Managing multiple pharmacies and prescribers for seniors isn’t just about logistics-it’s about preventing life-threatening mistakes. When an older adult sees three different doctors, fills prescriptions at two pharmacies, and takes seven medications daily, the risk of errors skyrockets. Duplicates, dangerous interactions, missed refills, and incorrect dosages aren’t rare-they happen every day. But there’s a way to fix this: centralized pharmacy management systems.
Why Centralized Systems Are Non-Negotiable for Senior Care
Without a unified system, each pharmacy works in isolation. One pharmacy might not know that another filled a blood thinner the day before. A prescriber might not realize a patient’s local pharmacy already has a similar medication on file. This isn’t hypothetical. Studies show that 1.3% of prescriptions in multi-location scenarios contain errors simply because drug names or dosages weren’t standardized across locations. For seniors, that’s not a small number-it’s a death sentence waiting to happen. Centralized systems solve this by creating one master drug file. Every pharmacy in the network uses the same NDC codes, brand names, and dosage instructions. If a doctor in Chicago prescribes “Lisinopril 10mg,” every pharmacy from Florida to Ohio recognizes it the same way. No confusion. No guesswork. This alone cuts medication errors caused by naming inconsistencies by up to 17%, according to Dr. William Eggleston of Binghamton University.How the Best Systems Work Behind the Scenes
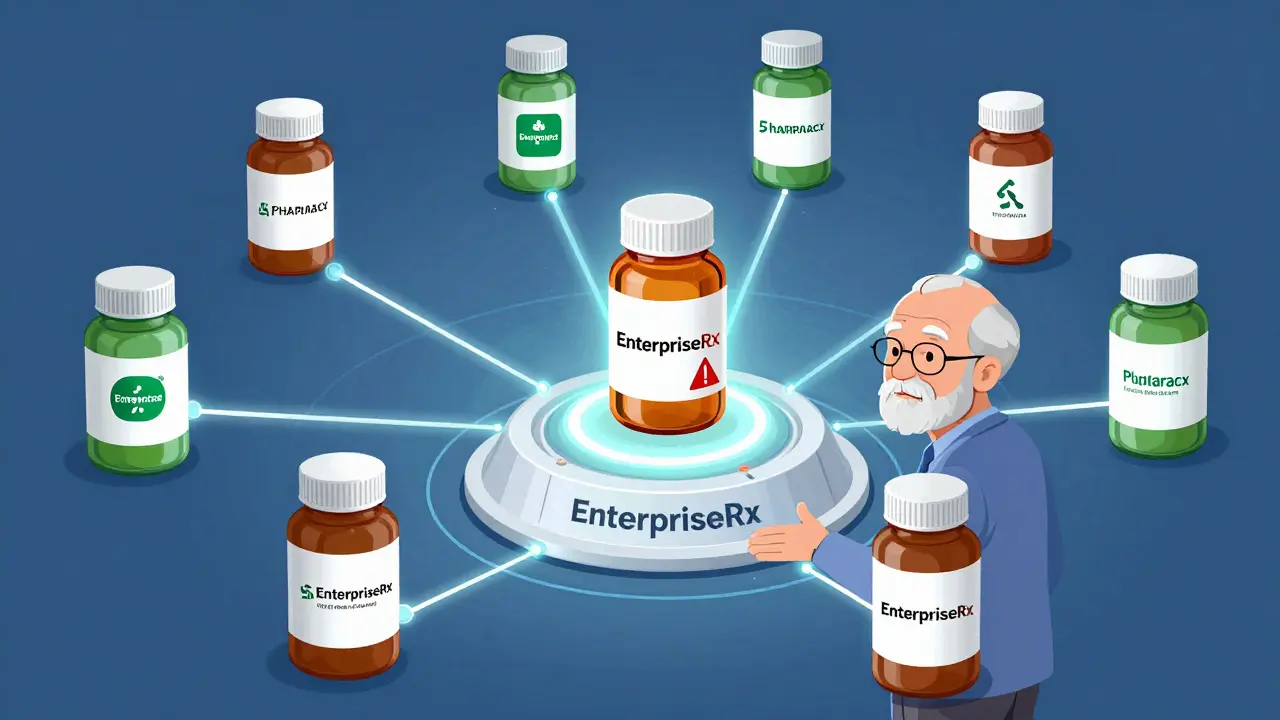
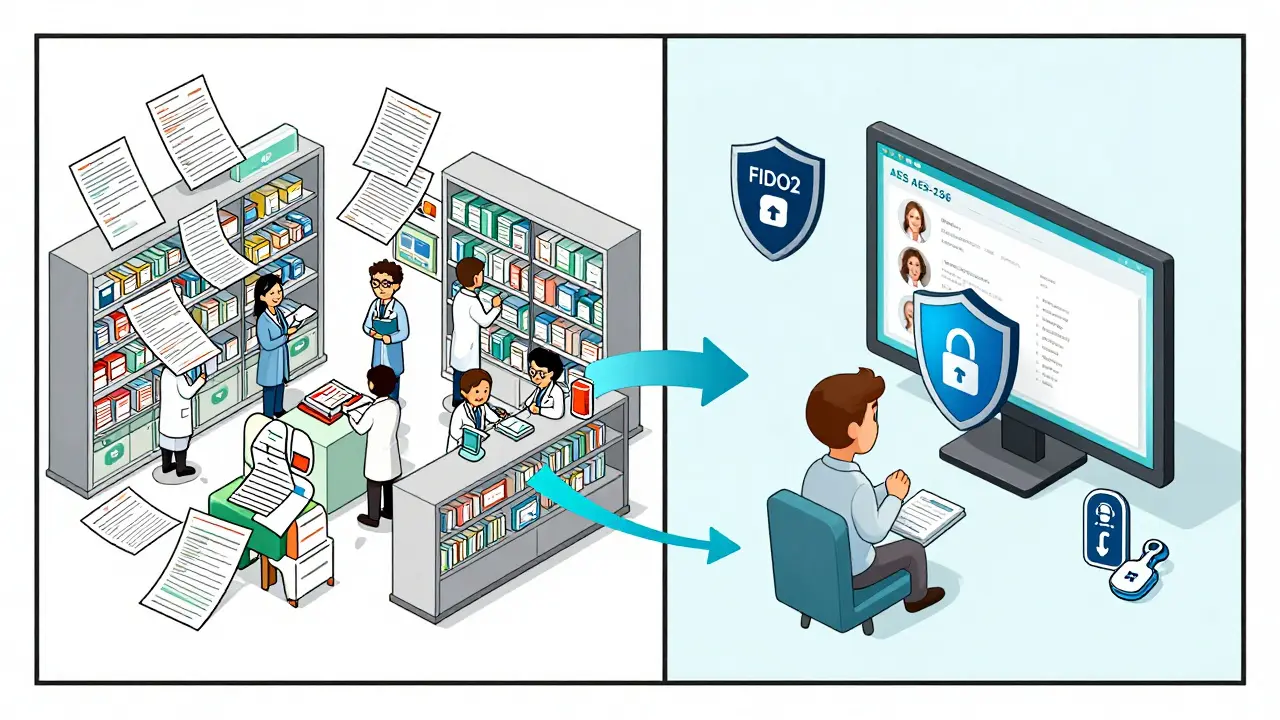
