Immunosuppressant Drug Interaction Checker
Check Drug Interactions
When you're on immunosuppressants after a transplant or for an autoimmune disease, even small changes in your medication routine can have big consequences. Two of the most common drugs - azathioprine and mycophenolate - work differently, interact with other drugs in unique ways, and affect your body in ways you can't always feel. Getting this wrong can mean severe infections, organ rejection, or even cancer. This isn't theoretical. Real patients have ended up in the hospital because of these interactions.
How Azathioprine and Mycophenolate Actually Work
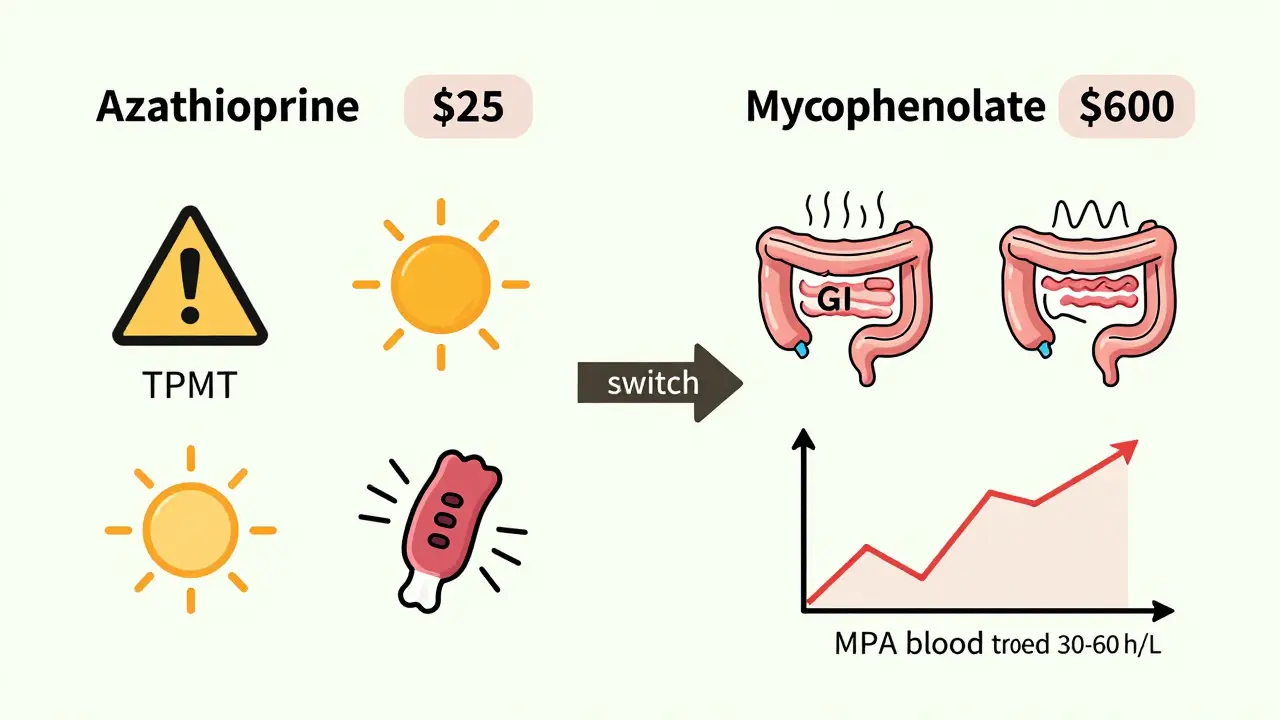
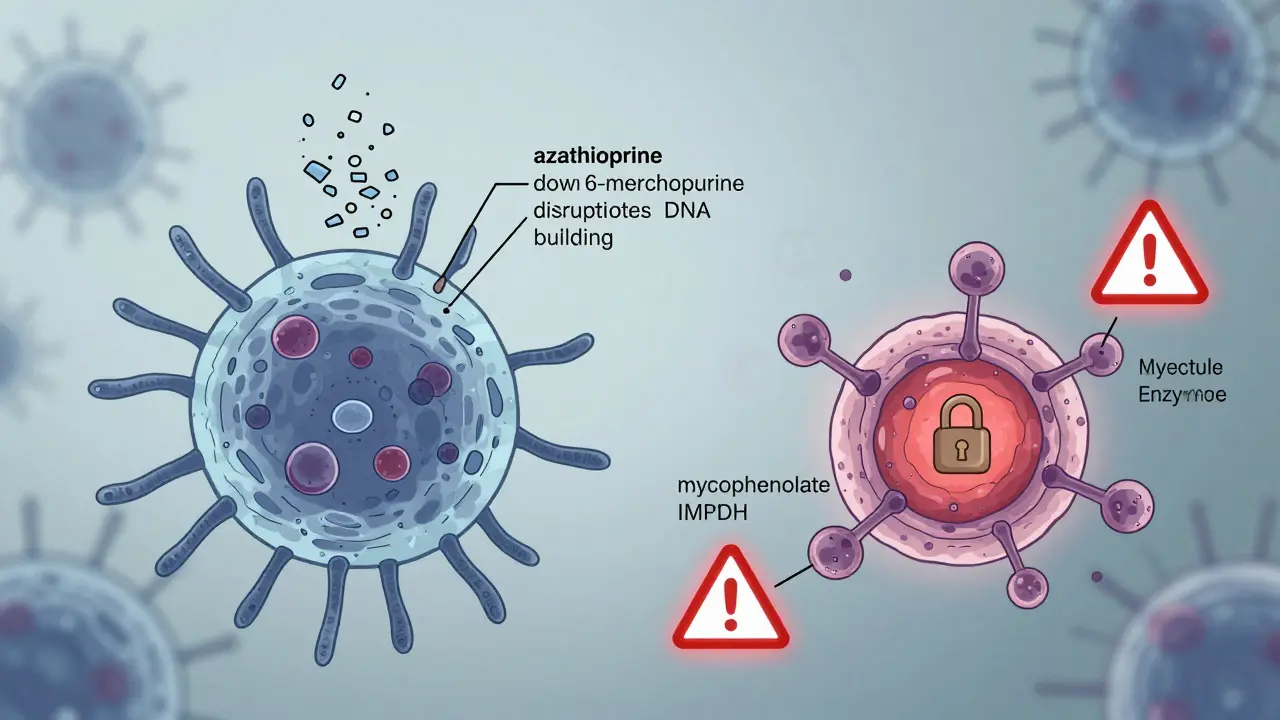
Azathioprine and mycophenolate both stop your immune system from attacking your new organ or your own tissues, but they do it in completely different ways. Azathioprine breaks down into 6-mercaptopurine, which then turns into compounds that mess with DNA building blocks. This slows down the growth of immune cells, especially T-cells and B-cells. It’s been around since the 1960s and is cheap - generic versions cost about $25 a month.
Mycophenolate, on the other hand, blocks a specific enzyme called IMPDH. That enzyme is needed for immune cells to make guanine, a key part of DNA. Without it, those cells can’t multiply fast enough to cause damage. The active form, mycophenolic acid (MPA), is more targeted than azathioprine. That’s why it’s now the go-to drug for 70% of kidney transplant patients in the U.S. and up to 85% in Europe.
But here’s the catch: neither drug works the same in everyone. Azathioprine’s effect depends heavily on an enzyme called TPMT. About 11% of people have reduced TPMT activity, and 0.3% have almost none. If you’re in that group and take the standard dose, your body builds up toxic levels of active metabolites. That can crash your white blood cell count in days. That’s why TPMT testing is required before starting azathioprine - it’s not optional.
