Obesity isn’t a lack of willpower. It’s a chronic disease - and treating it like one makes all the difference. Since 2013, the American Medical Association has officially classified obesity as a medical condition, not a personal failure. Today, medical weight management has evolved into a structured, science-backed system that combines clinics, medications, and ongoing monitoring to help people lose weight and keep it off. This isn’t about fad diets or quick fixes. It’s about real, lasting change - and it’s working.
What Medical Weight Management Actually Looks Like
Medical weight management isn’t just seeing a doctor and getting a prescription. It’s a full-care approach that brings together nutritionists, behavioral coaches, physicians, and sometimes pharmacists. The goal? To achieve at least a 5% reduction in body weight - a number that may sound small, but it’s enough to lower blood pressure, improve insulin sensitivity, and reduce the risk of heart disease. For many, losing 10% or more can lead to remission of type 2 diabetes. Clinics that specialize in this care follow strict guidelines. The American College of Cardiology’s 2025 Clinical Guidance says patients need a BMI of 30 or higher to qualify. If you have a BMI of 27 or above and conditions like high blood pressure, prediabetes, or sleep apnea, you’re still eligible. That’s because weight isn’t just about numbers on a scale - it’s about how those extra pounds affect your health.How Medications Are Changing the Game
For years, weight loss medications were limited, underused, or even stigmatized. That’s changed. Today, two drugs - semaglutide (Wegovy®) and tirzepatide (Zepbound®) - are leading the charge. Both are GLP-1 receptor agonists, originally developed for type 2 diabetes, but now proven to be powerful weight loss tools. In clinical trials, semaglutide helped people lose an average of 14.9% of their body weight over 72 weeks. Tirzepatide? It pushed that number to 20.2%. These aren’t outliers. Real-world data from clinics show similar results. The difference between the two? Tirzepatide works slightly better, but it’s also more expensive and harder to get through insurance. There’s a new player too: retatrutide, a triple-agonist drug targeting GLP-1, GIP, and glucagon receptors. Early phase 2 trials showed an average weight loss of 24.2% in just 48 weeks. It’s not FDA-approved yet, but it’s coming fast. The big catch? Insurance coverage. Only 68% of commercial insurers cover these medications in 2025. Compare that to 98% coverage for diabetes drugs like metformin. Medicare? Only 12% of Medicare Advantage plans cover them. That means many people pay out of pocket - $150 to $300 a month - while commercial programs like Weight Watchers cost $20 to $60. The gap is wide, and it’s unfair.Why Clinics Outperform Commercial Programs
