Most people don’t realize their liver is silently filling with fat-until it’s too late. Nonalcoholic fatty liver disease (NAFLD), now more accurately called Metabolic Associated Fatty Liver Disease (MAFLD), affects about 1 in 4 adults worldwide. In the U.S. and Europe, that number climbs to nearly 1 in 3. And here’s the kicker: most of these people feel fine. No pain. No jaundice. No warning signs. But inside their livers, fat is building up, inflammation is starting, and fibrosis could be creeping in. The good news? If caught early, this condition can be reversed. Not just slowed-reversed.
What Exactly Is MAFLD?
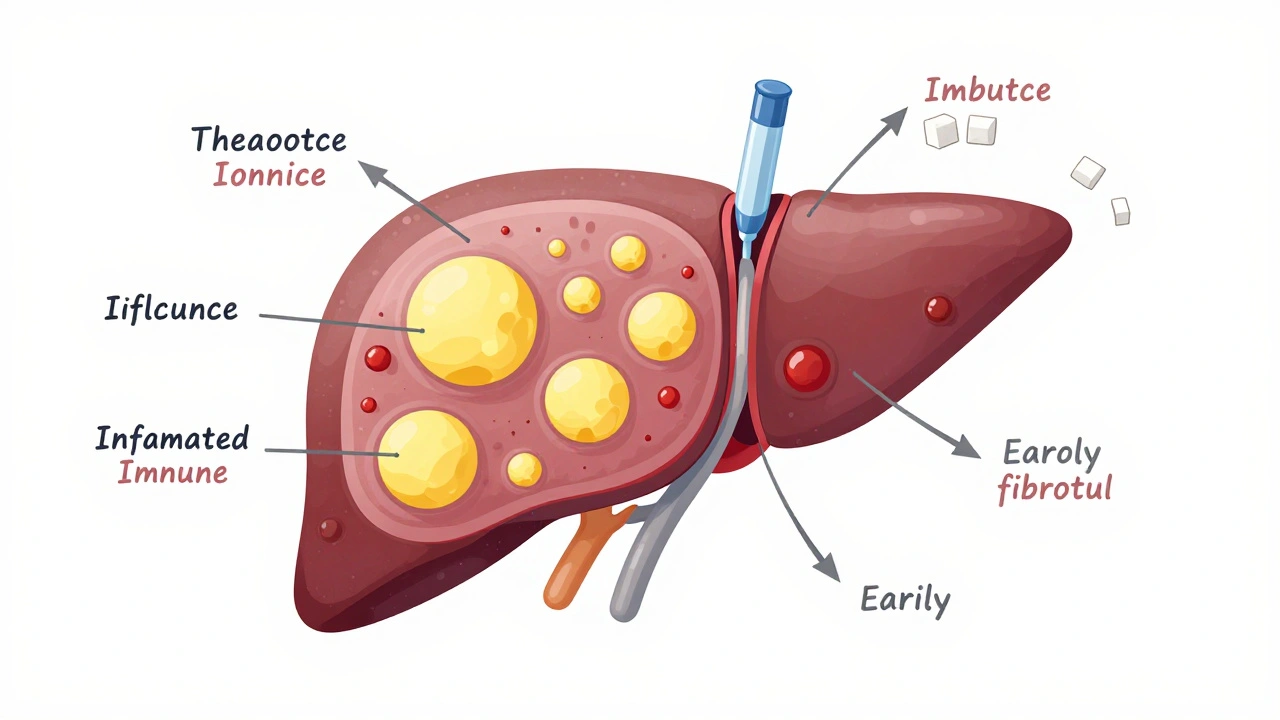
MAFLD isn’t just ‘a little fat on the liver.’ It’s when more than 5% of liver cells are filled with fat-not because of heavy drinking, but because of metabolic problems. Think insulin resistance, belly fat, high blood sugar, and high triglycerides. It’s not a separate disease. It’s your body’s response to how you’ve been eating, moving, and managing stress over years.
The old name, NAFLD, focused on what wasn’t there: alcohol, viruses, or other liver diseases. The new name, MAFLD, flips the script. It says: this is a disease tied to metabolism. You don’t need to be overweight to have it. Even people with normal weight can develop MAFLD if their insulin is out of whack. And once fat builds up, it doesn’t just sit there. It starts talking to immune cells, triggering inflammation, damaging liver cells, and eventually scarring the organ.
How Does It Progress?
