Every year, millions of people take SSRIs to manage depression, anxiety, or OCD. These medications work by boosting serotonin in the brain - a chemical that helps regulate mood. But what most people don’t realize is that taking an SSRI with another common medication can trigger something dangerous: serotonin syndrome.
What Is Serotonin Syndrome?
Serotonin syndrome isn’t just a side effect. It’s a medical emergency. It happens when too much serotonin builds up in your nervous system, usually because two or more drugs that increase serotonin are taken together. Symptoms can start within hours and escalate fast: muscle stiffness, high fever, rapid heartbeat, confusion, shaking, or even seizures. In severe cases, it can be fatal.The good news? Most cases are mild and reversible if caught early. The bad news? Many doctors miss it. Symptoms often look like the flu, food poisoning, or even a panic attack. That’s why knowing the triggers is critical.
Which SSRIs Are Most Likely to Cause Problems?
Not all SSRIs are the same when it comes to serotonin syndrome risk. Fluoxetine (Prozac) sticks around in your body for weeks - its active metabolite can last up to 15 days. That means even if you stop taking it, the risk lingers. Paroxetine (Paxil) is the strongest serotonin reuptake blocker, making it more likely to cause issues when mixed with other drugs. Sertraline (Zoloft) and escitalopram (Lexapro) are commonly prescribed because they’re generally well-tolerated, but they still carry risk when combined with other serotonergic agents.The key isn’t just which SSRI you’re on - it’s what else you’re taking.