You’ve probably seen ads for apps, shakes, or online coaching. They work for some. But when you compare medical weight management clinics to commercial programs, the data doesn’t lie. A 2024 JAMA Internal Medicine study found that people in medical programs lost 9.2% of their body weight in a year. Those in commercial programs? Only 5.1%. Why? Because medical clinics don’t just tell you what to eat. They customize your plan. They track your progress. They adjust your meds. They help you deal with emotional eating, sleep issues, stress, and even medications that cause weight gain. Take West Virginia University’s program. Before you even meet a doctor, you complete a mandatory online orientation, fill out detailed questionnaires, and read a patient handbook. You’re not just another number. You’re part of a system designed to understand your life - your schedule, your food preferences, your barriers. These clinics also use electronic health record templates to document weight, waist circumference, blood pressure, and lab values. That way, every visit builds on the last. No one’s starting from scratch.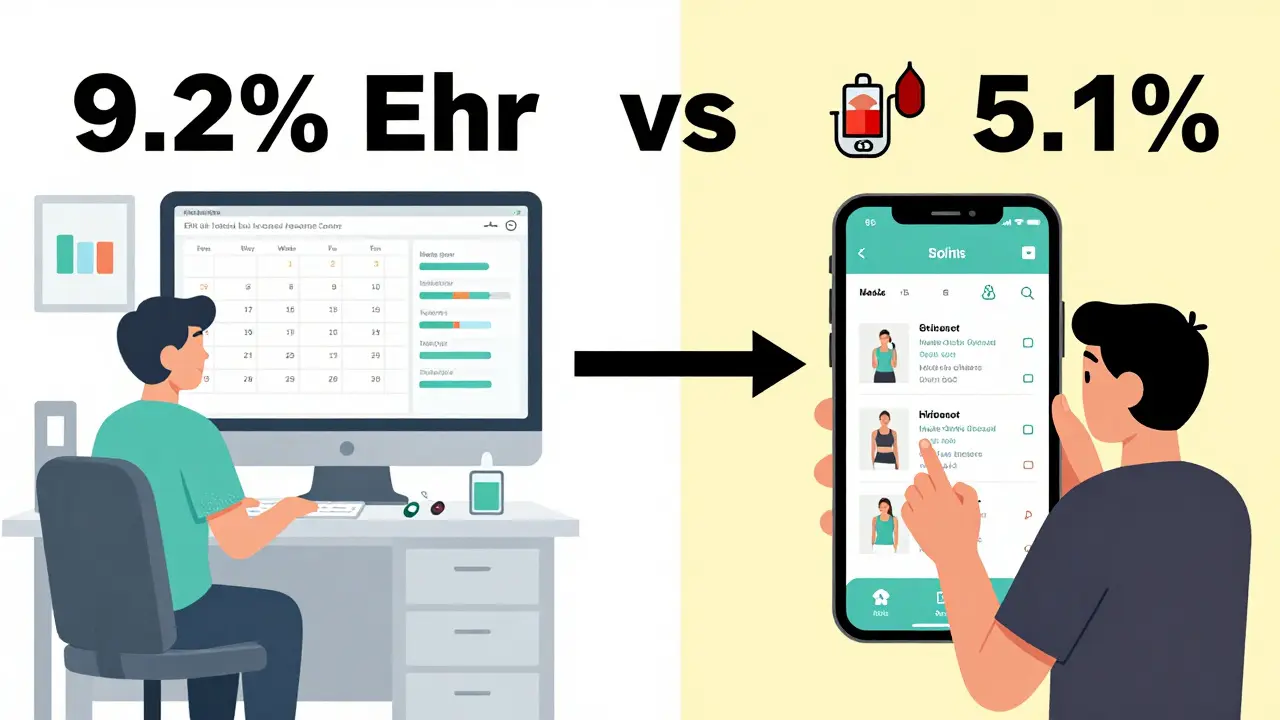
Monitoring: The Secret to Long-Term Success
You can’t manage what you don’t measure. That’s why the American Diabetes Association recommends checking weight, waist size, and blood pressure every three months during active treatment. That’s more frequent than most people realize. Successful programs track more than just the scale. They look at:- Waist circumference - a better predictor of heart risk than BMI alone
- HbA1c levels - to see if diabetes is improving
- Lipid panels - for cholesterol and triglycerides
- Medication side effects - nausea, fatigue, or low blood sugar
- Mental health - depression and anxiety often go hand-in-hand with weight struggles
Who’s Getting Left Behind
The system is improving, but it’s not equal. Black and Hispanic patients are 43% less likely to be offered medication, even when they meet the same BMI and health criteria. Rural patients often travel hours to reach a clinic. People on Medicaid or Medicare often can’t get coverage at all. The American College of Cardiology’s 2025 guidance calls this out directly. It urges clinics to use inclusive language, provide blood pressure cuffs in multiple sizes, and replace blame with support. Chairs without armrests. Food logs that don’t shame. Providers trained in weight bias. And yet, the biggest barrier isn’t geography or race - it’s cost. One patient on Reddit said she waited 8 weeks just to get her prescription filled because her insurer denied it twice. That’s not care. That’s bureaucracy.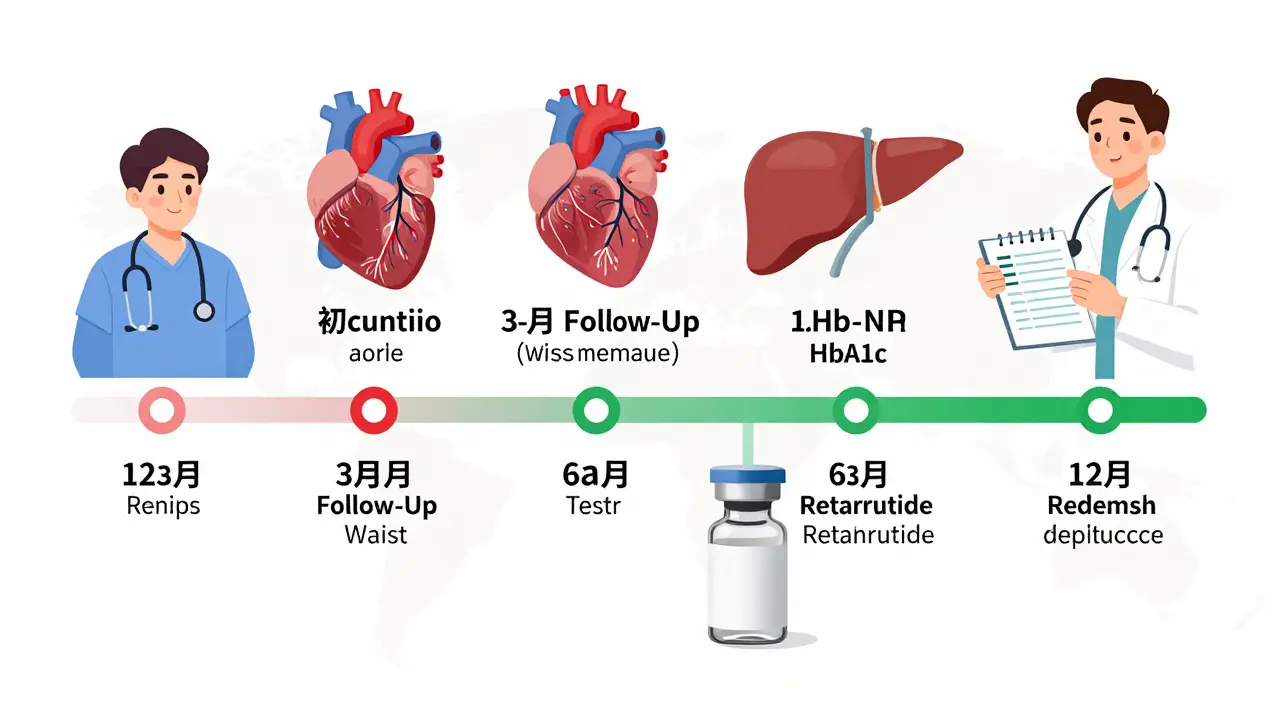
What You Can Do
If you’re struggling with weight and health:- Ask your primary care doctor if they offer medical weight management - or can refer you.