Key Drug Interactions You Can’t Ignore
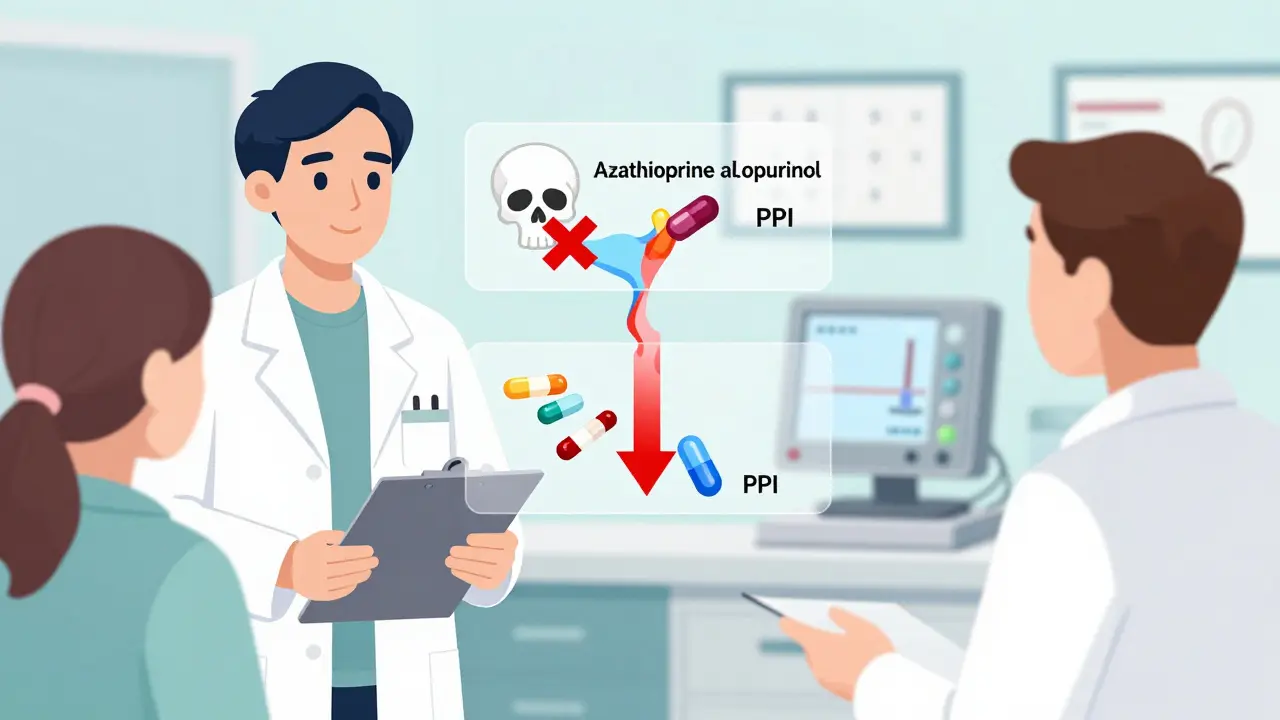
Some interactions are deadly. The most dangerous one involves azathioprine and allopurinol. Allopurinol is used for gout and kidney stones, and it’s often prescribed alongside azathioprine. But combining them increases the risk of life-threatening bone marrow suppression by 6.3 times. The FDA has a black box warning for this. If you need allopurinol, your azathioprine dose must be cut by 75% - and even then, you need weekly blood tests.
Mycophenolate has its own set of traps. Proton pump inhibitors (PPIs) like omeprazole or pantoprazole - commonly used for heartburn - can reduce mycophenolate absorption by 25-35%. In lupus nephritis patients, that means the drug doesn’t reach the kidneys effectively. One study found patients on PPIs had twice the rate of kidney flare-ups. The fix? Switch to an H2 blocker like famotidine, or increase the mycophenolate dose under close monitoring.
Cyclosporine also interferes with mycophenolate. It blocks the recycling of MPA in the gut, lowering its blood levels by 35-50%. That’s why when patients switch from cyclosporine to tacrolimus, their mycophenolate dose often needs to go up. If you don’t adjust it, rejection can happen silently - no symptoms, just rising creatinine levels.
Side Effects and Tolerability: What Patients Really Experience
Doctors talk about side effects in percentages, but patients live them. For azathioprine, the biggest complaints are sun sensitivity and pancreatitis. One patient on Reddit described getting severe sunburns after walking to the mailbox. Another developed pancreatitis two weeks after starting the drug - a known 4% risk. Blood counts drop, too. If your neutrophils fall below 1,000 per microliter within two weeks, stop the drug immediately.
