Kava Medication Interaction Checker
Check if Your Medication Interacts with Kava
Enter a medication name to see if it's dangerous to combine with kava. This tool analyzes known interactions based on liver enzyme interference.
Enter a medication name to get results...
When you're looking for natural relief from anxiety, kava might seem like a safe bet. It’s been used for centuries in the South Pacific, and today, it’s sold in health stores and online as a calming supplement. But here’s the part no one tells you: kava can seriously hurt your liver-especially if you’re taking any other medications.
What Exactly Is Kava?
Kava comes from the root of Piper methysticum, a plant native to islands like Fiji, Vanuatu, and Samoa. For thousands of years, people there have prepared it as a ceremonial drink using cold water extraction. The active compounds, called kavalactones, are what give kava its calming effect-similar to benzodiazepines like Xanax, but without the same risk of addiction.
But here’s the catch: what works in a village in Vanuatu doesn’t always translate to a capsule bought in Adelaide or Chicago. Most commercial kava products today aren’t made the traditional way. Instead, they use solvents like ethanol or acetone to pull out the kavalactones. These organic extracts are the ones linked to liver damage.
Why Kava Can Damage Your Liver
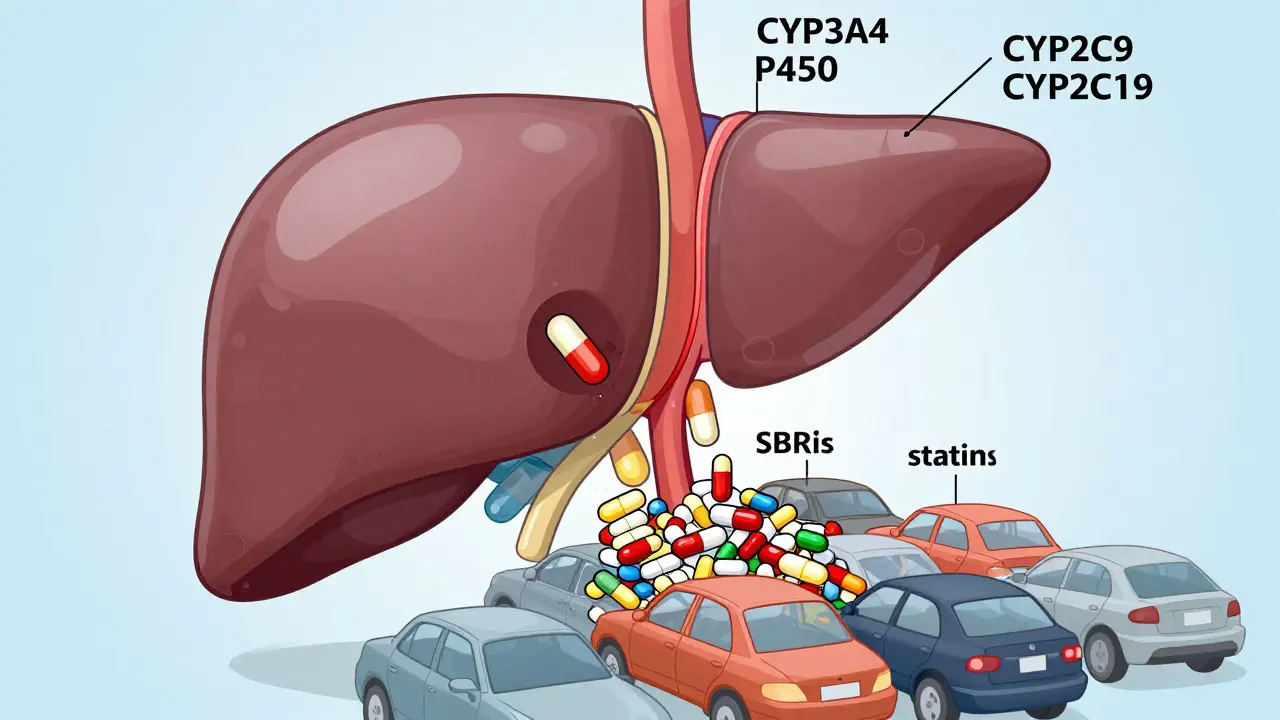
Your liver is your body’s main detox center. It uses enzymes-mostly from the cytochrome P450 family-to break down drugs, alcohol, and toxins. Kava interferes with these enzymes, especially CYP3A4, CYP2C9, and CYP2C19. That means if you’re taking any medication processed by these enzymes, kava can cause it to build up in your system.
