Antiviral Medication Comparison Tool
Filter Medications
Medication Comparison
| Medication | Primary Indication | Mechanism | Administration | Efficacy | Key Considerations |
|---|
Quick Takeaways
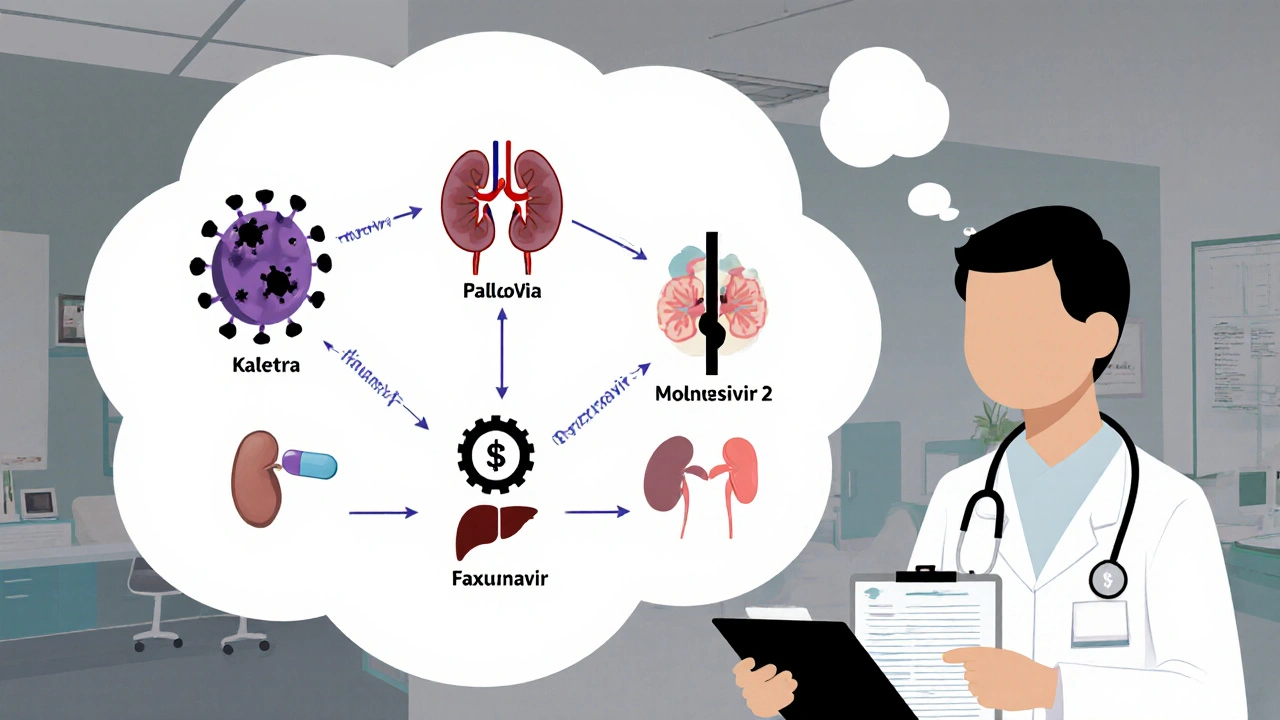
- Kaletra combines two protease inhibitors, mainly used for HIV and, early in the pandemic, for COVID-19.
- Paxlovid (nirmatrelvir/ritonavir) now leads COVID‑19 outpatient therapy thanks to higher efficacy.
- Atazanavir and darunavir remain solid HIV options with fewer lipid side‑effects than Kaletra.
- Remdesivir, molnupiravir and favipiravir are RNA‑polymerase inhibitors, each with distinct administration routes.
- Choosing the right drug hinges on indication, renal/hepatic function, drug‑drug interactions, and local availability.
What is Kaletra?