- Check if your employer offers it. Nearly half of Fortune 500 companies now include it in wellness plans.
- Look for clinics that use the nutrition care process - that means a registered dietitian is involved.
- Don’t wait until your BMI hits 35. If you have prediabetes or high blood pressure, start now.
- Track your progress: weight, waist, energy, sleep. Use a notebook or app. Data gives you power.
The Future Is Here
By 2030, the American Diabetes Association predicts weight management will be as routine in diabetes care as checking HbA1c. That’s huge. It means doctors won’t just treat your blood sugar - they’ll treat the root cause. The market is growing fast. The U.S. obesity treatment industry hit $2.8 billion in 2025 and is on track to hit $5.1 billion by 2030. More medical schools are teaching obesity medicine. More providers are getting certified. More patients are seeing results. This isn’t about looking a certain way. It’s about living longer, feeling better, and reducing your risk of heart attack, stroke, and diabetes. And for the first time, medicine is finally catching up.Can I get medical weight management through my regular doctor?
Some primary care doctors offer basic weight management, but many don’t have the time, training, or resources. Specialized clinics have dietitians, behavioral coaches, and access to the latest medications. Ask your doctor for a referral. If they say no, ask why - and consider seeking out an obesity medicine specialist.
Are GLP-1 medications safe?
Yes, when used as prescribed. Semaglutide and tirzepatide have been studied in tens of thousands of people. Common side effects include nausea, vomiting, or diarrhea - especially at first. These usually fade in a few weeks. Serious risks like pancreatitis or gallbladder disease are rare. They’re far safer than bariatric surgery, which has a 4.7% complication rate. Medical weight management has a complication rate under 0.2%.
How long do I need to stay on these medications?
Obesity is a chronic disease, so treatment often is too. Stopping the medication usually leads to weight regain. Most experts recommend continuing as long as it’s helping and well-tolerated. Think of it like taking blood pressure or cholesterol meds - you don’t stop when you feel better. You keep going to stay healthy.
What if my insurance won’t cover the medication?
Many clinics offer patient assistance programs or payment plans. Some pharmaceutical companies have co-pay cards or free trials. Ask your provider - they often know how to navigate this. You can also appeal your insurance denial. The Obesity Medicine Association has templates to help. Don’t give up - coverage is improving, and many people get approved on the second try.
Do I need to follow a strict diet?
No. The best programs don’t force you into rigid rules. Instead, they help you find sustainable habits - like eating more protein, reducing ultra-processed foods, or finding enjoyable movement. One-size-fits-all diets fail 80% of the time. Personalized, flexible nutrition is what works. A registered dietitian will tailor your plan to your culture, schedule, and preferences.
Can I use these medications if I don’t have diabetes?
Absolutely. While these drugs were first approved for diabetes, they’re now approved for obesity alone. If your BMI is 30 or higher (or 27 with a related condition), you qualify. You don’t need to have diabetes to benefit. In fact, many people without diabetes see the biggest improvements in blood pressure and cholesterol.


Sonja Stoces
February 12, 2026 AT 23:34Luke Trouten
February 14, 2026 AT 12:16Kristin Jarecki
February 16, 2026 AT 05:54Jonathan Noe
February 16, 2026 AT 12:16Jim Johnson
February 18, 2026 AT 11:40Autumn Frankart
February 20, 2026 AT 09:55Skilken Awe
February 21, 2026 AT 08:33Steve DESTIVELLE
February 22, 2026 AT 17:15steve sunio
February 23, 2026 AT 09:29Jack Havard
February 24, 2026 AT 00:30Annie Joyce
February 25, 2026 AT 00:57Rob Turner
February 25, 2026 AT 06:18Gabriella Adams
February 25, 2026 AT 22:12Sophia Nelson
February 27, 2026 AT 12:38