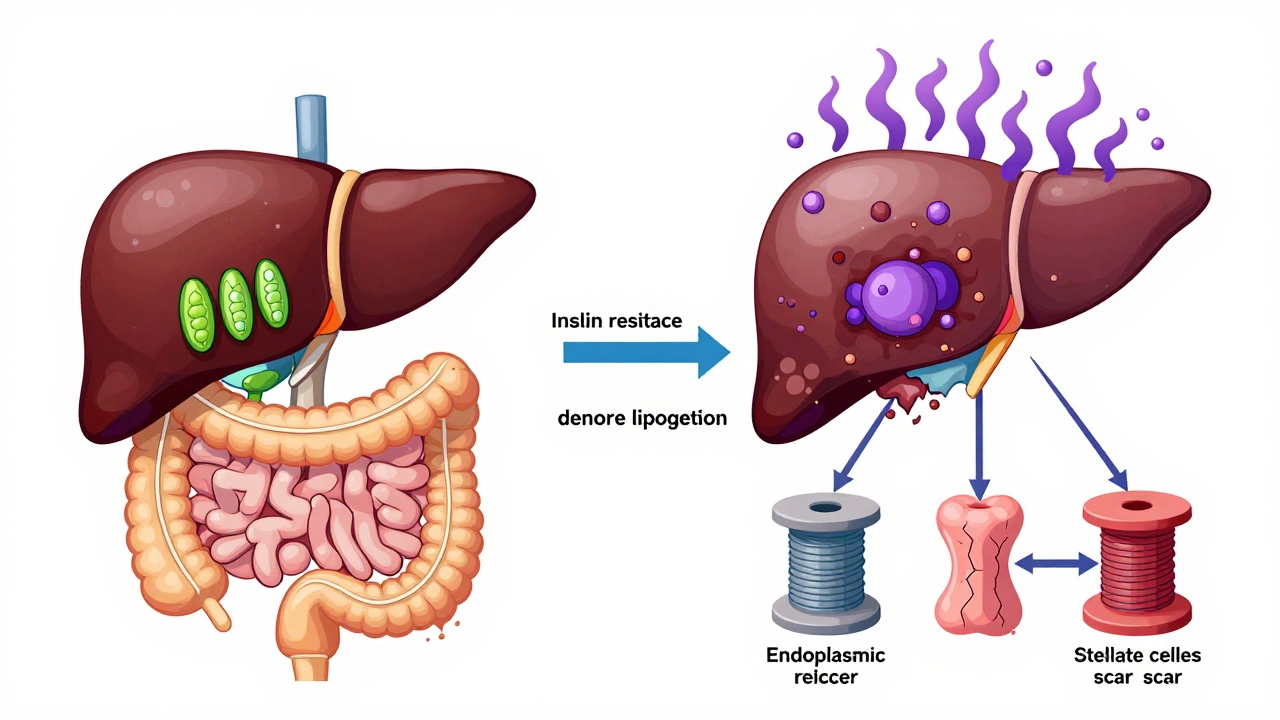
Not everyone with fat in their liver gets sick. But for some, it turns into NASH-nonalcoholic steatohepatitis. That’s when fat causes real damage: liver cells die, immune cells swarm in, and scar tissue begins to form. Think of it like a slow burn. First, fat accumulates. Then, toxic fats like ceramides and diacylglycerols overload mitochondria. The liver can’t process them. Oxidative stress spikes. The endoplasmic reticulum gets stressed. Inflammation kicks in.
At this stage, fibrosis starts. Liver stellate cells-normally quiet-turn into scar factories. If unchecked, this leads to cirrhosis. And cirrhosis? That’s when the liver can’t regenerate properly. It becomes hard, lumpy, and dysfunctional. About 20% of people with NASH develop cirrhosis within 15 years. And once cirrhosis hits, the risk of liver cancer rises sharply.
But here’s what most doctors don’t tell you: progression isn’t inevitable. Studies show only 20-30% of people with MAFLD ever reach advanced fibrosis. That means 7 out of 10 people stay at the fatty liver stage-forever-if they make the right changes.
What’s Driving This?
The real engine behind MAFLD? Insulin resistance. When your cells stop responding to insulin, your body starts pumping out more of it. That extra insulin tells your liver: ‘Make more fat.’ And it does-through a process called de novo lipogenesis. In healthy people, this accounts for about 5% of liver fat. In MAFLD? It jumps to 26%. That’s not from eating too much fat. That’s from eating too many carbs-especially sugar and refined grains.
Another big player? Gut health. When your gut lining gets leaky (thanks to processed foods, antibiotics, or chronic stress), endotoxins like LPS slip into your bloodstream and head straight to your liver. That triggers inflammation. Studies show people with MAFLD have different gut bacteria than healthy people. Some bad bugs are overgrown. Good ones are missing. Fecal transplants from healthy donors have even improved liver fat in early trials.
