When pancreatic cancer is caught early, survival rates jump from 3% to nearly 40%. But here’s the problem: most people don’t know they have it until it’s too late. The pancreas hides deep behind the stomach, and early warning signs are easy to ignore. They look like common issues-back pain, weight loss, indigestion. That’s why nearly 80% of cases are diagnosed at stage III or IV, when treatment options shrink and survival drops sharply.
What Are the Real Early Signs of Pancreatic Cancer?
There’s no single red flag for pancreatic cancer. Instead, it’s a mix of subtle, overlapping symptoms that often get written off as stress, aging, or a bad diet. If you’ve had two or more of these for more than a few weeks, it’s worth asking your doctor about pancreatic cancer-even if you’re young or otherwise healthy.
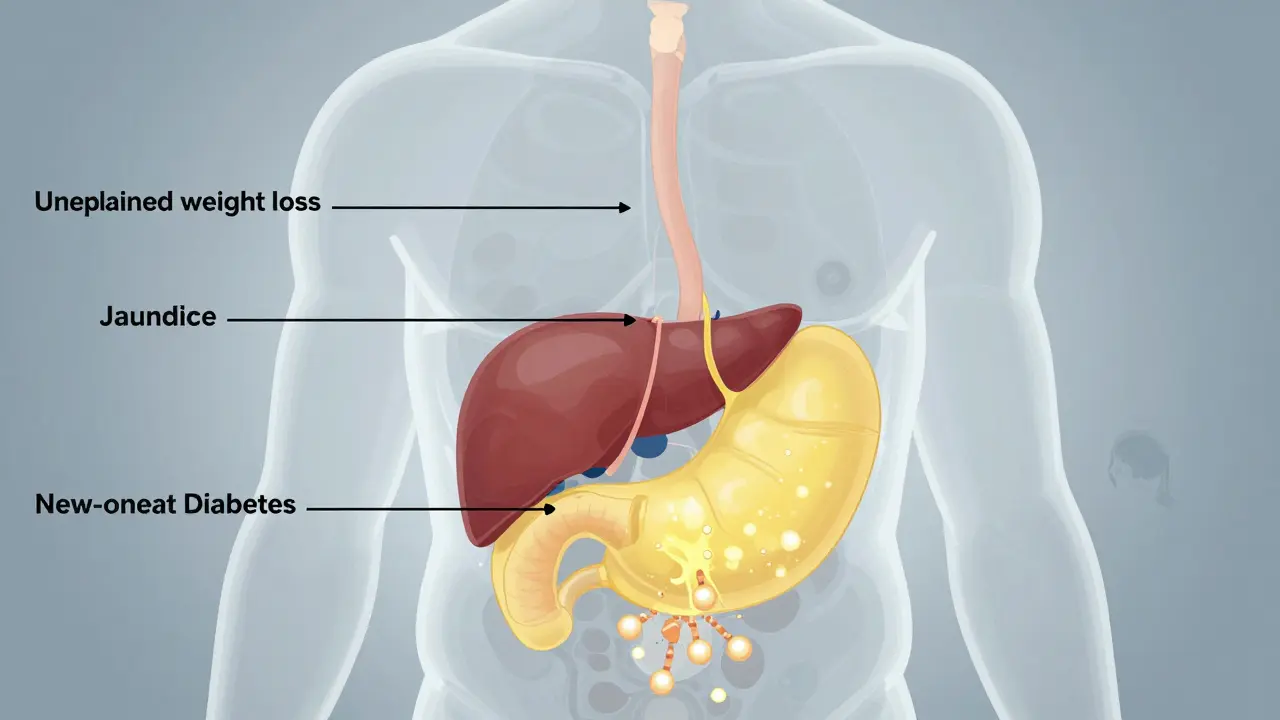
- Unexplained weight loss: Losing 10 pounds or more without trying happens in 60% of cases. It’s not just from not eating-it’s the cancer stealing energy from your body.
- Abdominal or back pain: A dull, constant ache that radiates to your back is common. It often gets worse after eating or lying down.
- Jaundice: Yellow skin or eyes? That’s a big one. It happens when a tumor blocks the bile duct. You’ll also notice dark urine and pale, greasy stools that float. Itching is another sign-60% of people with jaundice from pancreatic cancer feel it badly.