Mycophenolate’s worst side effect is gastrointestinal trouble. Up to 40% of patients get diarrhea, nausea, or vomiting. That’s why many switch to the enteric-coated version (EC-MPS or Myfortic). One transplant patient said it took three different formulations before he found one he could tolerate. Still, 45% of mycophenolate users report GI issues severe enough to reduce their dose.
But here’s something surprising: despite the GI problems, patient adherence is higher with mycophenolate. Why? Fewer blood count issues. Azathioprine causes low white cells, low platelets, and anemia more often - 28% more than mycophenolate. Patients feel better overall, even if they have stomach upset.
Efficacy: Which Drug Works Better?
Head-to-head studies show mycophenolate wins in most autoimmune conditions. In autoimmune hepatitis, a Dutch trial found 68% of patients on mycophenolate reached normal liver enzymes and IgG levels, compared to 46% on azathioprine. In lupus nephritis, the ALMS trial showed 56% complete kidney response with mycophenolate versus 42% with azathioprine.
But azathioprine still has its place. In inflammatory bowel disease - especially Crohn’s - azathioprine works in 65% of cases. Mycophenolate? Only 35%. That’s why many GI specialists still start with azathioprine for IBD.
Cost matters too. Mycophenolate costs about $600 a month. Azathioprine is $25. In places with limited healthcare access, azathioprine remains the only option. Even in the U.S., some patients skip doses because they can’t afford it. One survey found 65% of mycophenolate users skipped pills due to cost.
