When a drug leaves the lab and heads to pharmacies, hospitals, or your medicine cabinet, it needs to stay safe and effective for months or even years. That’s where stability testing comes in. It’s not optional. It’s a legal requirement. And at the heart of every stability study are two non-negotiable factors: temperature and time.
Why Temperature and Time Matter in Stability Testing
Drugs aren’t static. They change. Heat, moisture, and light can break them down. A painkiller might lose potency. An antibiotic could turn toxic. A biologic therapy might clump together and stop working. Stability testing catches these changes before patients get harmed. The goal is simple: figure out how long a drug lasts under real-world conditions and what temperature it should be stored at. This isn’t guesswork. It’s science backed by global rules. These rules come from ICH Q1A(R2), a guideline created in 2003 by regulators from the U.S., Europe, and Japan. It’s the same standard used by the FDA, EMA, Health Canada, and most major markets today. If you don’t follow it, your drug won’t get approved. And if it’s already on the market and fails, you could face a recall - like the 150,000 vials Teva pulled in 2021 because their stability testing missed aggregation issues.Core Temperature and Time Conditions
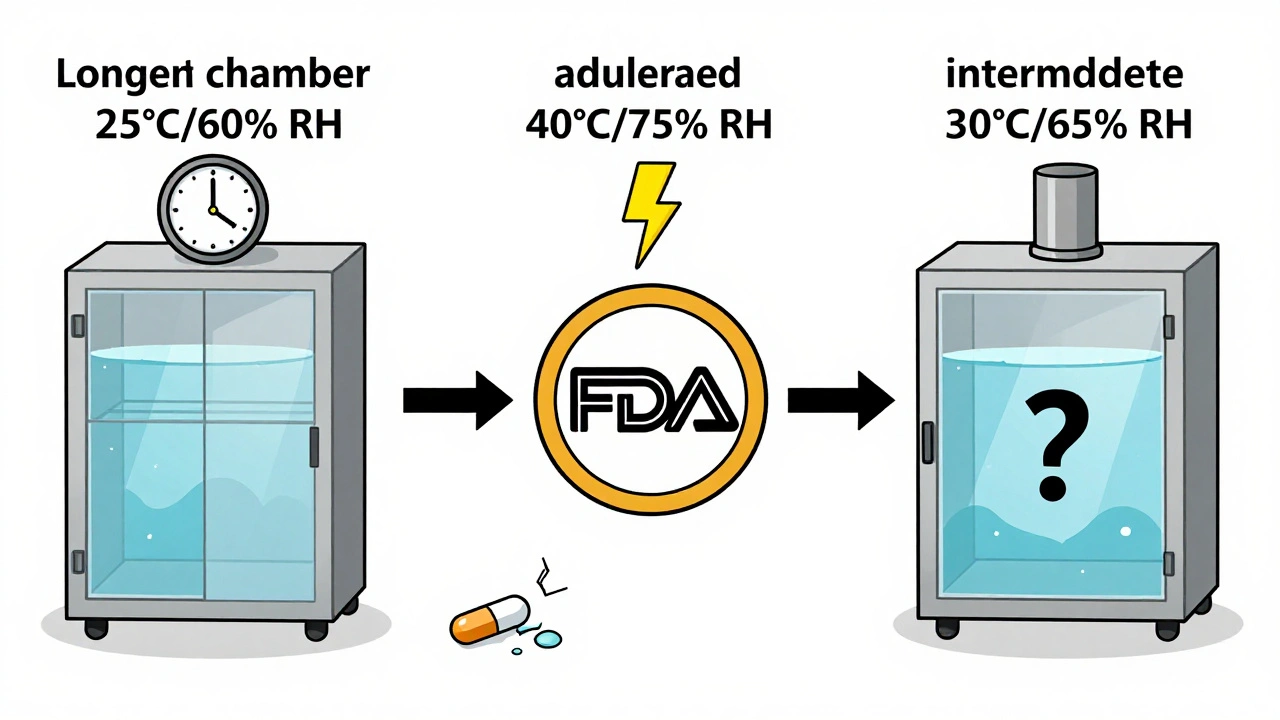
There are three main types of stability tests, each with fixed temperature and time rules.- Long-term testing is the gold standard. It runs for years and simulates real storage. The two approved conditions are: 25°C ± 2°C with 60% RH ± 5% RH or 30°C ± 2°C with 65% RH ± 5% RH. You pick one based on where your product will be sold. For example, if you’re targeting tropical markets, you’d use 30°C/65% RH. This test must have at least 12 months of data when you submit your drug for approval in the U.S. (FDA requires this). Europe lets you submit with 6 months, but you’ll need to finish the full 12 later.