Top platforms like EnterpriseRx by McKesson a high-level pharmacy management software designed for multi-location chains, with real-time prescription processing and integrated EHR connectivity and PrimeRx by PioneerRX a cloud-based pharmacy system with seamless cross-location patient record access and preferred pickup functionality don’t just store data-they actively protect patients. These systems sync daily, sometimes hourly, across all locations. If a senior’s daughter in Atlanta calls to refill a prescription, the system checks every pharmacy where that patient has ever filled a script. It flags duplicates, checks for interactions with other medications, and alerts the pharmacist if a new prescriber is prescribing something that conflicts with an existing regimen. The infrastructure is built for reliability. EnterpriseRx runs on Windows 10 or newer servers with at least 8GB RAM and 500GB storage. PrimeRx maintains 99.98% uptime, verified over two full years. All data is encrypted with AES-256, the same standard banks use. And with FIDO2 security keys, only authorized staff can access house accounts or approve transfers-cutting unauthorized access by 94%.Key Features That Save Lives
Not all systems are created equal. Here’s what actually matters when choosing one:- Universal Drug Database - Ensures every pharmacy uses the same names and codes. Prevents confusion between brand and generic versions.
- Real-Time Patient Profiles - Every medication, allergy, and prescriber is visible across all locations. No more “I didn’t know they were on warfarin.”
- Automated Transfer Protocols - If a senior moves or switches pharmacies, the system moves their entire profile, including refill history and notes from pharmacists.
- Watchdog Monitoring - Systems like Datascan’s AI Watchdog 2.0 scan for patterns that suggest drug diversion or overprescribing. In beta testing, it caught 92.4% of suspicious activity.
- Prescriber Communication Hubs - EnterpriseRx now integrates directly with Epic EHR, letting pharmacists message prescribers in real time. This cuts communication-related errors by 18%.
What Happens Without a Central System?