High-Risk Drug Combinations
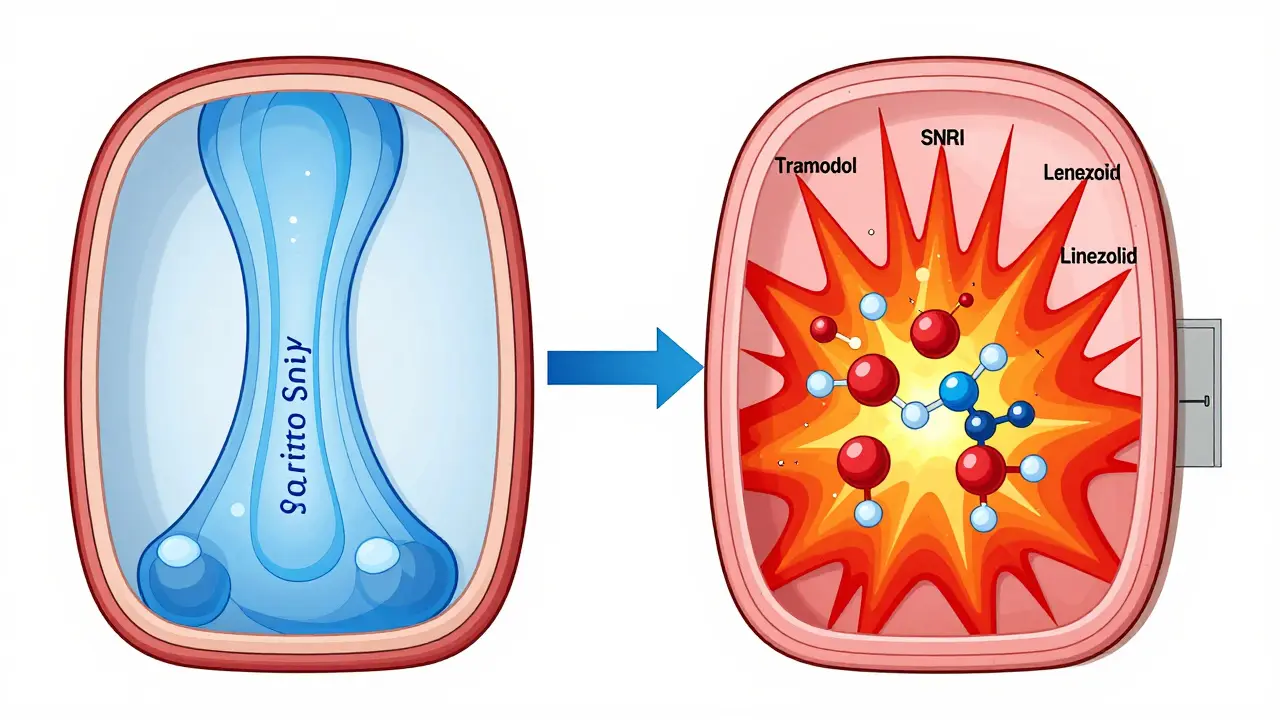
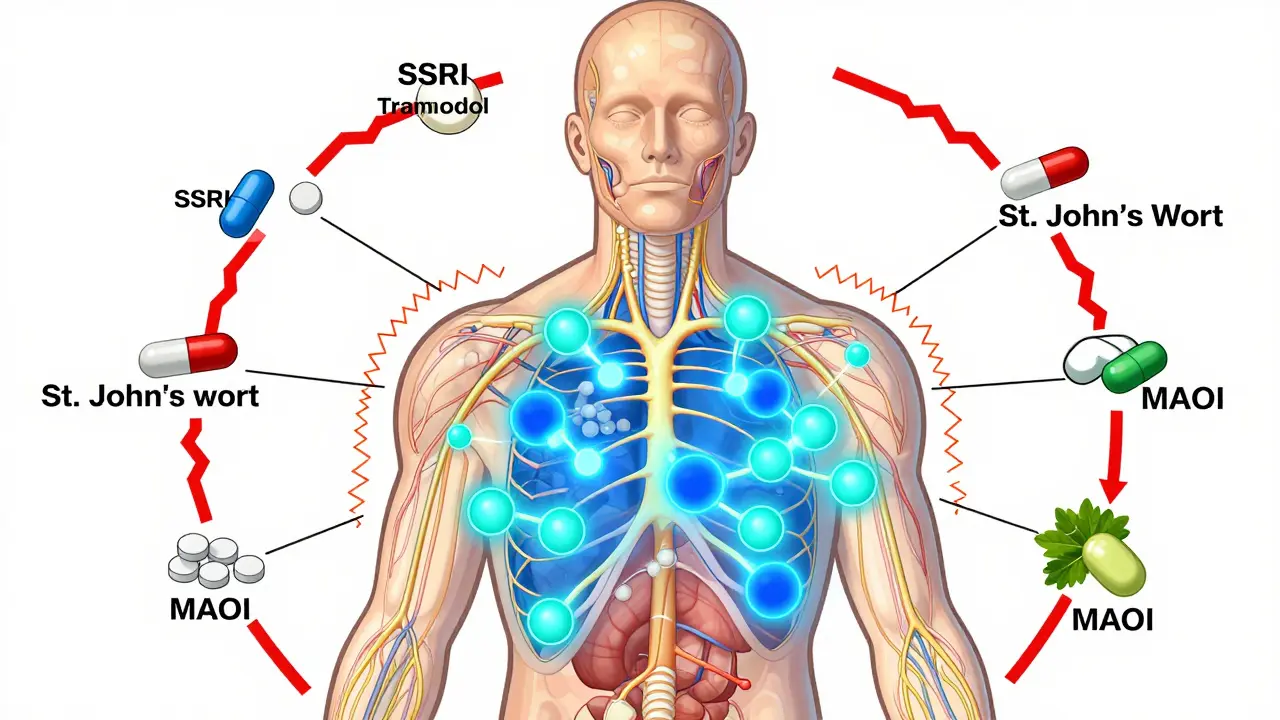
Here’s where things get dangerous. Certain medications, even those prescribed for common conditions, can turn an SSRI into a ticking time bomb.- SNRIs like venlafaxine (Effexor) or duloxetine (Cymbalta): Combining these with SSRIs increases serotonin syndrome risk by more than three times.
- Tramadol, dextromethorphan, and pethidine: These painkillers and cough medicines are sneaky offenders. Tramadol, in particular, is often prescribed for chronic pain, but when taken with an SSRI, it raises the risk nearly fivefold.
- Linezolid: This antibiotic is used for tough infections like MRSA. It’s an MAOI, which means it blocks serotonin breakdown. Even a short 5-day course can trigger serotonin syndrome in someone on an SSRI.
- MAOIs like phenelzine or selegiline: Never, ever combine these with SSRIs. The interaction can be deadly, with mortality rates between 30% and 50%.
- St. John’s wort: This popular herbal supplement for mild depression is a serotonin booster. People think it’s “natural,” so it’s safe - but it’s just as risky as prescription drugs when mixed with SSRIs.
- Mirtazapine, trazodone, buspirone: These are sometimes added to SSRIs to boost mood or help with sleep. But they also increase serotonin, and together they can push you over the edge.