And don’t forget the role of fat transport proteins. FATP5, a protein that pulls fatty acids into liver cells, is turned up in MAFLD. Delete it in mice? Liver fat drops by 40%. That’s not a coincidence. It’s biology.
Can You Reverse It?
Yes. And not just a little. Real, measurable, biopsy-proven reversal is possible.
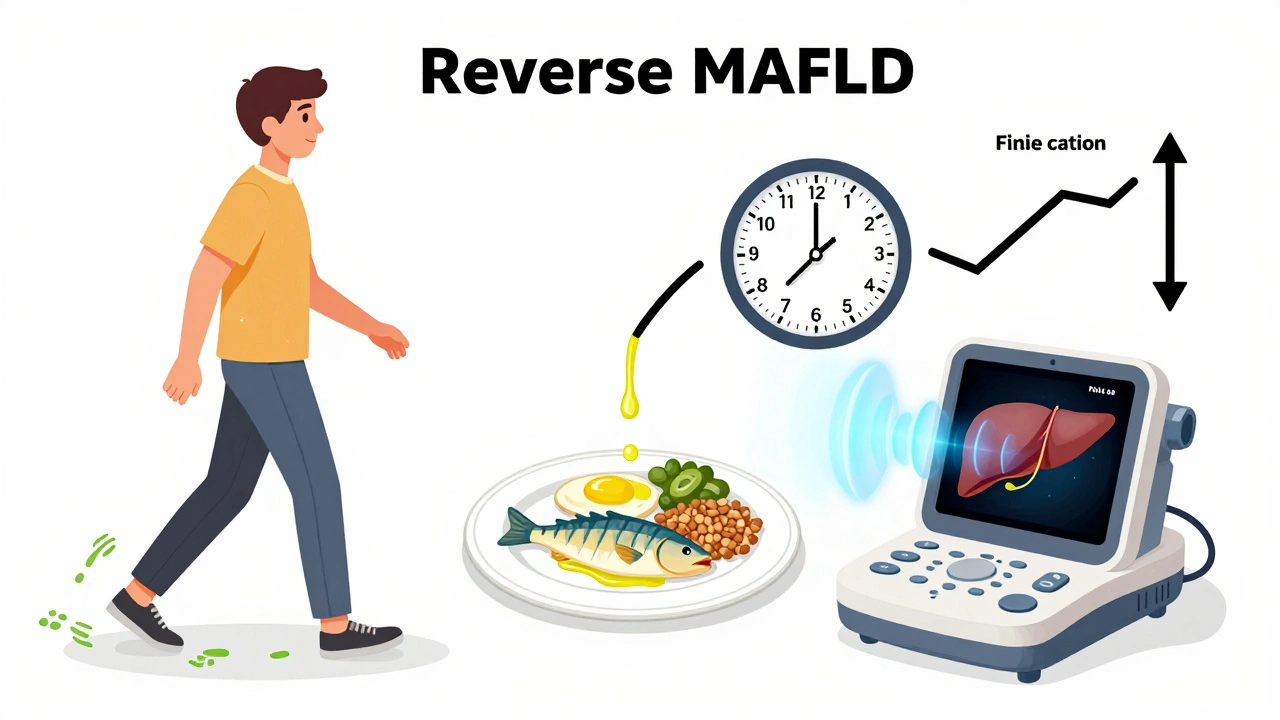
The most powerful tool? Weight loss. Losing 7-10% of your body weight can clear NASH in 90% of cases. Even losing 3-5% reduces liver fat. Losing 7-10% can actually reduce fibrosis. That’s not theoretical. It’s from the LEAN study, published in 2013, and confirmed by dozens since.
But how you lose it matters more than how much.
The Diet That Works
Forget low-fat. Forget calorie counting. The Mediterranean diet is the gold standard. It’s not a fad. It’s a way of eating that’s been tested in trials and shown to cut liver fat by 60-70% in six months.
Here’s what it looks like:
- 40-45% carbs from whole foods: vegetables, legumes, fruits, whole grains
- 35-40% healthy fats: olive oil, nuts, avocado, fatty fish
- 15-20% protein: fish, eggs, poultry, tofu
- 25-30 grams of fiber daily
- No sugar-sweetened drinks. No ultra-processed snacks. No white bread.
One patient on a health forum wrote: ‘I cut out soda and switched to olive oil. Lost 10% of my weight in 6 months. My ALT dropped from 98 to 34.’ That’s not luck. That’s diet.
And don’t underestimate the power of time-restricted eating. Eating within an 8-10 hour window helps reset insulin sensitivity. You don’t need to count calories. Just stop eating after dinner and don’t snack before breakfast.