- New-onset diabetes: If you’ve never had diabetes before and suddenly your blood sugar spikes, it could be a clue. Research shows 80% of pancreatic cancer patients develop diabetes within 18 months of diagnosis. Fasting glucose levels above 126 mg/dL are a red flag.
- Loss of appetite and nausea: You might feel full after a bite, or food suddenly turns unappealing. Nausea isn’t always from food poisoning-it can be a tumor pressing on your digestive tract.
What’s even more telling? Depression or anxiety that comes out of nowhere. A 2018 study found that over one-third of pancreatic cancer patients had mood changes as their first symptom-months before any physical signs. If you’ve been feeling down for no reason, and it doesn’t improve with therapy or medication, it’s worth discussing with your doctor.
Why Is It So Hard to Diagnose Early?
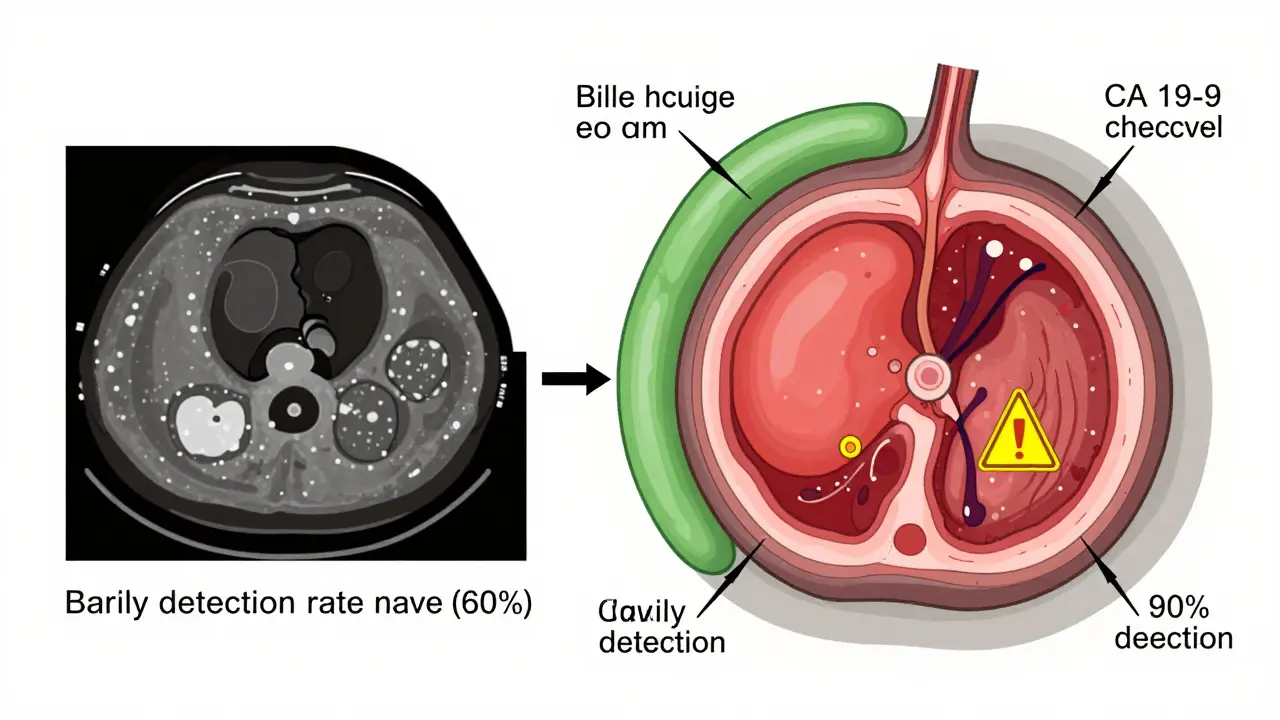
The pancreas is tucked behind other organs. You can’t feel a tumor during a routine exam. There’s no simple blood test like a mammogram or colonoscopy for the general public. Even the most common blood marker, CA 19-9, misses early-stage cancer in half the cases.
Imaging helps-but only when the tumor is big enough. A CT scan catches 90% of tumors larger than 3 cm, but only 60% of those under 2 cm. That’s why most diagnoses happen after the cancer has spread or caused noticeable blockages.
For people at high risk-those with a family history of pancreatic cancer, BRCA gene mutations, or chronic pancreatitis-screening with MRI or endoscopic ultrasound is recommended starting at age 50. But for the average person? There’s no official screening program. That’s why awareness of symptoms is your best defense.