On top of that, kava depletes glutathione, one of your liver’s most important antioxidants. Without enough glutathione, your liver cells become vulnerable to damage. This isn’t theoretical. In 2002, the CDC documented 11 people in the U.S. who needed liver transplants after taking kava. One case from UCLA Health showed a patient’s ALT levels-normally under 17 U/L-spiking to over 2,400 U/L after just 17 weeks of use. That’s liver failure.
Which Medications Are Dangerous with Kava?
If you’re on any of these, kava is a hard no:
- Antidepressants (SSRIs like sertraline, SNRIs like venlafaxine)
- Anxiolytics (benzodiazepines like lorazepam, alprazolam)
- Painkillers (acetaminophen, even in normal doses)
- Birth control pills (ethinyl estradiol and norgestimate)
- Migraine meds (rizatriptan)
- Blood thinners (warfarin, aspirin)
- Statins (atorvastatin, simvastatin)
- Antibiotics (erythromycin, clarithromycin)
Why? Because all of these are metabolized by the same liver enzymes kava blocks. The result? Toxic buildup. One Reddit user reported their ALT jumped to 300 U/L after combining kava with blood pressure meds. Their doctor told them to stop immediately-liver enzymes were already climbing.
Water-Based vs. Organic Extracts: The Real Difference
Not all kava is the same. Traditional Pacific Island preparations use only water and ground root. No alcohol. No chemicals. Just root, water, and time. Studies show this method has been used safely for generations.
But the kava sold in the U.S. and Europe? Most of it is extracted with ethanol or acetone. These solvents pull out different compounds-including flavokawains-that are directly toxic to liver cells. The FDA’s 2020 report points to these non-kavalactone components as the likely culprits behind liver injury. Germany and Switzerland reported 26 cases of liver damage, and every single one involved organic extracts.
If you’re going to use kava, insist on water-based extracts. But even then, caution is still needed.
Who’s at Highest Risk?
Some people are more vulnerable than others. The FDA lists five major risk factors:
- Using organic solvent extracts (not water-based)
- Taking high doses (over 250 mg kavalactones per day)
- Drinking alcohol regularly
- Having pre-existing liver disease (fatty liver, hepatitis, etc.)
- Having genetic variations in liver enzymes (CYP polymorphisms)
Even one of these factors raises the risk. Two or more? That’s a recipe for disaster. A 2022 study from the American Association for the Study of Liver Diseases (AASLD) says anyone with liver disease or on multiple medications should avoid kava entirely.
What Happens When You Combine Kava with Other Drugs?
It doesn’t always happen fast. In the NCBI LiverTox case, symptoms started at 16 weeks: nausea, yellow eyes, dark urine. By week 17, the patient was confused, then comatose. Within weeks, they needed a transplant.
But here’s the scary part: many people don’t tell their doctors they’re taking kava. They think it’s “just a herbal tea.” In Sacramento County, 13 out of 16 liver injury cases involved patients who didn’t mention kava use until after they were hospitalized. One woman took kava for anxiety while on birth control and acetaminophen. Her liver enzymes rose slowly-so slowly her doctor missed it. By the time they tested again, it was too late.
That’s why doctors now ask: “Are you taking any herbs or supplements?”-not just pills.
What Should You Do If You’re Already Taking Kava?