- Accelerated testing is the speed round. It’s done at 40°C ± 2°C with 75% RH ± 5% RH for 6 months. This isn’t meant to predict exact shelf life - it’s a stress test. If your drug breaks down here, you know you’ve got a problem. It’s designed to catch degradation faster. The science behind it? A 6-month test at 40°C roughly mimics 24 months at 25°C for 85% of small-molecule drugs. But it fails for hygroscopic (moisture-loving) compounds - and that’s where things get messy.
- Intermediate testing is the backup. You only run this if your accelerated test shows a problem and your long-term test is at 25°C. It’s done at 30°C ± 2°C with 65% RH ± 5% RH for 6 months. Think of it as a middle ground to confirm whether the accelerated results are real or just noise.
Refrigerated drugs - like insulin or some vaccines - follow different rules. Their long-term storage is at 5°C ± 3°C for 12 months. Accelerated testing for these is done at 25°C/60% RH, not 40°C. That’s because freezing and thawing can ruin biologics, and 40°C would destroy them.
Global Variations and Climatic Zones
The world isn’t one climate. That’s why ICH breaks it down into five zones.- Zone I (Temperate): 21°C / 45% RH
- Zone II (Mediterranean/Subtropical): 25°C / 60% RH
- Zone III (Hot-Dry): 30°C / 35% RH
- Zone IVa (Hot-Humid/Tropical): 30°C / 65% RH
- Zone IVb (Hot/Higher Humidity): 30°C / 75% RH
If you’re selling a drug in India or Brazil (Zone IVa), your long-term test must match 30°C/65% RH. But if you’re only selling in Canada or Germany (Zone I), you might use 25°C/60% RH. This creates complexity. Companies targeting global markets often run multiple parallel studies. One study from Tovatech in 2023 found this adds 4-6 months to development timelines.
And here’s the catch: humidity control isn’t just about setting a dial. Chambers must hold ±2% RH. Temperature must stay within ±0.5°C. In real labs, 78% of professionals report at least one temperature excursion over ±2°C during a 12-month study. One spike can invalidate the whole test.
What Counts as a ‘Significant Change’?
The ICH guidelines say a drug has failed if there’s a “significant change” in any of these:- Assay (potency) changes by more than 5%
- Any impurity exceeds its specification limit
- Physical appearance changes - color, texture, dissolution rate
But here’s the problem: “significant change” isn’t defined with exact math. It’s open to interpretation.
One Pfizer analyst shared a story on Reddit: a drug’s assay dropped to 95.2% from 100%. The specification was 95-105%. Statistically, it was fine. But the regulator said it was a failure. Why? Because they saw a trend. That’s the gray zone. Companies spend months arguing with inspectors over what counts as a “change.”
And it’s not just about numbers. A tablet that cracks, a liquid that clouds, or a capsule that sticks together - these are physical changes. They’re just as important as chemical ones. A 2022 AAPS paper found 62% of failures in solid oral drugs came from humidity cycling, not constant high humidity. That’s something standard testing doesn’t always catch.
Real-World Challenges and Pitfalls
Setting up a stability lab isn’t plug-and-play. It takes weeks just to qualify a chamber - IQ (Installation Qualification), OQ (Operational Qualification), PQ (Performance Qualification). And even then, temperature varies across shelves. One study found differences up to ±1.8°C from top to bottom. That’s enough to skew results.Humidity control is another headache. In dry climates like Arizona or Adelaide, keeping 60% RH in a chamber means adding moisture. In humid places, you need to remove it. Dual-loop systems help, cutting RH variation from ±8% to ±3%. But they cost money.