How Is Pancreatic Cancer Treated Today?
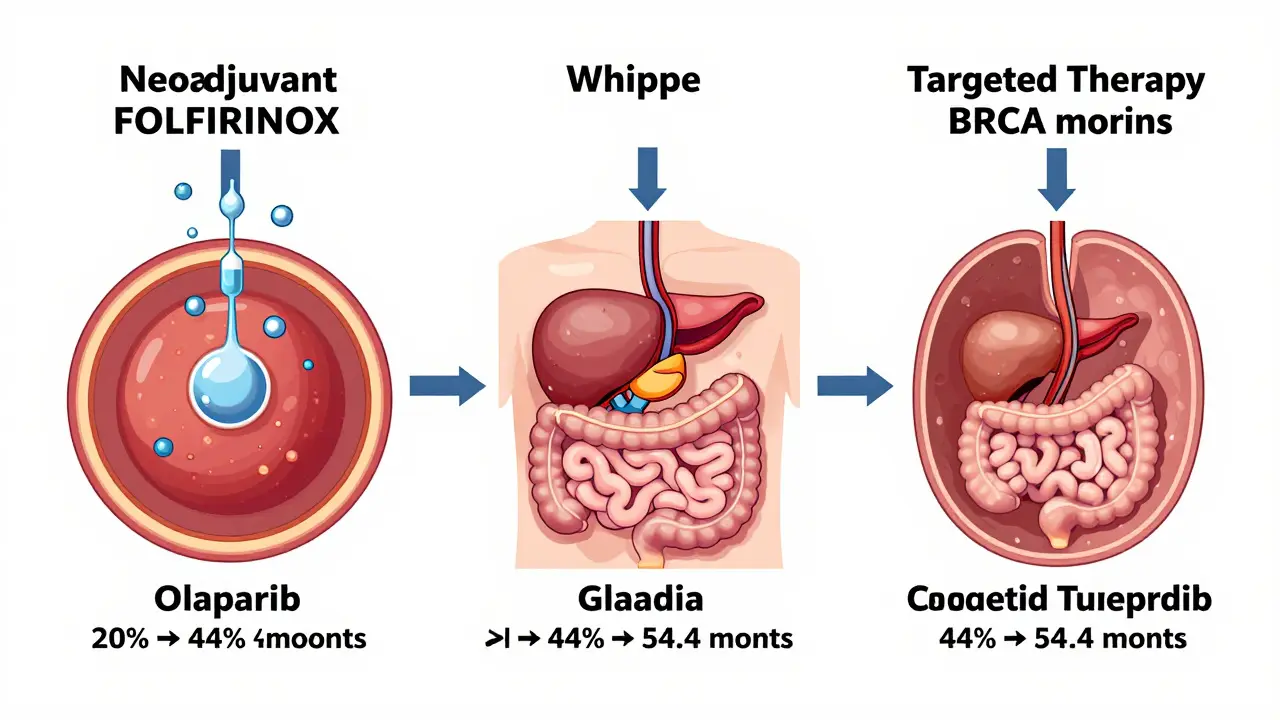
Surgery is still the only chance for a cure. The Whipple procedure removes the head of the pancreas, part of the small intestine, gallbladder, and sometimes part of the stomach. It’s complex, but at top centers, survival rates for early-stage patients hit 20-25% at five years.
But here’s the shift: more patients are getting chemotherapy before surgery now. This is called neoadjuvant therapy. It shrinks tumors that were once considered inoperable. The FOLFIRINOX combo (a mix of four chemo drugs) has shown a 58% response rate in borderline tumors, turning them into candidates for surgery.
For those with advanced cancer, treatment has improved dramatically. In 2022, the PRODIGE 24 trial showed patients on modified FOLFIRINOX lived a median of 54.4 months-nearly four and a half years-compared to just over 20 months with older treatments. That’s not a cure, but it’s a massive leap from the 6-month survival rates seen in 2000.
Targeted Therapies and Personalized Medicine
Not all pancreatic cancers are the same. Some have specific genetic mutations that make them vulnerable to targeted drugs.
- Olaparib: For patients with BRCA1 or BRCA2 mutations, this drug can delay cancer progression by 7.4 months compared to placebo. It’s now a standard maintenance treatment after chemo.