Even opioids like methadone and fentanyl carry a moderate risk. But morphine, oxycodone, and buprenorphine? Studies show they don’t significantly raise serotonin levels when used with SSRIs. If you need pain relief while on an SSRI, these are safer choices.
Who’s Most at Risk?
It’s not just about the drugs - it’s about who’s taking them. Older adults are the most vulnerable. Nearly 22% of Americans over 65 are on an SSRI, and more than 18% are also taking opioids for chronic pain. Many are on five or more medications. Each new drug adds another layer of risk.People with liver problems are also at higher risk. The liver breaks down SSRIs and other serotonergic drugs. If your liver is slow to process them - due to age, disease, or genetics - serotonin builds up faster. A genetic variation in the CYP2D6 enzyme (found in about 7% of people) makes it harder to metabolize tramadol and some SSRIs, increasing the chance of toxicity.
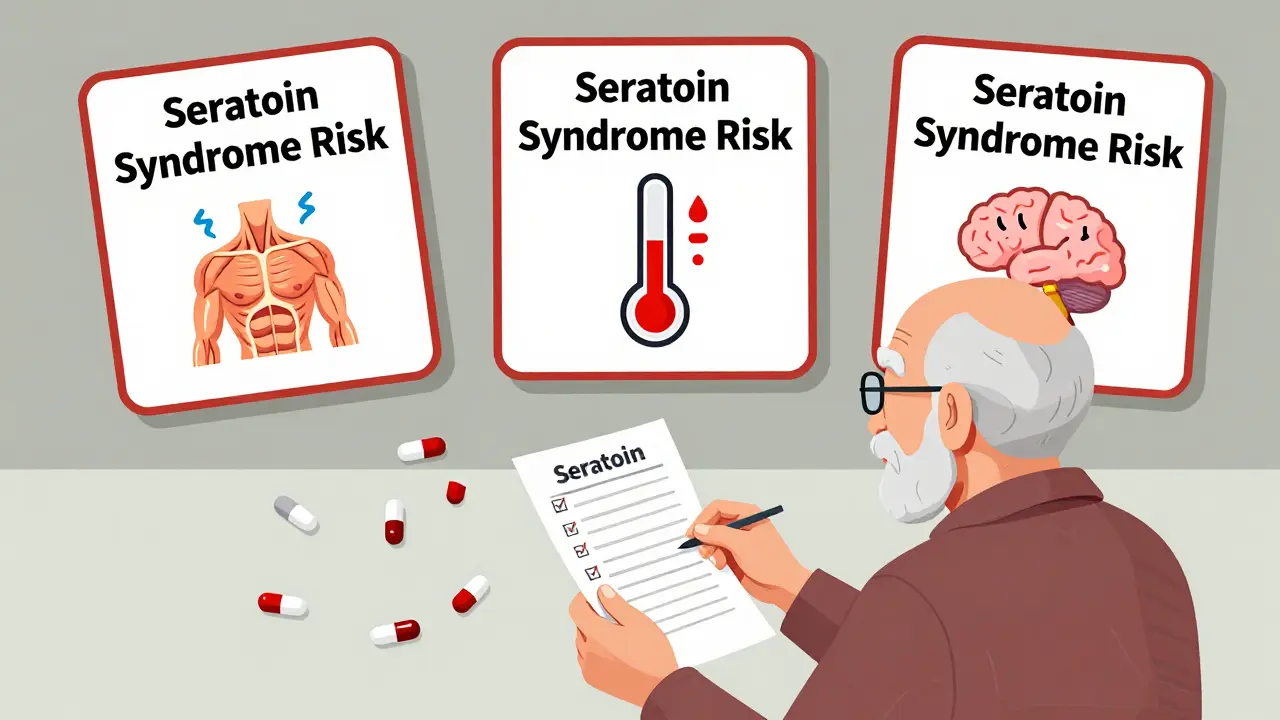
What to Watch For: The 5 S’s
If you’re on an SSRI and start a new medication, pay attention to these signs - especially in the first few days:- Shivering - not from being cold, but uncontrollable tremors.
- Sweating - drenching sweats without exertion.
- Stiffness - muscles that feel rigid, especially in the legs or jaw.
- Seizures - rare, but a red flag when they happen.
- Sudden confusion - feeling disoriented, agitated, or hallucinating.