Then there’s the waiting. Long-term studies take years. A drug candidate might sit in a chamber for 18 months before you know if it’s stable. That delays launches. In a CPT Labs survey, 67% of respondents said stability issues held up at least one product launch.
And biologics? They’re a whole different ballgame. Monoclonal antibodies, mRNA vaccines, gene therapies - they’re sensitive. A freeze-thaw cycle can ruin them. The ICH Q1A(R2) guidelines weren’t written for these. That’s why Amgen and Roche got FDA warning letters in 2021-2022. Their stability protocols didn’t account for real-world handling.
What’s Changing? The Future of Stability Testing
The rules haven’t changed much since 2003. But science has.Companies are now using predictive modeling. Run tests at 50°C, 60°C, even 80°C - then use software to predict how the drug behaves at 25°C. Some top pharma firms say this cuts time-to-market by 9-12 months. But regulators are skeptical. EMA rejected 8 model-based submissions between 2022 and 2023.
The FDA is testing real-time stability using process analytical technology (PAT). Imagine sensors in the manufacturing line tracking drug quality as it’s made. That could replace some long-term testing for continuous manufacturing products.
And ICH is working on Q1F - a new update expected in late 2024. It’s meant to cover complex drugs like antibody-drug conjugates and cell therapies. The current rules just don’t fit.
By 2030, McKinsey predicts 60% of stability data might come from modeling, not physical testing. But until regulators fully trust the math, you still need the chambers, the data logs, and the 12-month shelf life study.
What You Need to Do
If you’re developing a drug, here’s your checklist:- Choose your target markets. That determines your long-term storage condition (25°C/60% RH or 30°C/65% RH).
- Run accelerated testing at 40°C/75% RH for 6 months. If it fails, you’ve got a problem.
- If your long-term test is at 25°C and accelerated failed, run intermediate testing at 30°C/65% RH for 6 months.
- For refrigerated products, use 5°C for long-term and 25°C/60% RH for accelerated.
- Calibrate your chambers. Map temperature and humidity across all shelves. Document everything.
- Test at 0, 3, 6, 9, 12, 18, 24, and 36 months. More often early on if degradation is expected.
- Define “significant change” in your protocol - and be ready to defend it.
Stability testing isn’t glamorous. It’s slow. It’s expensive. It’s repetitive. But it’s the last line of defense between a patient and a bad drug. Get it right, and you protect lives. Get it wrong, and you risk recalls, fines, and worse.
What are the standard temperature and humidity conditions for long-term stability testing?
The ICH Q1A(R2) guidelines allow two options: 25°C ± 2°C with 60% RH ± 5% RH, or 30°C ± 2°C with 65% RH ± 5% RH. The choice depends on the climatic zone of the target market. For example, tropical markets require 30°C/65% RH, while temperate regions use 25°C/60% RH. At least 12 months of data must be available at submission for U.S. approval.
Why is accelerated testing done at 40°C and 75% RH?
The 40°C/75% RH condition is designed to accelerate degradation and identify potential stability issues within 6 months. It represents extreme but plausible environmental stress - like a drug left in a hot warehouse or shipped without climate control. This condition was chosen because it’s above typical storage temperatures but below the melting point of most drug excipients. Studies show this 6-month test roughly predicts 24 months of stability at 25°C/60% RH for 85% of small-molecule drugs.
What happens if a drug fails stability testing?
If a drug shows a significant change - such as potency dropping below 95%, impurities exceeding limits, or physical changes like discoloration or clumping - it’s considered unstable. Regulatory agencies like the FDA can issue warning letters, block approval, or order a recall. For example, Teva recalled 150,000 vials of Copaxone® in 2021 after stability testing failed to detect aggregation at 40°C.
Do refrigerated drugs follow the same stability rules?
No. Refrigerated products - like insulin or certain vaccines - are tested at 5°C ± 3°C for long-term storage. Their accelerated test is done at 25°C ± 2°C and 60% RH ± 5% RH, not 40°C. This is because freezing and thawing cycles, not heat, are the main risks for biologics. Testing at 40°C would destroy these products and give misleading results.