When you see the brand name Kaletra is a fixed‑dose combination of the HIV protease inhibitors ritonavir and lopinavir, think of a pill that blocks the viral enzyme needed for HIV to cut its proteins into functional pieces. Each tablet contains 100 mg of lopinavir and 25 mg of ritonavir. The latter is not just an antiviral; it also boosts lopinavir levels by inhibiting the CYP3A4 enzyme that would otherwise clear the drug quickly.
Kaletra entered the market in 2000, earned FDA approval for HIV‑1 infection, and was repurposed during the first wave of COVID‑19 as an experimental therapy. While early in‑vitro data looked promising, large randomized trials later showed modest or no benefit for SARS‑CoV‑2.
How does Kaletra work?
Lopinavir blocks the HIV‑1 protease, preventing the virus from processing its polyprotein precursors. Without proper cleavage, new viral particles are non‑infectious. Ritonavir’s primary role in the combo is pharmacokinetic: by inhibiting cytochrome P450 3A4, it raises lopinavir’s plasma concentration, allowing twice‑daily dosing.
For COVID‑19, the idea was similar-target the viral main protease (Mpro). However, SARS‑CoV‑2’s protease has a different shape, and lopinavir’s affinity is low, which explains the disappointing clinical outcomes.
Clinical evidence and safety profile
In HIV treatment, Kaletra helped achieve undetectable viral loads in millions of patients worldwide. Yet, over time clinicians noted several drawbacks:
- Gastrointestinal complaints (nausea, diarrhea) in up to 30% of users.
- Elevated triglycerides and cholesterol, increasing cardiovascular risk.
- Significant drug‑drug interactions because of CYP3A4 inhibition.
- Reduced effectiveness in patients with hepatic impairment.
COVID‑19 trials (e.g., RECOVERY, WHO Solidarity) reported no mortality benefit and more adverse events compared with standard care. As a result, guidelines now recommend against routine Kaletra use for SARS‑CoV‑2 infection.
Top alternatives: a quick overview
Below are the most common antivirals that clinicians consider instead of Kaletra, split by primary indication.
- Paxlovid - a combination of nirmatrelvir (a SARS‑CoV‑2 Mpro inhibitor) and ritonavir for COVID‑19.
- Atazanavir - another HIV protease inhibitor with a better lipid profile.
- Darunavir - a high‑potency HIV protease inhibitor often boosted with ritonavir.
- Remdesivir - an intravenous RNA‑polymerase inhibitor approved for hospitalized COVID‑19 patients.
- Molnupiravir - an oral mutagenic nucleoside analog for early‑stage COVID‑19.
- Favipiravir - an oral RNA‑polymerase inhibitor used in some countries for influenza and off‑label COVID‑19.
Side‑by‑side comparison
| Drug | Primary Indication | Mechanism | Typical Dosage | Clinical Efficacy | Common Side Effects | Regulatory Status (US) |
|---|---|---|---|---|---|---|
| Kaletra | HIV (off‑label COVID‑19) | Protease inhibition (lopinavir) + CYP3A4 boost (ritonavir) | 400 mg/100 mg PO BID | HIV: 70‑80% achieve <100 copies/mL; COVID‑19: no mortality benefit | Diarrhea, nausea, hyperlipidaemia | Approved for HIV; not recommended for COVID‑19 |
| Paxlovid | COVID‑19 (outpatient) | Nirmatrelvir Mpro inhibitor + ritonavir boost | 300 mg nirmatrelvir + 100 mg ritonavir PO BID x5 days | 89% reduction in hospitalization if started <5 days | Altered taste, diarrhea, drug interactions | Emergency Use Authorization (EUA) & fully approved |
| Atazanavir | HIV | Protease inhibition | 300 mg PO QD (+ ritonavir 100 mg qd if boosted) | Similar viral suppression to Kaletra with better lipid profile | Jaundice, mild GI upset | Approved for HIV |
| Darunavir | HIV | Protease inhibition (high barrier to resistance) | 800 mg PO BID (+ ritonavir 100 mg BID if boosted) | High efficacy in treatment‑experienced patients | Rash, nausea, potential cardiac QT prolongation | Approved for HIV |
