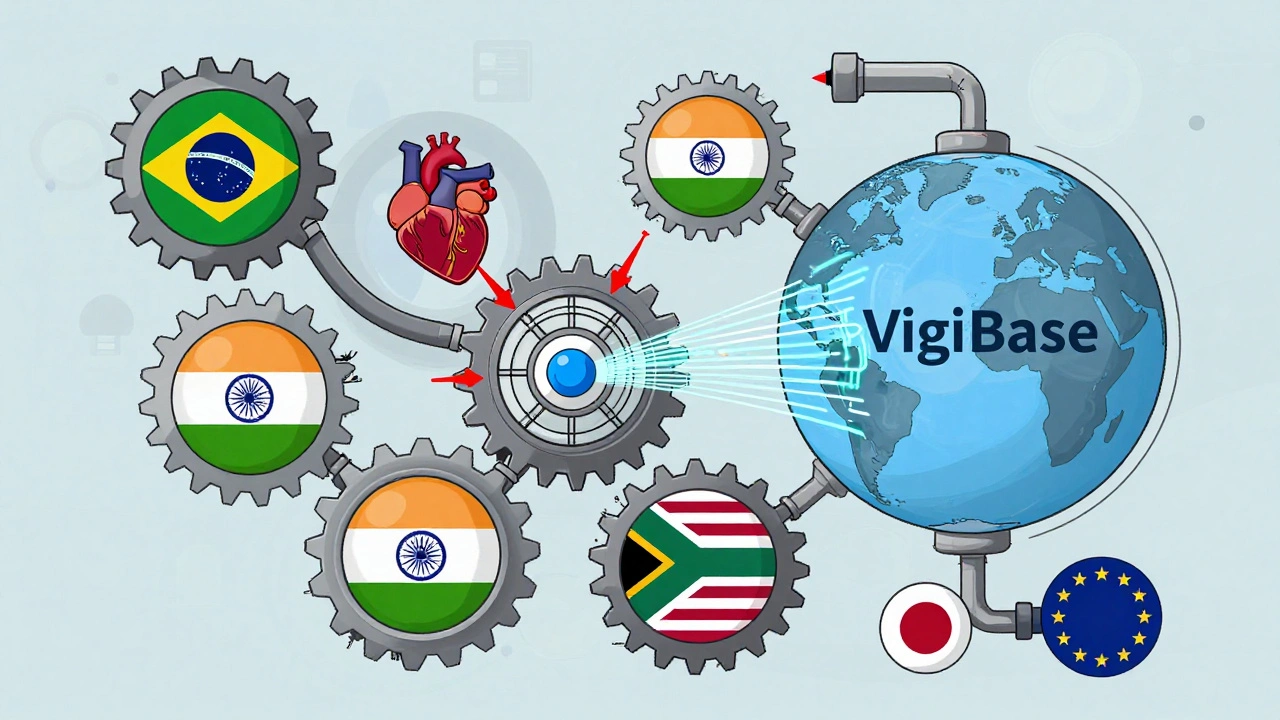
Every year, millions of people take generic medicines made in one country and used in another. But what happens when something goes wrong? A patient in Brazil has a rare reaction to a drug made in India, sold in South Africa, and approved by the FDA. Who tracks it? How fast does the system respond? This is where pharmacovigilance harmonization comes in - the quiet, complex effort to make sure drug safety monitoring works the same way no matter where you live.
Why harmonization matters more than ever
Before 1990, every country had its own rules for reporting side effects. A drug company had to submit five different reports for the same adverse event - one each for the U.S., EU, Japan, Canada, and Australia. That meant delays. Missed signals. And worse - preventable harm. The International Council for Harmonisation (ICH) was created to fix that. Today, its E2 series of guidelines - especially E2B(R3) - are the global standard for how adverse drug reactions get reported electronically. Companies that follow these rules can submit one report that 134 countries accept. That’s not just efficiency. It’s life-saving. The numbers prove it. The FDA estimates that harmonization cuts time to market by 15-20%. It prevents 2.5 million patients from being unnecessarily enrolled in duplicate clinical trials each year. And according to Novartis, using a single global safety database reduced duplicate case entry by 92%. That’s 92% less paperwork, less confusion, and faster responses when something dangerous pops up.How the big players do it differently
Even with harmonization, differences remain. The European Medicines Agency (EMA) requires every new drug to have a full Risk Management Plan (RMP). That means detailed plans for monitoring side effects, even for common drugs. The U.S. FDA? They only require Risk Evaluation and Mitigation Strategies (REMS) for about 1.2% of drugs - the ones with the highest risk. Then there’s Japan. The PMDA uses data from 12 million patient records in its J-STAR system to catch signals early. China demands local adverse event reports within 15 days - the same deadline as the U.S. - forcing global companies to report the same event twice. Canada requires serious events to be reported within 30 days. And the WHO’s VigiBase? It’s the world’s largest database, holding over 35 million individual case reports from 134 countries. It’s not just a backup - it’s a global early warning system. These differences aren’t just bureaucratic. They cost money. TransCelerate Biopharma found that inconsistent rules increase pharmacovigilance costs by 22% for multinational companies. One pharmacist on Reddit said they spend 35-40% of their time just formatting reports for different regions. That’s hours that could be spent analyzing real safety signals instead of chasing formatting rules.Technology is changing the game
The old way of monitoring drug safety relied on manual reviews of paper reports. Today, AI and machine learning are doing the heavy lifting. Since 2022, both the EMA and FDA have used AI to scan safety data. The results? Signal detection is 30-40% faster. Japan’s PMDA cut false alarms by 25% using AI models trained on local data. Real-world data (RWD) is another game-changer. The EU now requires electronic health records (EHRs) to feed into safety monitoring. The FDA’s Sentinel Initiative tracks 300 million patient records. EMA’s DARWIN EU covers 100 million. That’s not just data - it’s a living safety net. But not everyone has access. In Brazil and South Africa, less than 15% of potential RWD sources can even be processed. In low- and middle-income countries, 74% of pharmacovigilance staff say they lack the resources to meet even basic ICH standards. That’s a huge gap. A drug might be safe in Germany but dangerous in Nigeria - and we won’t know until it’s too late.
