When a spinal cord is injured, it doesn’t just hurt-it changes everything. The nerves that carry signals between your brain and body get damaged, and suddenly, movements you took for granted-standing, walking, gripping a cup, even controlling your bladder-become uncertain or impossible. This isn’t just about paralysis. It’s about losing control over your own body, and then learning how to live again. Every year, around 17,810 people in the U.S. face this reality, mostly from car crashes, falls, or violence. But here’s the truth: recovery isn’t about going back to how things were. It’s about rebuilding a new normal.
What Happens When the Spinal Cord Is Damaged?
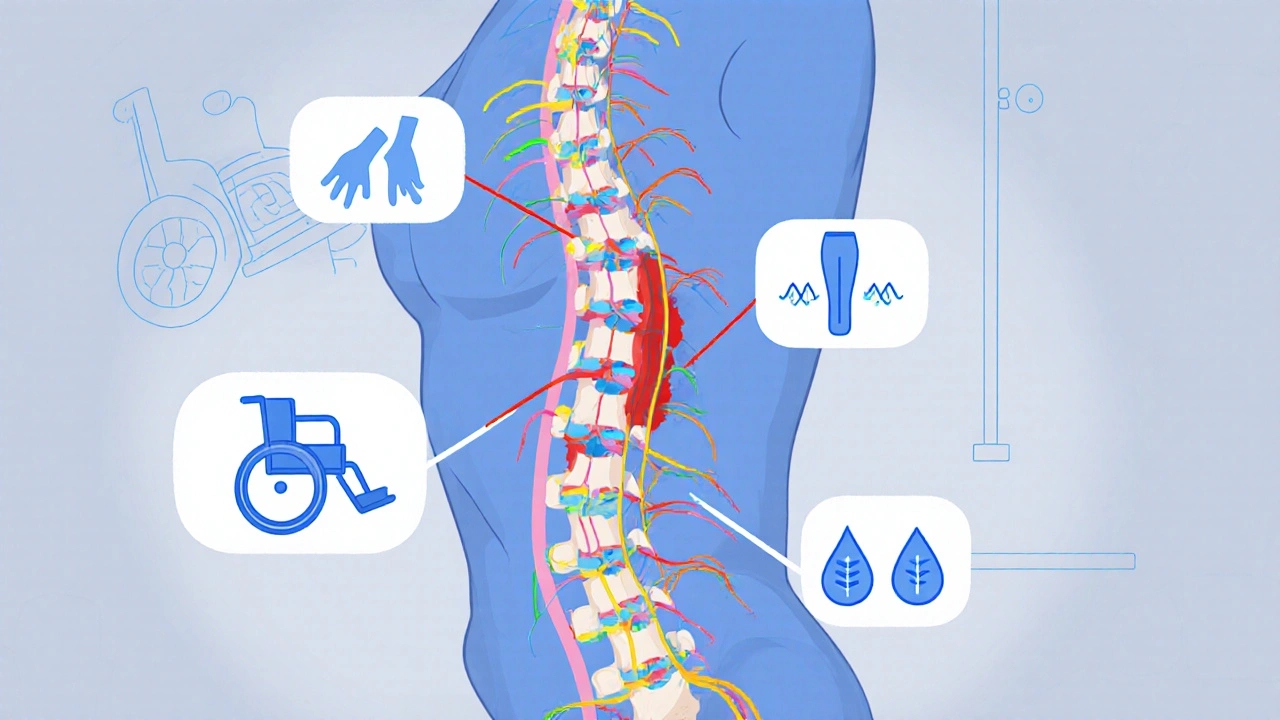
The spinal cord is like a thick cable full of nerves that send messages from your brain to your muscles, skin, and organs. When it’s injured, those messages get blocked. The higher the injury on the spine, the more functions are affected. A C1-C4 injury can mean you can’t breathe on your own. A T12 injury might leave your legs paralyzed but keep your arms and hands fully functional. Injuries are classified as complete or incomplete. Complete means no feeling or movement below the injury. Incomplete means some signals still get through. About 59% of people with incomplete injuries regain some walking ability within a year. For complete injuries, that number drops to just 1-3%. That doesn’t mean hope is gone-it just means the path looks different. Beyond movement, you lose control over things like temperature, blood pressure, bowel, and bladder function. These are called autonomic functions, and they’re often the hardest to adjust to. One person described it as “living with a body that doesn’t listen anymore.”Rehabilitation Starts the Day You’re Stabilized
Rehab doesn’t wait. It begins within 24 to 72 hours after the injury, as soon as the patient is medically stable. The goal isn’t just to prevent complications-it’s to build skills that last a lifetime. Early rehab focuses on keeping joints flexible. If you’re lying still for days, your muscles tighten, your tendons shorten, and your shoulders and elbows lock up. Physical therapists do passive range-of-motion exercises-moving your limbs for you-at least once a day, sometimes three times if you’re spastic. This isn’t just busywork. It prevents permanent contractures. Breathing is another critical focus, especially for injuries above C5. Without proper care, pneumonia becomes a real threat. Therapists teach assisted coughing, use percussion (gentle clapping on the chest), and give incentive spirometers to help you take deep breaths. Studies show these simple tools cut pneumonia rates by 65% in high-level injuries. You’ll also learn how to sit, transfer from bed to wheelchair, and handle daily tasks like dressing and bathing. Occupational therapists work with you to adapt your environment-raising your sink, installing grab bars, or switching to long-handled reachers. Every skill is practiced until it becomes automatic. Most inpatient programs require at least three hours of therapy, five days a week. Teams include doctors, nurses, physical and occupational therapists, psychologists, social workers, and speech therapists. You’re not just a patient-you’re part of a system designed to get you back into life.Assistive Devices: Tools That Restore Independence