If you’re on any medication and taking kava, stop immediately. Don’t wait for symptoms. Liver damage can be silent until it’s advanced.
Get a liver function test. Ask for ALT, AST, bilirubin, and alkaline phosphatase. Normal ALT is under 17 U/L. Anything above 40 is a red flag. If your numbers are up, stop kava and see a hepatologist.
If you’ve had no symptoms and aren’t on any meds? Still, don’t take it long-term. Even water-based kava shouldn’t be used for more than 3 months at a time. The WHO recommends no more than 240 mg kavalactones per day-and even that’s risky if you’re not monitoring.
Alternatives to Kava for Anxiety
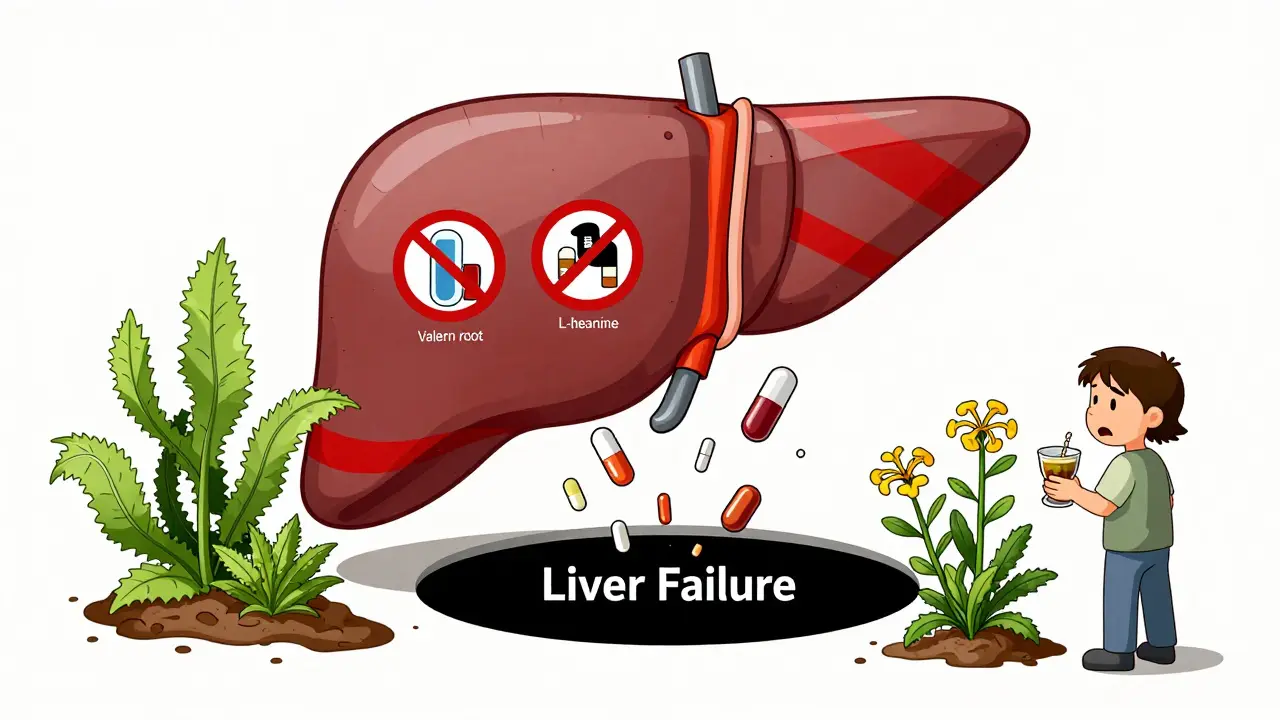
If you’re using kava for anxiety, there are safer options:
- Valerian root (studies show mild calming effects with no liver risk)
- L-theanine (an amino acid in green tea that reduces stress without sedation)
- Passionflower (shown in trials to be as effective as oxazepam, with no liver toxicity)
- Cognitive behavioral therapy (CBT) (proven to work better than any supplement for long-term anxiety)
None of these carry the same risk profile as kava. And none have been linked to liver failure.