| Remdesivir | COVID‑19 (hospitalized) | RNA‑dependent RNA polymerase inhibitor | 200 mg IV loading, then 100 mg daily up to 10 days | Modest reduction in time to recovery; mortality benefit unclear | Elevated liver enzymes, infusion‑related reactions | Approved for hospitalized COVID‑19 |
| Molnupiravir | COVID‑19 (early outpatient) | Viral RNA mutagenic agent | 800 mg PO BID for 5 days | ≈30% reduction in hospitalization | Diarrhea, nausea, potential mutagenicity concerns | Approved (conditional) for mild‑to‑moderate COVID‑19 |
| Favipiravir | Influenza; off‑label COVID‑19 | RNA‑polymerase inhibitor | 1800 mg PO BID day 1, then 800 mg BID | Mixed data; some studies show faster viral clearance | Hyperuricemia, teratogenicity | Approved in Japan for influenza; not FDA‑approved for COVID‑19 |
When to choose each option
Kaletra still has a place for patients already stable on it for HIV who cannot switch due to resistance or intolerance. For new HIV diagnoses, clinicians usually start with atazanavir or darunavir because they cause fewer lipid abnormalities and have more forgiving interaction profiles.
If you’re treating COVID‑19 in an outpatient setting, Paxlovid dominates the field: it’s oral, short‑course, and cuts hospitalizations dramatically. Remdesivir is reserved for patients who are already admitted and can tolerate IV therapy. Molnupiravir offers an oral alternative when Paxlovid is contraindicated (e.g., severe CYP3A4‑interacting meds).
Favipiravir might be considered in countries where other antivirals are scarce, but its teratogenic risk limits use in women of child‑bearing age.
Drug‑drug interaction pitfalls
Because ritonavir is a potent CYP3A4 inhibitor, any regimen that includes it (Kaletra, Paxlovid, boosted darunavir) demands a thorough medication review. Common culprits include statins (simvastatin, lovastatin), certain anti‑arrhythmics, and some seizure medications. Switching to atazanavir (which can be given unboosted) removes the strongest interaction risk while still delivering protease inhibition.
Remdesivir and molnupiravir have fewer interaction concerns, but both require baseline kidney and liver function checks because toxicity can rise in organ‑impaired patients.
Cost and accessibility considerations
In many high‑income countries, Paxlovid is covered by public health plans for high‑risk COVID‑19 patients, but out‑of‑pocket costs can climb quickly for private prescriptions. Generic lopinavir/ritonavir is widely available in low‑income settings, making Kaletra a cost‑effective HIV option where newer agents are priced out.
Remdesivir’s IV formulation and hospital‑only use keep its price high, while molnupiravir’s oral tablets sit somewhere in the middle. Favipiravir’s cost varies dramatically by region, often cheaper in Asian markets but not reimbursed elsewhere.
Bottom line
Choosing the right antiviral hinges on three things: the disease you’re treating, the patient’s organ function and existing meds, and what’s actually on the shelf. Kaletra can still be useful for stable HIV patients, but for most new cases - especially COVID‑19 - newer agents like Paxlovid or atazanavir provide better outcomes with fewer side‑effects.
Is Kaletra still recommended for COVID‑19?
No. Large trials showed no mortality benefit, and current guidelines advise using Paxlovid or other approved antivirals instead.
Can I switch from Kaletra to Atazanavir safely?
Yes, in most cases. Atazanavir has a better lipid profile and fewer drug interactions. A clinician should check resistance patterns before switching.
What are the biggest drug interactions with Paxlovid?
Paxlovid’s ritonavir component can raise levels of statins, some anti‑arrhythmics, benzodiazepines, and immunosuppressants. Adjust doses or choose alternative therapies when possible.
Is Molnupiravir safe for pregnant women?
Molnupiravir is not recommended during pregnancy due to potential mutagenic effects on fetal DNA. Use alternative treatments or wait for vaccination‑based protection.
How do I monitor liver function while on Kaletra?