Chains using outdated, standalone software face serious risks. A 2024 audit by the National Pharmacist Association found that 23% of multi-location pharmacies without centralized systems had billing and prescription discrepancies between locations. That means a senior might be billed twice for the same drug-or worse, not billed at all, leading to missed refills. Worse, local pharmacists can’t always verify transferred prescriptions. Dr. Linda Tyler from Mayo Clinic warns that 12% of medication errors in chains happen because the receiving pharmacist doesn’t double-check what was sent. Centralized systems fix this by forcing a review step before any transfer is completed.Choosing the Right System for Your Chain
There’s no one-size-fits-all, but here’s how to pick:| System | Best For | Monthly Cost per Location | Key Strength | Limitation |
|---|---|---|---|---|
| EnterpriseRx by McKesson | Large chains with 10+ locations | $325-$450 | Real-time prescription balancing and EHR integration | Steep learning curve; requires 8-12 weeks to implement |
| PrimeRx by PioneerRX | Chains focused on patient convenience | $399 | Seamless pickup location switching and 99.98% uptime | Less robust clinical decision support |
| DocStation | Chains offering clinical services | $349 | 87% revenue increase in vaccines and clinical services | Weak inventory management tools |
| Datarithm | Chains struggling with inventory waste | $279 | 28% reduction in inventory-related errors | Not designed for complex prescriber coordination |
| PharmacyOne Chain Management | Small chains under 10 locations | $299 | Lowest entry cost | Only supports 10 locations without extra fees |

Implementation: What to Expect
Deploying a new system isn’t quick. On average, it takes 8-12 weeks for a chain with 5-10 locations. Staff need 16 hours of training for technicians and 24 hours for pharmacists. Chains that use vendor-certified trainers see 12% higher adoption rates than those training internally. One major hurdle? Data migration. 27% of chains had prescription history errors during the switch. That means manually checking 14.7% of patient records to make sure nothing was lost. To avoid this, choose a vendor that offers full data cleanup as part of the onboarding. The best model is the “hub-and-spoke” approach: one central hub manages drug pricing, inventory, and compliance, while each local pharmacy keeps full control over clinical decisions. A University of California study found this method reduced medication errors by 38% compared to fully centralized clinical models.The Future Is Here-And It’s Mandatory
Regulators aren’t waiting. CMS now requires multi-location pharmacies to prove they track prescription errors across all locations to qualify for Medicare Part D. That’s why adoption jumped 44% since 2021. By 2025, all pharmacy systems must comply with FHIR API standards-something 63% of current systems can’t do without $200,000+ in upgrades. And by 2027, the Pharmacy Quality Alliance predicts centralized systems will be mandatory for any chain with three or more locations. Even newer tech is emerging. Blockchain-based verification, tested by Outcomes.com, cut prescription fraud by 67% in trials. AI tools now predict which seniors are at risk of overmedication before it happens.What You Should Do Today
If you manage multiple pharmacies or work with seniors on multiple prescriptions:- Identify how many pharmacies your patients use. If it’s more than one, you’re at risk.
- Check if each pharmacy shares medication records. If not, push for a centralized system.
- Ask prescribers to use e-prescribing platforms that integrate with your pharmacy software.
- Choose a system with Watchdog or AI monitoring features-they catch errors humans miss.
- Train staff to always verify transfers. No matter how good the system is, human checks still save lives.
Managing multiple pharmacies and prescribers safely isn’t about technology-it’s about respect. It’s about making sure an 82-year-old doesn’t get two blood thinners because two different doctors didn’t know what the other prescribed. It’s about giving families peace of mind. The tools exist. The data proves they work. The only question left is: are you ready to use them?
Can a senior use two different pharmacies safely without a centralized system?
It’s risky. Without a unified system, pharmacies can’t see what’s been filled elsewhere. This leads to dangerous duplicates, missed interactions, and delayed refills. Seniors on five or more medications are especially vulnerable. A centralized system is the only reliable way to prevent errors.
Do all pharmacies in a chain need to use the same software?
Yes. If even one pharmacy uses a different system, data won’t sync properly. This creates blind spots. For example, a patient’s allergy might be recorded in one system but not in another, leading to a life-threatening error. All locations must use the same centralized platform.
How long does it take to switch to a new pharmacy management system?
Typically 8-12 weeks for chains with 5-10 locations. The timeline includes data migration, staff training, system testing, and go-live support. Chains with more than 15 locations may need 14-18 weeks. Rushing the process increases the risk of prescription errors during transition.
Is cloud-based better than on-site software for multi-pharmacy chains?
Yes. Cloud-based systems offer 99.99% uptime, automatic updates, and real-time access from any location. On-site systems require manual updates, have higher downtime risks, and can’t easily support remote access for pharmacists working across multiple sites. All top vendors now offer cloud-only solutions.
What’s the biggest mistake pharmacies make when adopting a new system?
Trying to do everything at once. The most successful chains start with one feature: universal drug files. Then they add real-time patient profiles. Then automated transfers. Trying to migrate all data, train everyone, and switch prescriber communication overnight leads to errors and staff burnout. Take it step by step.
Can a centralized system help with Medicare Part D compliance?
Absolutely. CMS now requires multi-location pharmacies to demonstrate cross-location tracking of prescription errors and duplicate therapies. Only centralized systems can provide the audit trails and real-time reporting needed to meet these standards. Chains without them risk losing Medicare contracts.
Are there affordable options for small pharmacy chains?
Yes. PharmacyOne Chain Management starts at $299 per location monthly and supports up to 10 pharmacies. Datarithm is another budget-friendly option focused on inventory and error reduction. But avoid systems that limit connections or charge extra for each additional location-those aren’t built for true multi-site management.
How do these systems handle prescriber changes?
Modern systems automatically flag new prescribers and cross-check their prescribing patterns against the patient’s history. If a new doctor prescribes a drug already being taken, the system alerts the pharmacist. Some, like EnterpriseRx, even allow direct messaging to prescribers through integrated EHRs, reducing delays and misunderstandings.