Final Reality Check
Kava isn’t banned everywhere because it’s “dangerous.” It’s banned in Australia, Canada, and the EU because it’s predictably dangerous when mixed with common medications. The science is clear. The cases are documented. The liver transplants happened.
Yes, kava works for anxiety. But at what cost? If you’re taking even one prescription or OTC drug, the risk isn’t worth it. And if you’re not? Still, your liver doesn’t have a backup plan. One bad batch. One hidden interaction. One missed blood test. That’s all it takes.
There’s no such thing as a completely safe herbal supplement when your liver is involved. Kava is a reminder that natural doesn’t mean harmless. It means complex. And sometimes, deadly.
Can kava cause liver damage even if I don’t take any other medications?
Yes. While the risk is higher when combined with other drugs, there are documented cases of liver failure in people who only took kava. The issue isn’t just interactions-it’s direct toxicity from compounds like flavokawains in non-traditional extracts. Even water-based kava, when taken in high doses over long periods, has been linked to enzyme elevations and liver stress.
Is it safe to drink kava tea occasionally?
If it’s made from traditional water-based extraction, and you’re healthy, not on any medications, and limit it to 1-2 times per week, the risk is low-but not zero. The WHO and FDA still recommend avoiding long-term use. One study found liver enzyme abnormalities in 15% of people taking kava daily for 6 months-even without other drugs.
How do I know if my kava product is water-based or organic extract?
Check the label. If it says “ethanolic extract,” “acetonic extract,” or “standardized to X% kavalactones,” it’s likely an organic solvent extract. Water-based products will say “traditional water extraction,” “noble kava,” or “Pacific Island style.” If the label doesn’t specify, contact the manufacturer. Most companies won’t answer-because they don’t want you to know.
I took kava and now I feel nauseous and my skin is yellow. What should I do?
Stop kava immediately. Go to an emergency room or urgent care. Ask for a liver function panel (ALT, AST, bilirubin). Yellow skin and nausea are signs of jaundice-your liver is struggling. Do not wait. Liver damage from kava can progress rapidly. Early detection can mean the difference between recovery and transplant.
Are there any supplements that are safer than kava for anxiety?
Yes. Valerian root, L-theanine, and passionflower have all been studied for anxiety with no reports of liver toxicity. CBT, mindfulness, and regular exercise are even more effective long-term. If you need something stronger, talk to your doctor about FDA-approved options. No supplement is worth risking your liver.
What to Do Next
If you’re currently using kava and taking any medication, stop now. Schedule a liver test. Tell your doctor exactly what you’ve been taking-even if you think it’s “just a herb.”
If you’re thinking about starting kava, don’t. There are safer, better-studied ways to manage anxiety. Your liver doesn’t get a second chance. Once it’s damaged, recovery isn’t guaranteed. And if you need a transplant? That’s not a cure-it’s a life sentence.
Kava isn’t the enemy. But it’s not the gentle herb it’s made out to be. It’s a powerful substance with serious risks. And if you’re on meds? That risk is multiplied. Play it safe. Your liver will thank you.

Amber Lane
January 21, 2026 AT 00:50I used kava for months thinking it was harmless. Then my ALT hit 89. My doctor looked me dead in the eye and said, 'Stop. Now.' I didn't even know it could do that.
Now I take L-theanine. No drama. No liver panic.
Jerry Rodrigues
January 21, 2026 AT 05:48Been drinking traditional kava tea from Fiji for years. Never had an issue. But yeah, those solvent extracts? Yeah that stuff’s sketchy.
Don’t blame the plant. Blame the lab.