If you have at least one of these plus a fever above 38°C (100.4°F) or clonus (involuntary muscle spasms), seek emergency care immediately. The Hunter Criteria, used by ER doctors, are the gold standard for diagnosis - and they’re accurate 84% of the time.
What Should You Do?
If you’re taking an SSRI:- Don’t start any new medication, supplement, or herb without talking to your doctor or pharmacist. That includes over-the-counter cough syrups with dextromethorphan.
- Know your meds. Keep a written list of everything you take - including doses and why. Bring it to every appointment.
- Ask about alternatives. If you need pain relief, ask if oxycodone or morphine is an option instead of tramadol.
- Wait before switching. If you’re switching from one antidepressant to another, especially from fluoxetine, wait at least 5 weeks. For other SSRIs, wait 2 weeks. Never overlap MAOIs with SSRIs.
- Trust your gut. If something feels off - like sudden muscle tightness or confusion - don’t wait. Go to the ER.
Pharmacists are your best allies here. A 2023 study found that pharmacist-led medication reviews cut serotonin syndrome risk by nearly half in older patients. They catch interactions doctors miss.
Technology Is Helping - But Not Enough
Electronic health records now have alerts for dangerous combinations. One system reduced risky SSRI-opioid prescriptions by 32% across 200 hospitals. That’s progress. But alerts can be ignored, overridden, or missed entirely - especially in busy clinics.The FDA is pushing for mandatory alerts in all e-prescribing systems by 2026. That’s a step forward. But the real solution is better communication between prescribers, pharmacists, and patients.
Real Stories, Real Risks
One Reddit user, on the r/SSRI subreddit, described going to the ER after taking tramadol with sertraline. Within 12 hours, their body temperature hit 104.2°F. They had muscle rigidity and involuntary leg movements. They were hospitalized for three days. Another person on Drugs.com started taking St. John’s wort with Prozac. Three days later, they were shaking uncontrollably and confused. The ER doctor said it was early serotonin syndrome. These aren’t rare cases. Between 2018 and 2022, over 1,800 serotonin syndrome reports were filed with the FDA - 68% involved drug combinations. And that’s just the ones that were reported.What’s Next?
Researchers are working on a blood test called SerotoninQuant that could measure serotonin levels directly. It’s still in trials, but if it works, it could change how we diagnose this condition - no more guessing based on symptoms.In the meantime, the message is simple: SSRIs are safe when used alone. But when layered with other drugs, the risk skyrockets. You don’t need to avoid treatment. You just need to be informed.
If you’re on an SSRI, don’t assume your doctor knows every medication you’re taking. Don’t assume herbal supplements are harmless. And don’t wait for symptoms to get worse before acting.
Can you get serotonin syndrome from one SSRI alone?
Rarely. Serotonin syndrome almost always happens when two or more serotonergic drugs are combined. Overdosing on a single SSRI can cause it, but that’s uncommon. Most cases involve mixing medications - like an SSRI with tramadol, St. John’s wort, or an MAOI.
How long after stopping an SSRI is it safe to start an MAOI?
It depends on the SSRI. For most, wait at least 2 weeks. But for fluoxetine (Prozac), wait 5 weeks because it stays in your system so long. Never start an MAOI without clearing it with your doctor first.
Are all opioids dangerous with SSRIs?
No. Tramadol, dextromethorphan, and pethidine are high-risk. Methadone and fentanyl are moderate. But morphine, oxycodone, and buprenorphine show no significant increase in serotonin syndrome risk when used with SSRIs. Always ask your doctor which painkiller is safest for you.
Can I take melatonin or CBD with an SSRI?
Melatonin is generally safe with SSRIs - no strong evidence links it to serotonin syndrome. CBD is trickier. It can interfere with how your liver processes SSRIs, potentially increasing levels in your blood. Talk to your doctor before combining them, especially if you’re on a high dose of SSRI.
What should I do if I think I have serotonin syndrome?
Stop all serotonergic medications immediately and go to the emergency room. Do not wait. Early treatment - stopping the drugs, giving fluids, and using medications like cyproheptadine - can save your life. Delaying care increases the risk of organ failure or death.
Is serotonin syndrome common?
It’s not common in the general population - about 0.5 to 1.5 cases per 1,000 people per year. But among those taking multiple serotonergic drugs, the risk jumps dramatically. Underdiagnosis is a big problem, so the real number is likely higher.