The human cost of misalignment
Harmonization isn’t just about paperwork. It’s about saving lives. Deloitte projects that full global harmonization could prevent 1,200-1,500 drug-related deaths each year by catching dangerous signals faster. But right now, there’s a $1.8 billion funding gap for pharmacovigilance systems in poorer countries. And it’s not just about money. It’s about training. As of 2024, 76% of top pharmaceutical companies require their pharmacovigilance staff to understand machine learning basics. That’s a big shift. You can’t just be a pharmacist anymore. You need to know data science, coding, and AI validation. Even technical standards aren’t perfect. EMA found that 18-22% of safety reports get rejected because of incorrect MedDRA coding - the universal language for describing side effects. One wrong code, and your report gets bounced. That’s a delay. A missed signal. A potential risk.What’s next? The road to true global safety
The WHO’s Global Smart Pharmacovigilance Strategy, updated in October 2024, aims to set common data standards across 150 countries by 2027. That’s ambitious. But progress is happening. In January 2024, the FDA, EMA, and PMDA formed a Joint Pharmacovigilance Task Force. They’ve already aligned 78% of their risk management requirements for new biologic drugs. The ICH is working on new AI validation standards, due by mid-2026. That’s huge. Right now, every company builds its own AI model. If they all use the same validation rules, we’ll get more reliable, consistent results. But here’s the truth: Harmonization isn’t about making everyone the same. It’s about making sure the system works together. A drug approved in the U.S. should be monitored with the same urgency in Kenya or Indonesia. The technology exists. The guidelines exist. What’s missing is the will - and the funding - to bring every country up to speed.

Aidan Stacey
December 11, 2025 AT 13:43This is the kind of work that actually saves lives, not just moves paper around. I’ve seen firsthand how fragmented systems delay responses - I worked with a team that missed a cardiac signal for six months because the report got stuck in translation between regional portals. Now? AI catches it in hours. That’s not tech hype - that’s a mother in Nairobi getting her child’s drug warning before the local clinic runs out of stock. We’re not just harmonizing forms. We’re harmonizing humanity.
Katherine Liu-Bevan
December 12, 2025 AT 09:45The 92% reduction in duplicate case entry by Novartis is the most compelling statistic here. It’s not just about cost - it’s about cognitive load. Pharmacovigilance staff aren’t clerks; they’re frontline analysts. When you remove redundant data entry, you free up bandwidth to detect patterns, not just file reports. The real win isn’t the ICH guidelines - it’s the fact that people can finally focus on what matters: the patient, not the form field.
Aman deep
December 12, 2025 AT 18:20as someone from india where most generics are made - this hits home. we churn out meds for the world but our own reporting system? barely functional. my cousin got a rash from a common antibiotic and the local hospital didn’t even know how to file a report. no one trained. no e-system. just a notebook in a drawer. i’m glad the world is catching up but why does it take a crisis in brazil or south africa for us to get serious? we need more than guidelines - we need boots on the ground, not just cloud servers.
Sylvia Frenzel
December 13, 2025 AT 11:10Let’s be real - this whole harmonization push is just the EU and FDA forcing their rules on everyone else under the guise of ‘global standards.’ Why should India or Nigeria follow E2B(R3) when they can’t even afford basic lab equipment? This isn’t progress - it’s digital colonialism dressed up in compliance jargon.
Doris Lee
December 15, 2025 AT 04:25Every time a country joins VigiBase, it’s a tiny victory. We’re not fixing everything overnight but we’re moving. And that’s enough to be hopeful about.
Vivian Amadi
December 15, 2025 AT 11:5218-22% of reports get rejected because of MedDRA coding errors? That’s unacceptable. This isn’t rocket science - it’s basic training. If your team can’t code a rash correctly, they shouldn’t be touching safety data. Fix the people, not the system.
Monica Evan
December 15, 2025 AT 16:40Back in 2018, I helped train pharmacovigilance staff in Ghana. We had one laptop, no internet, and a printer that only worked on Tuesdays. We printed reports, mailed them to Accra, then waited six weeks for confirmation. Now? They’re using WhatsApp to send photos of adverse events to a central AI triage system. That’s not magic - it’s creativity under constraints. The tech exists. The will? That’s the real bottleneck. And honestly? It’s not always money. Sometimes it’s just someone believing it’s possible.
Taylor Dressler
December 15, 2025 AT 21:09Monica’s point about Ghana is exactly why I’m optimistic. We don’t need every country to look like the FDA. We need them to be able to speak the same safety language. The Joint Task Force aligning 78% of biologic risk requirements? That’s the blueprint. Now scale it. Train local staff. Fund local tech. Let them adapt the standards, not just adopt them. Harmonization isn’t uniformity - it’s interoperability. And that’s something every country can own.