Assistive devices aren’t just gadgets-they’re lifelines. For someone with a C6 injury, a powered wheelchair with sip-and-puff control might be the difference between needing constant help and living alone. For someone with a T10 injury, a standing frame or exoskeleton can mean the difference between sitting all day and standing during a family gathering. Here are the most common devices and how they work:- Wheelchairs: Manual chairs are lighter and more portable, but power chairs are essential for those with limited arm strength. Custom seating systems prevent pressure sores and cost $1,200-$3,500 out-of-pocket after insurance.
- Functional Electrical Stimulation (FES) Bikes: These machines send tiny electric pulses to paralyzed leg muscles, making them cycle. Studies show they boost heart health better than arm cycling-increasing oxygen use by 14.3% in users.
- Robotic Exoskeletons: Devices like Ekso and ReWalk let people with paraplegia stand and walk with support. One user said it was the first time he stood next to his daughter in three years. But these machines need two or three therapists to operate safely, and sessions are limited to 30-45 minutes because they’re exhausting.
- Powered Upper Limb Exoskeletons: Armeo helps people with arm weakness relearn reaching and grasping. It’s used in rehab centers and sometimes at home.
- Implantable Diaphragm Pacing Systems: Approved by the FDA in 2022, these devices stimulate the diaphragm in people with C3-C5 injuries, reducing ventilator use by 74%.

What Works Best? Evidence Behind the Methods
Not all rehab is created equal. Some methods have strong proof behind them. Others are flashy but lack long-term data. Treadmill training with body weight support has been shown to improve walking speed 23% more than regular walking practice. Why? It rewires the brain. The repetitive motion activates the spinal cord’s own walking circuits, even without brain input. It’s not magic-it’s neuroplasticity. For spasticity-those painful muscle spasms that affect 65-78% of people with SCI-doctors use a mix of oral meds like baclofen and injections of Botox into tight muscles. One study found this combo reduced spasticity scores by 40-60% in 78% of patients. But here’s the catch: many new technologies, like advanced exoskeletons and brain-computer interfaces, haven’t been tested long enough. Only 37% of studies track patients beyond six months. That means we don’t know if the gains last. And while AI-driven therapy plans are becoming common in top centers, they’re not yet standard. Only 65% of leading rehab hospitals use them, and most insurance plans won’t pay for them.The Human Side: What Patients Really Say
Behind every statistic is a person trying to get through the day. One man on Reddit said his Ekso exoskeleton gave him his first steps in three years-but he only got 25 minutes of use per session. “It felt amazing,” he wrote, “but I left frustrated because I wanted more.” Another user on the Christopher & Dana Reeve Foundation forum shared that FES cycling helped him keep his leg muscles from wasting away-but he couldn’t afford the home unit. “I did it at the clinic, but I stopped when I couldn’t get there anymore.” Peer support makes a huge difference. At Spaulding Rehabilitation, 82% of patients said talking to someone who’d been through it helped them adjust emotionally more than any therapy session. That’s why many centers now pair new patients with mentors who’ve lived with SCI for years. The biggest reason people quit home exercises? Lack of motivation and no follow-up. Sixty-eight percent stop within six months. That’s not laziness-it’s isolation. Rehab doesn’t end when you leave the hospital. It just changes shape.