Final Thoughts
SSRIs changed how we treat depression. They’re safer than older antidepressants. But they’re not risk-free - especially when combined with other drugs. The problem isn’t the SSRI. It’s the cocktail.If you’re on one, don’t be afraid. But be aware. Keep a list of every pill, patch, or supplement you take. Ask your pharmacist to review it. Speak up if something feels wrong. Your life might depend on it.

James Rayner
December 15, 2025 AT 11:25Wow. This is the kind of post that makes you pause mid-sip of coffee. I’ve been on sertraline for years and had no idea tramadol was a ticking time bomb. My dad’s on it for back pain - gonna print this out and hand it to him. He thinks ‘natural’ means safe. 😅
Kayleigh Campbell
December 15, 2025 AT 12:31So let me get this straight - St. John’s wort is basically a sneaky SSRI in a bottle with a sunflower on it? 🌻 No wonder my aunt went from ‘calm’ to ‘human tornado’ after adding it to her Prozac. Natural ≠ harmless. Always.
Ron Williams
December 15, 2025 AT 22:36As someone who’s worked in rural clinics for 15 years, I’ve seen this play out too many times. Elderly patients on 7 meds, no pharmacist review, just ‘take this, take that.’ The system’s broken. We need mandatory med reviews before adding anything new - especially for folks over 65. This isn’t just medical advice. It’s public health.
Aditya Kumar
December 16, 2025 AT 05:40Too much info. I’ll just stop taking meds.
Andrew Sychev
December 16, 2025 AT 21:50Of course you’re telling people to ‘trust their gut’ - because clearly, the entire medical system is just a bunch of clueless idiots who can’t read a drug interaction chart. If you can’t remember your own meds, maybe you shouldn’t be allowed to leave the house. This isn’t rocket science. It’s basic pharmacology. Why are we even having this conversation?
Kitty Price
December 17, 2025 AT 10:21Thank you for this. I started CBD oil last month for anxiety and was worried. Now I know to talk to my pharmacist before anything else. 🙏
Mike Smith
December 18, 2025 AT 16:39Let me be clear: This is not fear-mongering. This is life-saving education. If you’re on an SSRI, you are not ‘just fine.’ You are one interaction away from a hospital stay. Please, for your own sake - keep a written list. Ask your pharmacist. Don’t assume. Don’t guess. Your life matters.
Souhardya Paul
December 19, 2025 AT 16:26I’m from India, and here, people buy SSRIs over the counter with zero guidance. I’ve seen friends mix fluoxetine with painkillers because ‘it’s just a little extra.’ This post should be mandatory reading in every pharmacy, every clinic, every school. Knowledge is the only real protection.
Josias Ariel Mahlangu
December 20, 2025 AT 21:07People need to stop being so careless with their bodies. If you can’t manage your own medications, why are you even allowed to drive? This isn’t a ‘medical mystery’ - it’s negligence dressed up as convenience.
anthony epps
December 22, 2025 AT 06:21so if i take morphine and sertraline its safe? just making sure
Arun ana
December 22, 2025 AT 12:21My mom’s on Lexapro and just started melatonin for sleep. I showed her this post. She said, ‘I thought that was just for jet lag.’ Now she’s printing it out to take to her doctor. Thank you for making this so clear.
Dan Padgett
December 23, 2025 AT 06:04Back in Lagos, my cousin took Prozac and then a ‘traditional tonic’ for ‘mental strength’ - three days later, he was in ICU. No one told him the tonic had kola nut, yohimbine, and something called ‘spirit root.’ He survived, but his body still shakes sometimes. This isn’t just Western medicine stuff. It’s global. We need better education everywhere - not just in the US.
sue spark
December 24, 2025 AT 15:06Billy Poling
December 25, 2025 AT 17:19While I appreciate the intent behind this article, I must respectfully point out that the reliance on anecdotal Reddit and Drugs.com reports as primary evidence undermines the scientific rigor expected in clinical communication. The FDA Adverse Event Reporting System (FAERS) is inherently biased due to voluntary reporting, and the cited 1,800 cases represent only a fraction of potential incidents. Furthermore, the assertion that pharmacists reduce risk by nearly half is derived from a single 2023 observational study with limited generalizability. A more robust conclusion would require randomized controlled trials and standardized diagnostic criteria across diverse populations. Until then, while the warnings are prudent, they should be contextualized within the broader epidemiological landscape to avoid therapeutic nihilism or unnecessary medication discontinuation.