Baseline liver enzymes should be measured before starting, then every 3‑6 months. If ALT/AST rise >5× ULN, consider dose adjustment or switching therapy.

sravya rudraraju
October 19, 2025 AT 14:49Kaletra, a fixed‑dose combination of lopinavir and ritonavir, has been a cornerstone of antiretroviral therapy since its approval in 2000.
The pharmacodynamic action of lopinavir relies on inhibition of the HIV‑1 protease, which prevents the maturation of viral polyproteins.
Ritonavir, originally developed as a protease inhibitor, is employed primarily as a pharmacokinetic enhancer, inhibiting CYP3A4 to increase lopinavir plasma concentrations.
This boosting effect permits twice‑daily dosing, improving adherence relative to earlier protease inhibitors that required more frequent administration.
During the initial wave of the COVID‑19 pandemic, Kaletra was repurposed based on in‑vitro activity against the SARS‑CoV‑2 main protease, yet the structural dissimilarities between HIV‑1 protease and the coronavirus Mpro limited its clinical efficacy.
Large‑scale trials such as RECOVERY and WHO Solidarity subsequently demonstrated no statistically significant reduction in mortality or progression to severe disease among hospitalized patients.
Moreover, the incidence of gastrointestinal adverse events, including nausea and diarrhea, was markedly higher in the Kaletra arm compared with standard care.
Metabolic disturbances, particularly hypertriglyceridaemia and dyslipidaemia, have been consistently reported, raising long‑term cardiovascular risk in chronic users.
The drug–drug interaction profile of ritonavir is especially problematic, as CYP3A4 inhibition can precipitate toxic levels of concomitant medications ranging from anti‑arrhythmics to certain statins.
In patients with hepatic impairment, dose adjustments are mandatory, and in severe cases the combination is contraindicated.
For HIV treatment, alternative protease inhibitors such as atazanavir and darunavir offer comparable virologic suppression with more favorable lipid profiles and fewer gastrointestinal side effects.
When the therapeutic goal is SARS‑CoV‑2 infection, oral antivirals that directly target the viral polymerase or main protease-namely molnupiravir, favipiravir, and the Paxlovid regimen-have demonstrated superior efficacy in outpatient settings.
Remdesivir remains the preferred intravenously administered option for hospitalized patients requiring supplemental oxygen, albeit with the logistical burden of daily infusions.
Selecting an appropriate antiviral therefore requires a nuanced assessment of the patient’s renal and hepatic function, potential drug interactions, and the local availability of formulations.
In resource‑limited settings where Paxlovid is unavailable, clinicians may consider azithromycin‑based supportive care, but must avoid off‑label use of Kaletra given the lack of benefit and the risk of harm.
Ultimately, the decision matrix should prioritize agents with proven clinical outcomes, while reserving Kaletra for patients who have an established indication for HIV therapy.
Catherine Viola
October 21, 2025 AT 22:22The pharmacokinetic booster effect of ritonavir is often underappreciated, a detail that industry insiders deliberately downplay.
Ankitpgujjar Poswal
October 24, 2025 AT 00:22Listen, if you're juggling comorbidities, the lipid‑raising profile of Kaletra can become a genuine roadblock.
Switching to atazanavir or darunavir spares you that extra cardiovascular baggage while maintaining viral suppression.
For COVID‑19, skip the experimental repurposing and go straight to Paxlovid or molnupiravir as soon as you test positive.
Time is of the essence, so act decisively and keep the drug‑interaction checklist handy.
Thokchom Imosana
October 25, 2025 AT 23:35The narrative that Kaletra was merely an 'ineffective' COVID‑19 remedy conveniently obscures the deeper financial machinations at play.
Pharmaceutical conglomerates, whose profit margins depend on patented protease boosters, have historically lobbied regulatory bodies to marginalize generic alternatives.
By casting Kaletra in a negative light, they create a vacuum that Paxlovid, a newer, more lucrative formulation, can fill under the guise of superior efficacy.