Practical Tips for Safe Use
- For azathioprine: Get TPMT testing before starting. Never combine with allopurinol without a 75% dose reduction. Monitor CBC weekly for the first month. Avoid excessive sun exposure - wear UPF 50+ clothing.
- For mycophenolate: Take on an empty stomach - one hour before or two hours after meals. Separate from antacids, iron, or calcium supplements by at least two hours. Avoid PPIs if possible. If you must take them, check MPA blood levels. Use EC-MPS if GI side effects are bad.
- For both: Get regular blood tests. Watch for fever, sore throat, or unexplained bruising - signs of low white cells or platelets. Report any new rash or skin changes immediately - both drugs raise skin cancer risk.
What’s New and What’s Coming
There’s progress. In 2023, a new delayed-release mycophenolate tablet (Myfortic DR) hit the market with 28% fewer GI side effects in trials. The FDA also approved a TPMT genotype-guided dosing calculator that’s already cut azathioprine toxicity by 37% in clinics using it.
The IMPROVE trial, which ended in late 2024, compared fixed-dose mycophenolate to personalized dosing based on blood levels. Early results suggest targeting MPA levels between 30-60 mg·h/L reduces rejection and side effects. This could soon become standard.
But don’t expect azathioprine to disappear. It’s too cheap, too well-understood, and still effective in IBD. Mycophenolate will dominate transplant medicine, but azathioprine holds on in resource-limited settings and specific autoimmune cases.
Final Takeaway
Neither drug is perfect. Azathioprine is affordable and effective in some conditions, but carries higher cancer and bone marrow risks. Mycophenolate is more effective in most transplant and autoimmune cases, but it’s expensive and hard on the gut. The right choice depends on your condition, your genetics, your budget, and your tolerance for side effects.
There’s no one-size-fits-all. That’s why you need a team - a transplant pharmacist, a rheumatologist, a nephrologist - working together. Don’t assume your doctor knows every interaction. Bring a list of all your meds, including OTC and supplements. Ask: "Is this safe with my immunosuppressant?" If they hesitate, get a second opinion.
These drugs save lives. But they demand respect. One missed dose, one wrong combination, one ignored symptom - and the consequences can be irreversible.
Can I take azathioprine and mycophenolate together?
While some guidelines say the combination increases side effects, recent studies show it’s safe in most cases when used sequentially - like switching from azathioprine to mycophenolate after a flare. But combining them from the start is not standard practice. Most transplant centers avoid it due to overlapping bone marrow suppression risks. Always discuss this with your transplant team.
How do I know if my mycophenolate dose is too low?
Signs your dose may be too low include rising creatinine levels, new protein in your urine, or a positive donor-specific antibody test. If you’re on a PPI, taking it with food, or have kidney disease, your MPA levels might be low even if you’re taking the right dose. A blood test measuring MPA AUC (area under the curve) is the only way to be sure. Target range is 30-60 mg·h/L.
Why does my doctor want me to avoid antacids with mycophenolate?
Antacids, iron supplements, calcium, and magnesium bind to mycophenolate in the gut and block its absorption. This can cut your drug levels by 25% or more. Even a Tums or a daily calcium pill can interfere. Take these at least two hours before or after your mycophenolate. The enteric-coated version (Myfortic) is less affected, but still not immune.
Is mycophenolate safer than azathioprine for long-term use?
Yes, for most people. Long-term studies show azathioprine carries a 2.1-fold higher risk of lymphoma compared to mycophenolate. It also causes more bone marrow suppression and skin cancers. Mycophenolate has a lower cancer risk and better safety profile over 10+ years. That’s why it’s now the preferred choice for younger transplant recipients.
What should I do if I miss a dose of mycophenolate?
If you miss a dose, take it as soon as you remember - unless it’s within two hours of your next dose. Then skip it. Never double up. Missing doses increases rejection risk, especially in the first year after transplant. Set phone alarms, use a pill organizer, and keep extra prescriptions on hand. If you miss more than two doses in a week, call your transplant team.
Can I drink alcohol while taking azathioprine or mycophenolate?
Moderate alcohol is generally okay, but heavy drinking increases liver stress and can worsen azathioprine-related liver toxicity. It also raises your risk of pancreatitis with azathioprine. With mycophenolate, alcohol doesn’t directly interact, but it can make GI side effects worse. Most doctors recommend limiting alcohol to one drink per day - if at all.

Ambrose Curtis
January 29, 2026 AT 01:41Just had my third kidney transplant last year and switched from azathioprine to mycophenolate after my TPMT came back low. Dude, the difference in my energy? Night and day. No more random fevers, no more wiping out my WBCs every other month. But the GI stuff? Oh yeah. I was puking like a drunk sailor for two weeks until I switched to Myfortic. Now I take it on an empty stomach like a monk and never look back. Also, avoid Tums like the plague. Learned that the hard way.