- Pembrolizumab: Works only in the rare 3-4% of cases with MSI-H or dMMR tumors-but when it works, responses can be deep and lasting.
Genetic testing is no longer optional. If you’re diagnosed with pancreatic cancer, ask for tumor profiling. It could open doors to treatments that weren’t available five years ago.
What’s on the Horizon for Early Detection?
Researchers are racing to find ways to catch pancreatic cancer before it spreads. One promising tool is the PancreaSeq test from Johns Hopkins. In high-risk groups, it detects early cancer with 95% accuracy by analyzing DNA in pancreatic fluid.
Blood tests are also improving. The DETECTA trial is testing a method that looks for tumor DNA and protein markers together. Early results show 85% accuracy. Another approach, the ESPAC study, combines four biomarkers (CA19-9, TIMP1, LRG1, and ctDNA) and hit 89% sensitivity in early trials.
Artificial intelligence is helping too. Google Health’s LYNA algorithm can spot cancer cells on tissue slides with 99.3% accuracy-faster and more consistently than human pathologists. And microbiome research is showing that gut bacteria patterns differ in pancreatic cancer patients, offering another potential detection method.
These aren’t just lab experiments. The National Cancer Institute aims to cut pancreatic cancer deaths by 25% by 2030. That goal is starting to feel possible-not because of one miracle cure, but because of dozens of small, smart advances coming together.
What Should You Do If You’re Worried?
If you’re experiencing persistent symptoms-especially unexplained weight loss, new diabetes, or jaundice-don’t wait. Ask your doctor for a CT scan or MRI. Bring up the possibility of pancreatic cancer. Many patients report being told they had gallstones, IBS, or acid reflux for months before the real diagnosis.
If you have a family history of pancreatic, breast, ovarian, or colorectal cancer, talk to a genetic counselor. Testing for BRCA, Lynch syndrome, or other inherited mutations could change your screening plan.
And if you’ve been feeling unusually down, anxious, or just "off" for no clear reason, don’t brush it off. Mental health changes can be the earliest signal.
Pancreatic cancer isn’t a death sentence anymore. It’s still dangerous, yes-but the tide is turning. More people are surviving longer. More treatments are working. More doctors are listening to subtle signs. Your awareness could be the difference between catching it early… and missing it entirely.
Can pancreatic cancer be detected with a blood test?
There’s no single blood test that can reliably detect early pancreatic cancer in the general population. The CA 19-9 test is sometimes used, but it’s only accurate for advanced cases and can be elevated by other conditions like pancreatitis or liver disease. New multi-marker blood tests-like those in the DETECTA and ESPAC trials-are showing promise, with up to 89% accuracy in early research, but they’re still in clinical trials and not yet available for routine use.
Is jaundice always a sign of pancreatic cancer?
No, jaundice can come from many causes, including gallstones, hepatitis, or liver disease. But when jaundice appears without a clear reason-especially with pale stools, dark urine, and itching-it should prompt immediate investigation. In people over 50, new-onset jaundice is one of the strongest indicators of pancreatic cancer, particularly if the tumor is in the head of the pancreas.
Can you survive pancreatic cancer if it’s caught early?
Yes. When pancreatic cancer is found before it spreads (localized stage), the five-year survival rate jumps to 44%. That’s still lower than many other cancers, but it’s a huge improvement over the 3% survival rate for metastatic disease. Surgery combined with chemotherapy can lead to long-term survival in these cases. The key is catching it early-and that’s why recognizing symptoms matters.
Does new-onset diabetes mean I have pancreatic cancer?
Not necessarily, but it’s a warning sign worth investigating. About 80% of pancreatic cancer patients develop diabetes within 18 months of diagnosis. If you’re over 50, have no family history of diabetes, and suddenly develop high blood sugar without weight gain or lifestyle changes, your doctor should consider pancreatic cancer as a possible cause. A CT scan or MRI may be recommended.
Are there screening tests for pancreatic cancer?
No routine screening exists for the general public because the disease is rare and hard to detect early. But if you have a strong family history, inherited gene mutations (like BRCA), or chronic pancreatitis, you may be eligible for annual screening with MRI or endoscopic ultrasound. These are offered at specialized centers like Johns Hopkins and MD Anderson. Talk to a genetic counselor if you’re unsure about your risk.
What’s the survival rate for pancreatic cancer today?