What Comes Next? The Future of SCI Recovery
The field is changing fast. In 2022, the FDA approved the first implantable device that lets people with high-level injuries breathe without a ventilator. In 2023, early trials of brain-computer interfaces showed a 38% improvement in hand movement for people with cervical injuries. That’s not science fiction-it’s happening now. New tools like the Tethered Pelvic Assist Device (TPAD) are helping people learn balance while standing. AI is being used to personalize rehab plans based on how your body responds in real time. By 2025, most top centers will use these systems. But money is still a wall. Medicare covers only 83% of actual rehab costs. Many centers operate at a loss. And with the population aging, falls are rising-especially in people over 65. The number of SCI cases from falls is growing by 4.2% every year. The real challenge isn’t just technology. It’s access. Only 32% of general hospitals offer full SCI rehab. Most people have to travel far for the care they need. And even then, insurance limits how long you can stay.You’re Not Alone in This
Spinal cord injury doesn’t just change your body. It changes your life. But it doesn’t have to end it. Thousands of people are living full lives-working, parenting, traveling, even competing in sports-after SCI. They didn’t get back to who they were. They became someone new. The key isn’t waiting for a cure. It’s building skills, using tools, finding support, and pushing through the hard days. Rehab is hard work. It’s messy. It’s frustrating. But it works-if you stick with it. If you or someone you know is facing this, start with the right team. Find a center that offers comprehensive care, not just physical therapy. Ask about peer support. Learn what devices are covered. And don’t let cost stop you from asking for help. There are programs, grants, and nonprofits that help cover what insurance doesn’t. Recovery isn’t a straight line. It’s a series of small victories. Standing for five minutes. Dressing yourself. Taking a walk with a walker. Those moments matter more than any statistic.Can you walk again after a spinal cord injury?
It depends on whether the injury is complete or incomplete. About 59% of people with incomplete injuries regain some ability to walk within a year, often with help from devices like exoskeletons or walkers. For complete injuries, only 1-3% regain walking ability. But even if you can’t walk, many people learn to stand, transfer, and move independently using wheelchairs, braces, or robotic aids.
How long does spinal cord injury rehab last?
Rehab starts within days of injury and continues for life. The first 6-12 weeks are intensive inpatient care, with three or more hours of therapy daily. After that, most people move to outpatient care for months or years. Even after formal rehab ends, ongoing therapy, home exercises, and checkups are needed to maintain strength, prevent complications, and adapt to changes.
What are the most effective assistive devices for SCI?
The most effective devices depend on the injury level. For lower-body paralysis, powered wheelchairs and robotic exoskeletons like Ekso or ReWalk help with mobility. For arm weakness, Armeo exoskeletons improve hand function. FES bikes maintain muscle and heart health. For high injuries, implantable diaphragm pacers reduce ventilator dependence. The best device is the one that fits your goals and lifestyle.
Is spinal cord injury rehab covered by insurance?
Medicare and most private insurers cover inpatient rehab if you meet criteria (like needing 3+ hours of therapy daily). Outpatient care and devices like wheelchairs are partially covered, but often leave large out-of-pocket costs. Exoskeletons and FES bikes are rarely covered fully. Many patients rely on grants, nonprofits, or state programs to fill the gap.
What’s the biggest challenge after SCI rehab ends?
Maintaining progress without professional support. Sixty-eight percent of people stop their home exercises within six months because they feel isolated, unmotivated, or lack follow-up. The biggest risk isn’t losing ability-it’s losing momentum. Regular check-ins, peer support, and home modifications are critical to staying healthy long-term.
Spinal cord injury doesn’t define you. But how you respond to it? That does.

stephen riyo
November 26, 2025 AT 16:24I just saw a guy in a power chair do a wheelie down the grocery aisle yesterday-no big deal, right? But I cried. Not because he was impressive, but because he looked so damn free. I’ve been sitting here thinking about how we treat people with SCI like broken machines that need fixing, when really they’re just living differently. Like, who even decided walking is the only valid way to move through life? 🤷♂️
Albert Guasch
November 28, 2025 AT 01:28It is imperative to underscore that the neuroplasticity-driven interventions outlined herein represent a paradigmatic shift in rehabilitative neuroscience. The evidence supporting functional electrical stimulation (FES) and body-weight-supported treadmill training demonstrates statistically significant improvements in gait efficiency, with p-values < 0.01 across multiple RCTs. Furthermore, the integration of AI-driven adaptive therapy protocols, though currently underutilized due to reimbursement constraints, holds immense promise for personalized neurorehabilitation. We must advocate for policy reform to ensure equitable access to these life-altering technologies.