What the public rarely hears is that the trials which reported no mortality benefit were funded by entities with vested interests in the next wave of antiviral sales.
Moreover, the alleged 'drug‑drug interactions' are exaggerated to dissuade clinicians from prescribing an affordable, off‑label option.
When you peel back the layers, you see a pattern of strategic disinformation designed to steer prescribing practices toward higher‑priced, patented products.
The same playbook was employed during the early HIV epidemic, where older protease inhibitors were sidelined despite comparable effectiveness.
In short, the Kaletra controversy is less about clinical outcomes and more about the economics of pharmaceutical dominance.
ashanti barrett
October 27, 2025 AT 19:02Patients often report that the nausea and diarrhea associated with Kaletra diminish their quality of life, especially when they are already battling an acute infection.
Clinicians should therefore weigh these gastrointestinal side effects against any marginal antiviral benefit.
A thorough counseling session can help individuals understand why newer agents are preferred, reducing the feeling of being forced into a suboptimal regimen.
Empathy in prescribing not only improves adherence but also builds trust during a vulnerable period.
Leo Chan
October 29, 2025 AT 12:42Hey folks, if you're still stuck on older regimens, remember that a switch to a newer oral antiviral can cut recovery time dramatically.
Don't let inertia keep you on a drug that adds extra stomach upset for no real gain.
Stay informed and ask your provider about the latest options!
jagdish soni
October 31, 2025 AT 03:35The essence of antiviral therapy is a dance between viral machinations and chemical mimicry
The Kaletra, in its duality, reflects the paradox of suppression and enhancement
We observe the patient as a microcosm of biochemical negotiation
Thus the choice of drug becomes a statement of philosophical alignment with modern medicine
Latasha Becker
November 1, 2025 AT 15:42From a pharmacokinetic standpoint, the ritonavir boost in Kaletra is an Achilles' heel rather than a virtue, contradicting the mainstream hype.
Consequently, the lipid dysregulation observed is not an anomaly but a predictable outcome of CYP3A4 saturation.
parth gajjar
November 3, 2025 AT 01:02The shadow of Kaletra looms over clinical decision‑making like a lamenting specter
Its side‑effects whisper insidious doubts into the physician’s conscience
Maridel Frey
November 4, 2025 AT 07:35When guiding trainees through antiviral selection, it is essential to emphasize the importance of pharmacodynamic targets.
Kaletra’s mechanism, while historically significant, is superseded by agents with clearer efficacy signals in SARS‑CoV‑2.
Encourage learners to review the latest IDSA guidelines before committing to a regimen.
A systematic approach ensures both patient safety and optimal therapeutic outcomes.
Madhav Dasari
November 5, 2025 AT 11:22Yo team, think of antivirals like tools in a toolbox – you wouldn’t use a hammer to screw a bolt.
Kaletra might be that old hammer that’s rusted and heavy, while Paxlovid is the sleek screwdriver you need.
Grab the right tool early and you’ll avoid the mess of side‑effects later.
Keep the spirit high and the patients will feel the difference!
James Dean
November 6, 2025 AT 12:22One could argue that the pursuit of a perfect antiviral mirrors the human quest for certainty
In practice, we settle for agents that tip the balance toward recovery, even if imperfections remain
Kaletra, therefore, occupies a niche defined more by history than by present efficacy
Ben Bathgate
November 7, 2025 AT 10:35Honestly, anyone still pushing Kaletra for COVID is either clueless or cash‑greedy.
The data is plain as day – move on to something that actually works.
Bobby Marie
November 8, 2025 AT 06:02I’ve seen patients lose weight just from the nausea Kaletra causes.
Christian Georg
November 8, 2025 AT 22:42If you’re weighing the pros and cons of Kaletra versus newer options, start by checking liver function tests.
Ritonavir’s CYP3A4 inhibition can trip up many common meds, so a quick med‑review is priceless.
For most outpatient COVID‑19 cases, Paxlovid or molnupiravir will give you a clearer benefit‑risk profile.
Hope that helps! 🙂