Samuel Mendoza
January 22, 2026 AT 14:22So you’re telling me natural doesn’t mean safe? Shocking. Next you’ll say water is dangerous if you drink too much.
Also, why are you so scared of herbs? Pharma wants you dependent on pills.
MAHENDRA MEGHWAL
January 23, 2026 AT 11:06Respectfully, the scientific evidence presented herein is both comprehensive and alarming. The hepatotoxic potential of non-traditional kava preparations is well-documented in peer-reviewed literature.
It is my earnest recommendation that individuals under pharmacological treatment refrain entirely from kava consumption, regardless of extraction method.
Dee Monroe
January 23, 2026 AT 20:30I used to think herbs were this gentle, earthy magic - like sipping sunshine and listening to wind chimes. But kava? It’s not a tea. It’s a silent thief.
It doesn’t scream. It doesn’t warn. It just… slowly eats your liver while you’re scrolling Instagram and telling yourself, 'It’s natural, it’s fine.'
And then one day, you’re yellow. And your doctor’s voice sounds like it’s coming from underwater.
It’s not about fear. It’s about respect. Your liver doesn’t have a voice, but it’s been screaming for decades. We just stopped listening.
Maybe we think 'natural' means 'safe' because we want to believe healing can be simple. But biology doesn’t care about our wishes.
It’s not the plant’s fault. It’s not the FDA’s fault. It’s our collective denial that’s the real poison.
We want quick fixes. We want to feel calm without therapy. We want to medicate our modern anxiety with something that sounds like a Hawaiian vacation.
But the liver? It doesn’t go on vacation. It works 24/7. And when you give it something it can’t process? It doesn’t complain. It just… stops.
And then you’re on a transplant list. And your kids are asking why you didn’t listen.
There’s no heroism in surviving. There’s only responsibility.
And if you’re on meds? Just… don’t. There are so many other ways to breathe. You don’t need this.
Malvina Tomja
January 25, 2026 AT 12:40Wow. So you're saying if you're not a perfect, medication-free, organic-eating, yoga-practicing angel, you shouldn't touch kava?
What about people who just want to chill without SSRIs? You're not helping. You're just shaming.
Also, your 'alternatives' are all just placebo tea with a fancy label.
Barbara Mahone
January 25, 2026 AT 20:05Traditional water-based kava from noble cultivars has been consumed safely in the Pacific for millennia.
Modern solvent extracts are not equivalent. The distinction is critical and frequently ignored in Western media.
Labeling all kava as hepatotoxic is scientifically inaccurate and harmful to legitimate cultural practices.
Glenda Marínez Granados
January 27, 2026 AT 01:33So kava’s the villain now? 😂
Next thing you know, someone’s gonna ban sunlight because ‘it can cause skin cancer.’
Also, I take kava with my blood pressure med. My liver’s fine. Coincidence? Maybe. But I’m not scared of a blog post.
Also, CBT? Sounds like a therapist’s sales pitch. I’ll take my plant magic, thanks. 🌿
Yuri Hyuga
January 27, 2026 AT 11:34Let me tell you something - your liver is your silent warrior 🛡️
It filters everything you throw at it - alcohol, coffee, ibuprofen, stress, bad pizza, and yes - kava extracts.
But when you combine it with meds? You’re asking it to run a marathon while carrying a backpack full of bricks.
And then you wonder why it collapses.
Don’t wait for jaundice to be your wake-up call.
Get tested. Talk to your doctor. Try valerian. Try breathwork. Try therapy.
You don’t need a plant to feel calm. You need to stop running from your pain.
And if you’re still reading this? You already know what to do.
Be kind to your body. It’s the only one you’ve got. ❤️
MARILYN ONEILL
January 27, 2026 AT 21:57I’ve been taking kava for years. I’m 32. I’ve never been sick. You people are just scared of anything that’s not a pill.
Also, I don’t trust doctors. They’re just in it for the money.
And L-theanine? That’s just green tea powder. Boring.