Ginger Henderson
November 28, 2025 AT 19:38Okay but like… how many of these fancy devices are just expensive toys for rich people? I get it, exoskeletons are cool, but if I can’t even afford my insulin, why am I supposed to care about a $50k robot that makes me stand for 30 minutes? 😴
Bethany Buckley
November 29, 2025 AT 21:51How profound, really, that we’ve reduced the existential recalibration of post-SCI existence to a checklist of assistive technologies. 🤔 The body, once a vessel of autonomy, becomes a landscape of prosthetic dependencies-yet we celebrate the ‘victory’ of standing for five minutes as if it reclaims dignity. But dignity isn’t measured in watts or gait cycles. It’s in the quiet refusal to be defined by the brokenness others see. 🌿✨
Stephanie Deschenes
November 30, 2025 AT 20:21Just wanted to add-peer support is everything. I’ve been living with a T6 injury for 12 years. The first time I talked to someone who’d been through it, I stopped feeling like a medical case study. If you’re new to this, find a mentor. It’s free. It’s real. And it changes everything. You’re not alone, even when it feels like it.
Cynthia Boen
December 1, 2025 AT 06:42This whole post is just a fancy ad for rehab centers. Where’s the data on long-term depression rates? Or how many people quit therapy because they’re broke and tired? You talk about ‘small victories’ like they’re magic. Meanwhile, people are drowning in medical debt and isolation. Stop romanticizing struggle.
Jesús Vásquez pino
December 2, 2025 AT 22:50My cousin got hit by a drunk driver last year-C6 injury. They told him he’d never walk again. He’s now using an Ekso at his clinic twice a week. Doesn’t mean he’s cured. But he stands. He looks his niece in the eye while she’s 3 feet tall. That’s not a gadget. That’s a damn miracle. And yeah, it costs a fortune. But so does letting someone give up.
hannah mitchell
December 3, 2025 AT 21:00I read this while waiting for my mom’s PT appointment. She’s 72 and fell last month. I didn’t know SCI could happen to older folks too. Thanks for making me realize this isn’t just a young person’s thing. I’ll be asking more questions now.
Jaspreet Kaur
December 5, 2025 AT 18:36Life is not about walking or standing it is about feeling alive even if your body does not obey your mind the spirit remembers what the nerves forget
Gina Banh
December 6, 2025 AT 20:16Let’s be real-most of these devices are useless without consistent follow-up. I’ve seen too many people get a FES bike, use it once, then let it collect dust because no one checks in. The system gives you tools but abandons you after discharge. That’s not rehab. That’s a sales pitch with a clipboard.
Deirdre Wilson
December 7, 2025 AT 21:14I used to think ‘recovery’ meant getting back to normal. Now I know it’s like learning a new language-your body speaks differently, and you gotta learn to listen. The first time I used a reacher to grab my coffee cup without help? Felt like winning the lottery. Small stuff. Big joy.
Damon Stangherlin
December 8, 2025 AT 22:14Hey I just wanted to say thanks for this post. My bro got injured last year and I’ve been reading everything I can. The part about peer support? We found a mentor through Reeve Foundation and it saved us. He’s not cured but he’s living. And that’s what matters. I’ll never forget how he said ‘I didn’t lose my life, I just got a new one.’
Ryan C
December 10, 2025 AT 04:17Actually, the FDA didn’t approve the diaphragm pacing system in 2022-it was cleared under the 510(k) pathway, which is not the same as full approval. And the 74% reduction stat? That’s from a single-center pilot study with n=17. Also, ReWalk’s FDA clearance is for ‘ambulation assistance,’ not ‘walking.’ You’re overselling the tech. 🤓
Dan Rua
December 10, 2025 AT 21:02^This. I work in rehab tech sales. People get so hyped by the headlines, then when they find out insurance won’t cover the full system, they feel betrayed. We need better transparency-not just hype. The tools work, but the system is broken. Let’s fix that together.