Brittany Fiddes
January 29, 2026 AT 16:01Ugh, I can't believe Americans still think azathioprine is a 'budget option'. It's 2024. We're talking about life-or-death immunosuppression here. If you can't afford mycophenolate, you're not just being cheap-you're gambling with your graft. And don't even get me started on people skipping doses because they 'can't afford it'. That's not financial hardship, that's negligence. In the UK, we have access to these meds through the NHS. You don't get to treat your transplant like a discount pharmacy experiment.
Katie Mccreary
January 29, 2026 AT 19:01You're all missing the real issue: no one checks MPA levels. Ever. My nephrologist said 'just take it' and that was it. Two months later, my creatinine spiked. Turned out my levels were half the target. They don't care until you're in rejection mode. Classic.
matthew martin
January 30, 2026 AT 15:26Bro, I used to take my mycophenolate with breakfast like a normal person. Then I started getting diarrhea so bad I had to quit my job. Found out later that my calcium pill was blocking absorption. Now I take it at 7 AM, then wait until 9:30 for my coffee and vitamins. Life changed. Also, the new delayed-release version? Game changer. No more feeling like I’m digesting razor blades. If you’re struggling with GI stuff, just ask your pharmacist for Myfortic DR. They’ll hook you up.
Anna Lou Chen
January 31, 2026 AT 20:54It's fascinating how we've reduced complex immunological dynamics to a binary choice between two molecules. Azathioprine versus mycophenolate isn't a pharmacological debate-it's a metaphysical one. The former represents the industrial, cost-driven, paternalistic model of care; the latter, the neoliberal, personalized, bio-capitalist ideal. We're not choosing drugs-we're choosing ideologies. And yet, no one asks: who benefits from this dichotomy? The pharma conglomerates, of course. The patient? Just another data point in the algorithm.
Kevin Kennett
February 1, 2026 AT 20:53My wife’s on both drugs right now-switched from azathioprine after her liver flare. Doc said it’s okay if we space them out and monitor her counts like hawks. She’s been on it for 8 months and hasn’t had a single infection. I know people say don’t combine them, but if your team is on top of it? It works. Just don’t wing it. We get blood drawn every two weeks. No drama. Just discipline.
Phil Davis
February 3, 2026 AT 20:01So let me get this straight… you’re telling me I need to take my mycophenolate on an empty stomach, avoid every antacid in the pharmacy, stop drinking coffee for two hours, and get blood tests every week… just so I don’t reject my kidney? And this is the 'modern' standard of care? I miss the 90s. Back then, you just took the pill and hoped for the best. At least we had faith.
Jess Bevis
February 4, 2026 AT 00:52From Nigeria: we don’t get mycophenolate. Ever. Azathioprine is it. And yeah, people die from low TPMT. But we still use it because it’s $20 a month. No one tests TPMT here. No one can afford it. We pray more than we test. If you think this is easy in the U.S., you haven’t met someone who’s had to choose between meds and rent.
Amber Daugs
February 4, 2026 AT 01:41Someone just said 'I take it with food' and I lost it. Do you even know what you're doing? You're not just risking rejection-you're risking your life. And you think it's okay to treat this like a vitamin? No. This is not a suggestion. This is a medical protocol. If you don't follow it, you're not a patient-you're a liability. And your doctor deserves better than your ignorance.
Howard Esakov
February 4, 2026 AT 15:01My doctor told me to avoid allopurinol. I didn’t listen. Took it for my gout. Two weeks later, I was in the ICU with a WBC of 300. I thought I was being 'resourceful'. Turns out, I was just stupid. Now I use colchicine instead. And I check my meds with a pharmacist before I even think about swallowing anything. If you’re not doing this, you’re playing Russian roulette with your immune system. 🤡
Kathy Scaman
February 5, 2026 AT 17:34Just started mycophenolate last month. The diarrhea is brutal. But honestly? I’d rather have that than feel like I’m slowly dying from low blood counts. Azathioprine made me feel like a ghost. This? I just feel like I need to be near a bathroom. Small trade-offs, right? 😅
Irebami Soyinka
February 6, 2026 AT 12:25My doctor in Lagos told me azathioprine is 'good enough' for Africans. I told him to shut up. I'm not a statistic. I'm not a cost-saving experiment. I'm a person. I ordered mycophenolate from Canada. Paid $500 out of pocket. Took it for 6 months. My kidney function improved. Now I'm fighting to get it covered locally. If you think your life is worth less because of your passport, you're wrong. 💪🌍