the right combo. On average, people try 2.3 different treatments before hitting their target LDL level. That’s normal. Don’t get discouraged.
Supplements and myths: What actually helps?
Coenzyme Q10 is often recommended for statin muscle pain. The theory? Statins lower CoQ10, and that might cause fatigue or soreness. But the evidence? Weak. In double-blind trials, only 34% of people reported any benefit. And if you’re not on a statin, CoQ10 won’t help your muscle aches.
Same goes for vitamin D. If your level is below 20 ng/mL, correcting it can reduce muscle pain - but only if you were deficient to begin with. About 29% of people labeled as statin-intolerant have low vitamin D. That’s not a coincidence. It’s a clue.
Don’t waste money on fish oil or garlic pills for cholesterol. They don’t move the needle enough to matter for high-risk patients. Stick to proven therapies.
What you should do next
Step 1: Don’t stop your statin without talking to your doctor. Stopping increases your risk of heart attack or stroke by 25%. That’s a huge trade-off for symptoms that might not even be from the pill.
Step 2: Ask for a full workup. Check your thyroid, vitamin D, and CK levels. Rule out arthritis, fibromyalgia, or other causes.
Step 3: Try a different statin. Switch to rosuvastatin or pravastatin at the lowest dose. Wait 6 weeks. Many people are surprised at how well they feel.
Step 4: If symptoms return, consider a supervised re-challenge. Only 34% of people who think they’re intolerant actually have symptoms come back when they try the statin again. That means two out of three people were misdiagnosed.
Step 5: If all statins fail, work with your doctor on a non-statin plan. Ezetimibe + bempedoic acid is a powerful combo. PCSK9 inhibitors are an option if you’re high-risk and insurance approves.
Why this matters more than you think
Every year, 45-60% of statin prescriptions are stopped within 12 months. Muscle pain is the #1 reason. But research shows that when people stop statins for the wrong reasons, their risk of heart disease jumps.
The economic cost? About $1,800 more per patient per year in avoidable hospital visits and procedures. And the human cost? Anxiety. Fear. Feeling like your body betrayed you.
The good news? With better diagnosis and better alternatives, over 90% of people previously labeled as statin-intolerant can reach their cholesterol goals. You’re not stuck. You just need the right approach.
What’s on the horizon
By 2025, genetic testing for the SLCO1B1 gene variant could become routine. People with the *5 or *15 allele have a 4.5 times higher risk of muscle side effects. Knowing this before starting a statin could prevent unnecessary stops.
Oral PCSK9 inhibitors like MK-0616 are in late-stage trials. If approved, they could replace injections with a daily pill. And new myoprotective drugs like IMOD3001 are being tested to prevent muscle damage without lowering cholesterol.
This isn’t science fiction. It’s happening now. The tools are here. The knowledge is here. You just need to ask the right questions.

Bruno Janssen
December 12, 2025 AT 21:40Scott Butler
December 14, 2025 AT 19:01Tyrone Marshall
December 15, 2025 AT 04:59Emily Haworth
December 15, 2025 AT 22:57Tom Zerkoff
December 16, 2025 AT 23:20kevin moranga
December 17, 2025 AT 18:15Alvin Montanez
December 19, 2025 AT 13:29Lara Tobin
December 20, 2025 AT 05:03Keasha Trawick
December 22, 2025 AT 04:01Deborah Andrich
December 22, 2025 AT 07:52Tommy Watson
December 23, 2025 AT 23:24Donna Hammond
December 24, 2025 AT 16:20Richard Ayres
December 26, 2025 AT 15:20