Is the ICH Q1A(R2) guideline still current in 2025?
Yes. ICH Q1A(R2) from 2003 remains the official global standard for stability testing of small-molecule drugs. While updates are in progress - including a proposed Q1F guideline for complex products like biologics and cell therapies - no replacement has been adopted yet. All major regulators, including the FDA and EMA, still require compliance with Q1A(R2) for new drug submissions.
How long does a full stability study take?
A full long-term stability study takes at least 12 months to complete, but most run for 24-36 months to establish shelf life. Accelerated testing takes 6 months. Intermediate testing, if needed, adds another 6 months. Because testing starts at the beginning of development and runs in parallel with other studies, companies often begin stability testing years before a drug hits the market. Delays in stability data are one of the top reasons for late-stage launch delays.


Audrey Crothers
December 13, 2025 AT 03:01Just had to say-this post saved my butt at work. We were about to submit a stability package and missed the 30°C/65% RH requirement for our tropical market. Now we’re fixing it before the FDA tears us apart. 🙏
Adam Everitt
December 15, 2025 AT 02:05so… like… temp and humidy? yeah. i mean, drugs are just chemistrey right? and chemistrey hates heat. so… yeah. 40c for 6 mths? makes sense. i think. 🤷♂️
wendy b
December 16, 2025 AT 10:59It is frankly astonishing that anyone still relies on ICH Q1A(R2) in 2025. The guidelines were drafted before smartphones were ubiquitous, let alone before the advent of mRNA therapeutics. The notion that a 25°C/60% RH chamber can meaningfully predict the stability of a lipid nanoparticle is not just outdated-it’s scientifically negligent. We are still operating under a framework designed for aspirin tablets. The regulatory inertia here is not just frustrating-it’s dangerous.
Nathan Fatal
December 17, 2025 AT 16:51Let’s cut through the noise. The real issue isn’t the temperature settings-it’s the lack of real-world humidity cycling in most protocols. Labs run constant 60% RH, but in the real world, a pill bottle in a bathroom in Florida goes from 20% RH in the morning to 90% by night. That’s what causes cracking, deliquescence, and degradation. The 2022 AAPS paper nailed it: 62% of solid-dose failures came from humidity swings, not steady-state conditions. We need to redesign our protocols to simulate real life, not a controlled closet.
nikki yamashita
December 18, 2025 AT 06:43YES. This is the stuff no one talks about but everyone deals with. Keep pushing for better testing. We got this 💪
sandeep sanigarapu
December 18, 2025 AT 13:48Respectfully, the global harmonization of stability conditions remains a challenge. In India, we often face power fluctuations and ambient temperatures exceeding 40°C for weeks. The 30°C/65% RH standard is still too conservative. Perhaps we need a Zone IVc for regions with extreme ambient stress? A pragmatic approach may be more useful than rigid adherence.
Robert Webb
December 19, 2025 AT 16:33I’ve been in stability labs for over 15 years, and I can tell you the most underappreciated part isn’t the chambers or the specs-it’s the documentation. Every temperature excursion, every humidity drift, every calibration log needs to be timestamped, signed, and archived. One time, a 0.8°C spike at 14 months nearly got our entire submission rejected because the technician forgot to initial the log sheet. Regulators don’t care about your science if your paperwork is sloppy. You can have perfect data, but if your QMS isn’t bulletproof, you’re still in trouble. It’s not glamorous, but it’s the difference between approval and a 6-month delay.
Rob Purvis
December 20, 2025 AT 02:52And don’t forget: the 40°C/75% RH accelerated test? It’s a great screen, but it’s not a crystal ball. I’ve seen drugs pass it with flying colors-then fail at 18 months under 25°C because of a subtle polymorphic shift that only showed up after slow moisture uptake. The real danger is assuming accelerated = predictive. It’s not. It’s a warning light, not a full diagnostic. That’s why intermediate testing exists-and why you need to look at the whole picture, not just the headline numbers.