The overall five-year survival rate is 12%, according to the National Cancer Institute. But that number hides big differences: 44% for localized cancer, 15% for regional spread, and just 3% for cancer that has metastasized. Thanks to newer treatments like FOLFIRINOX and targeted therapies, median survival for advanced cases has improved from 6 months in 2000 to 12-15 months today-and some patients live much longer.

steve rumsford
January 8, 2026 AT 06:29Been dealing with back pain and weird indigestion for months. Thought it was just stress from work. Now I’m scared to even eat breakfast. If this post saved one person from getting dismissed by their doctor, it’s already worth it.
Anthony Capunong
January 9, 2026 AT 17:07Of course they didn’t mention the real cause-Big Pharma doesn’t want you to know you can cure this with turmeric and lemon water. They’re selling chemo like it’s a subscription box. Wake up people.
Vince Nairn
January 10, 2026 AT 15:21So let me get this straight-you’re telling me that if I’m depressed, losing weight, and suddenly diabetic, I should just assume it’s cancer and not just… life? I mean, I get it, awareness is good, but this reads like a fearmongering pamphlet from a clinic trying to sell MRIs.
Kyle King
January 11, 2026 AT 20:52They’re lying. The government knows about the cure but hides it because cancer patients are the only ones who still buy insurance. Also, 5G causes pancreas tumors. I’ve seen the videos. You think they’re testing blood markers? Nah. They’re tracking your phone’s GPS to see who’s near a cell tower when they start feeling sick.
Kamlesh Chauhan
January 12, 2026 AT 21:05Why even bother reading this? Everyone knows if you get pancreatic cancer you’re dead. No point in screening or chemo. Just drink whiskey and watch Netflix. I did that last year. Still alive. LOL
Emma Addison Thomas
January 14, 2026 AT 19:48Interesting how the UK’s NHS still doesn’t offer screening even for high-risk groups. I had a friend in Manchester who waited 11 months for a scan after jaundice. By then, it was stage IV. Awareness is good, but access is everything.
Mina Murray
January 16, 2026 AT 06:40So you’re saying new-onset diabetes = cancer? What about all the people who gained 40 pounds and started eating donuts? Or the 72-year-old who finally stopped walking 3 miles a day? You’re pathologizing normal life. And CA19-9 is useless-my uncle had pancreatitis and his levels were through the roof. This article is dangerously oversimplified.
Christine Joy Chicano
January 17, 2026 AT 04:08I’ve been following the ESPAC trial data since last year. The real breakthrough isn’t just the biomarkers-it’s the machine learning models that predict tumor behavior from imaging patterns. Google’s LYNA isn’t just spotting cells-it’s predicting which tumors will respond to FOLFIRINOX before treatment even starts. We’re entering an era where pancreatic cancer might be managed like HIV: chronic, not terminal. That’s not hype. That’s peer-reviewed.
And yes, if you’re over 50, unexplained weight loss + new diabetes = get scanned. Not because it’s cancer, but because it’s worth ruling out. I’m not scared-I’m just… prepared.
Adam Gainski
January 17, 2026 AT 19:04Christine’s right. The real story here is the shift from reactive to proactive care. Neoadjuvant chemo used to be a last resort. Now it’s standard for borderline resectable tumors. And olaparib? For BRCA carriers, it’s changed the game. I’m a nurse in oncology-last month, a 48-year-old woman with a BRCA2 mutation went from stage III to no evidence of disease after 6 months of FOLFIRINOX + olaparib. We used to never see that. Now it’s happening twice a month.
Don’t panic. But do pay attention. And if your doctor brushes off symptoms because you’re "too young"-go to another one. This isn’t about fear. It’s about knowing your body.
Paul Mason
January 18, 2026 AT 01:35Man I had that same back pain last year. Went to the doc, they said it was my posture. Turns out I was just sitting wrong. But now I’m paranoid. Should I get a CT scan just in case? I mean, what’s the worst that could happen? I spend $1200 and find out I’m fine? Or I save $1200 and die in six months?
Mina Murray
January 19, 2026 AT 23:03Adam, you’re being way too optimistic. You think FOLFIRINOX is a miracle? My cousin got it. Lost 30 pounds, vomited every day, still died in 9 months. And now they’re pushing genetic testing like it’s a spa day. Who pays for that? Not Medicare. Not Medicaid. Not most insurance. This is all just a luxury for rich people with good doctors.