Exercise: More Than Just Burning Calories
Exercise isn’t optional. It’s medicine. But not all exercise is equal.
Aerobic activity-walking, cycling, swimming-for 150 minutes a week reduces liver fat by 20-30%. Add resistance training-two days a week with weights or bodyweight exercises-and you get an extra 30% fat loss. Why? Muscle burns glucose. More muscle means less glucose floating around to turn into liver fat.
One study showed people who did both aerobic and strength training cut liver fat nearly twice as much as those who only walked. And you don’t need a gym. Bodyweight squats, push-ups, and resistance bands work just fine.
What About Supplements and Medications?
There’s no magic pill. But some things help.
Pioglitazone (a diabetes drug) improves liver histology in nearly half of patients. But it causes weight gain-2 to 4 kilograms. Not ideal if you’re trying to lose fat.
GLP-1 receptor agonists like liraglutide and semaglutide are game-changers. They reduce liver fat, inflammation, and fibrosis. They also help you lose weight. But they’re expensive. And insurance often denies coverage unless you have diabetes.
Vitamin E (800 IU daily) is FDA-approved for non-diabetic NASH. It reduces oxidative stress. But long-term safety is unclear. Don’t take it without medical supervision.
Probiotics like Lactobacillus rhamnosus GG have shown promise in reducing liver inflammation by tightening the gut barrier. Not a cure, but a helpful support.
New drugs are coming fast. Resmetirom, approved by the FDA in March 2024, targets thyroid receptors in the liver and reduced fibrosis in trials. Lanifibranor (a PPAR agonist) is expected to get approval by 2025. These aren’t cures-but they’re tools for people who’ve tried everything else.
Why Most People Fail
People don’t fail because they lack willpower. They fail because the system isn’t built for them.
62% of patients say their doctors don’t understand MAFLD. Many still think it’s ‘just fatty liver’ and don’t monitor it. FibroScan, a non-invasive test that measures liver stiffness and fat, is available in only 35% of primary care clinics. Insurance won’t cover it. So many people never get diagnosed until it’s too late.
And then there’s the frustration. ‘I’ve been eating clean for a year. Why isn’t my liver healing?’ Because healing takes time. Liver enzymes normalize in 3-6 months. Fibrosis improvement? That takes 6-12 months. You need consistency, not perfection.
One Reddit user wrote: ‘I did 30 minutes of walking every day for a year. Lost 10%. My FibroScan went from F3 to F1. It wasn’t easy. But it was worth it.’
What You Can Do Today
You don’t need a prescription. You don’t need to join a program. Start here:
- Remove sugary drinks. Seriously. One soda a day is enough to drive up liver fat.
- Swap white bread, pasta, and rice for whole grains, beans, or vegetables.
- Walk 30 minutes a day. Five days a week. That’s it.
- Stop eating 3 hours before bed.
- Get your liver enzymes checked. If they’re high, ask for a FibroScan.
If you have diabetes, prediabetes, or belly fat, get tested. Even if you feel fine. MAFLD doesn’t scream. It whispers. And if you ignore it, it gets louder.
The Future Is Personal
AI is starting to help. Algorithms can now predict fibrosis progression with 89% accuracy using simple blood tests and BMI. That means in a few years, your doctor might use a digital tool to tell you your risk-not guess.
But the biggest driver of change? You. The obesity epidemic is growing. By 2035, WHO predicts 3.3 billion adults will be overweight. That means more MAFLD. But also more awareness. More research. More tools.
The message is simple: your liver doesn’t need drugs. It needs balance. Less sugar. More movement. Better sleep. Less stress. And time.
It’s not about being perfect. It’s about being consistent. And it’s never too late to start.

Sangram Lavte
December 7, 2025 AT 04:02My dad had elevated ALT for years and no one ever connected it to diet. He switched to brown rice, stopped soda, and started walking. Two years later, his liver enzymes were normal. No meds. Just simple changes.
Oliver Damon
December 7, 2025 AT 14:52The metabolic framing of MAFLD is crucial. It shifts the narrative from moral failure to biochemical dysfunction. Insulin resistance isn't a choice-it's a downstream effect of chronic hyperinsulinemia driven by ultra-processed carbohydrates. The liver isn't broken; it's doing exactly what evolution programmed it to do: store excess energy. The problem is the environment, not the organism.
What's fascinating is how de novo lipogenesis becomes the dominant pathway for hepatic lipid accumulation, even in lean individuals. That's not about fat intake-it's about carb overload. Glucose → acetyl-CoA → palmitate. It's biochemistry, not willpower.
The gut-liver axis is equally underappreciated. LPS translocation from dysbiotic microbiota activates TLR4 on Kupffer cells, triggering TNF-alpha and IL-6 cascades. That's not speculation-it's replicated in murine models and human biopsy studies. Probiotics aren't placebo; they're modulators of endotoxin flux.
And yes, time-restricted eating works because it lowers the insulin area-under-the-curve. You're not fasting-you're giving your liver a nightly reprieve from lipogenic signaling. That's physiology, not dogma.
Kurt Russell
December 8, 2025 AT 16:25STOP SCROLLING. START WALKING. RIGHT NOW. I don't care if you're 20 or 60. Your liver doesn't care about your excuses. One soda a day? That's 40 grams of fructose. Your liver turns that into fat. Period. No debate.
I helped my sister reverse her NASH. She didn't join a gym. She didn't buy supplements. She cut out juice, started walking after dinner, and stopped eating after 7pm. In 8 months, her FibroScan dropped from F3 to F1. She cried when she saw the results. Not because she lost weight-because she got her life back.
You don't need a PhD to fix this. You need to stop lying to yourself. Sugar isn't 'just calories.' It's poison for your liver. And if you're still drinking it, you're choosing ignorance over survival.
Do it for your future self. Not tomorrow. Not next week. TODAY.
Stacy here
December 9, 2025 AT 05:18They don't want you to know this, but Big Pharma and the USDA are covering this up. MAFLD is a gateway to control-once they label you 'metabolically compromised,' they can push you into expensive drugs, mandatory diets, and surveillance programs.
Why is resmetirom approved so fast? Because it's a cash cow. They don't care if you heal-they care if you keep buying. The Mediterranean diet? Free. No patent. No profit. So they ignore it.
And don't get me started on FibroScan. It's available in only 35% of clinics? That's not negligence-that's intentional. If everyone knew their liver was dying, they'd stop eating the processed crap they're selling you. The system needs sick people to survive.
They'll tell you 'it's just fatty liver.' But it's not. It's a symptom of a broken food system. A system that profits from your ignorance. Wake up. Your liver is screaming. Are you listening-or just scrolling?
Louis Llaine
December 10, 2025 AT 02:20So... eat less sugar, walk more, and don't eat before bed. And somehow this is a medical breakthrough? I'm shocked. Truly. Next they'll tell us breathing fresh air helps your lungs.
Also, why is the guy who wrote this suddenly an expert? Did he get a liver biopsy after eating kale for six months? Just saying.
Jane Quitain
December 10, 2025 AT 05:39i just started doing the 8 hour window and omg its so hard but i think its working? my tummy feels less bloated and i dont crave sugar as much? im not even trying to lose weight but my dr said my alt was high so i thought maybe…? also i switched to olive oil instead of butter and it feels like a tiny win lol
Kyle Oksten
December 11, 2025 AT 17:59The most dangerous myth in medicine is that 'weight loss reverses MAFLD.' That's not the whole story. I've seen lean patients with NASH who lost zero weight but reversed fibrosis by eliminating fructose and increasing omega-3 intake. The driver isn't adiposity-it's metabolic dysregulation.
And the obsession with BMI? It's outdated. A person can have normal weight and high visceral fat-what we call 'TOFI'-thin outside, fat inside. That's the real silent killer.
Exercise isn't just about burning calories. It's about increasing GLUT4 translocation, improving insulin sensitivity, and reducing hepatic lipid flux. It's cellular biology, not calorie math.
And yes, vitamin E has risks-but so does ignoring the disease. The choice isn't between perfect and nothing. It's between action and inaction.
Sam Mathew Cheriyan
December 12, 2025 AT 04:45lol i read this and thought 'this is just a new way to scare people into eating salads' but then i checked my blood work and my triglycerides are through the roof. maybe there's something here. i used to drink 3 energy drinks a day. now i drink coconut water. not a hero, but not a zombie anymore.
Ernie Blevins
December 12, 2025 AT 23:13Who cares? Everyone's gonna die anyway. You think your liver's gonna save you? Nah. You're just delaying the inevitable. Eat the pizza. Drink the soda. Live a little.
Nicholas Heer
December 14, 2025 AT 16:41MAFLD? More like MADE UP FATTY LIVER DISEASE. This is all a scam to sell you organic kale and expensive supplements. In my grandpa's day, people ate lard and fried food and lived to 85. Now we're told to eat 'Mediterranean' like we're in some European spa. BS.
And why is this article pushing 'FibroScan'? That's a government surveillance tool disguised as medicine. They're tracking your liver to control your food choices. Wake up, sheeple.