Every time you pick up a prescription for a generic drug, you’re holding a product that’s been engineered to match a brand-name medicine down to the last molecule - but at a fraction of the cost. While many assume generic drugs are just cheaper copies, the truth is far more precise. The manufacturing process for generic drugs is tightly regulated, scientifically rigorous, and surprisingly complex. It’s not about cutting corners. It’s about meeting the same exact standards as the original - without repeating the same expensive clinical trials.
What Makes a Drug "Generic"?
A generic drug isn’t just a lookalike. It must contain the same active ingredient, in the same strength, same dosage form (tablet, capsule, injection, etc.), and same route of administration as the brand-name version. The U.S. Food and Drug Administration (FDA) requires that it works the same way in the body. That means if you take a generic version of lisinopril for high blood pressure, it must deliver the same amount of medicine into your bloodstream at the same rate as the brand-name version, Prinivil or Zestril. The key word here is bioequivalence. This isn’t marketing jargon. It’s a scientific requirement. To prove it, manufacturers run studies with 24 to 36 healthy volunteers. They measure how quickly and how much of the drug enters the bloodstream - tracked using two numbers: Cmax (peak concentration) and AUC (total exposure over time). For a generic to be approved, these values must fall within 80% to 125% of the brand-name drug’s results, with 90% confidence. That’s a tight window. It’s not guesswork. It’s data-driven science.The ANDA Pathway: Skipping the Clinical Trials
You might wonder: if generic drugs are just copies, why do they still take years to get approved? The answer lies in the Abbreviated New Drug Application (ANDA). Created by the 1984 Hatch-Waxman Act, this pathway lets generic makers rely on the brand-name drug’s existing safety and efficacy data. They don’t have to repeat animal studies or large-scale human trials proving the drug works. That cuts the development time from 10-15 years to just 3-4 years, and the cost from over $2 billion to $5-10 million per product. But here’s what people don’t realize: the ANDA isn’t short on paperwork. In fact, it’s often thicker than a novel. A typical submission runs between 5,000 and 10,000 pages. It includes hundreds of analytical methods, dozens of batch records, stability data from 12+ months of real-time testing, and full reports from bioequivalence studies. The FDA reviews every single page. On average, it takes them 17 months - though complex generics can take up to three years.Step-by-Step: How Generic Drugs Are Actually Made
The manufacturing process doesn’t start with a machine. It starts with a deep dive into the brand-name drug. Manufacturers don’t just buy the active ingredient and start pressing pills. They reverse-engineer the original product to understand every detail.- Reference Drug Analysis - The first step is studying the brand-name drug’s composition. This includes identifying the active pharmaceutical ingredient (API), all inactive ingredients (excipients), and how they’re structured. Even the shape, size, and coating of the tablet matter.
- Formulation Development - Using the Quality by Design (QbD) framework, manufacturers identify Critical Quality Attributes (CQAs) - like how fast the drug dissolves or how stable it is over time. Then they figure out which raw materials and manufacturing steps affect those attributes. A change in lactose particle size? That can alter tablet hardness and how quickly the drug releases. One small tweak can ruin the whole batch.
- Mixing and Granulation - The API and excipients are blended in precise ratios. If the mixture isn’t uniform, some pills get too much drug, others too little. Granulation turns the powder into small, consistent granules so they compress evenly later.
- Drying - Moisture is the enemy of drug stability. Granules are dried under strict temperature and humidity controls. Too much moisture? The tablet can degrade. Too little? It crumbles.
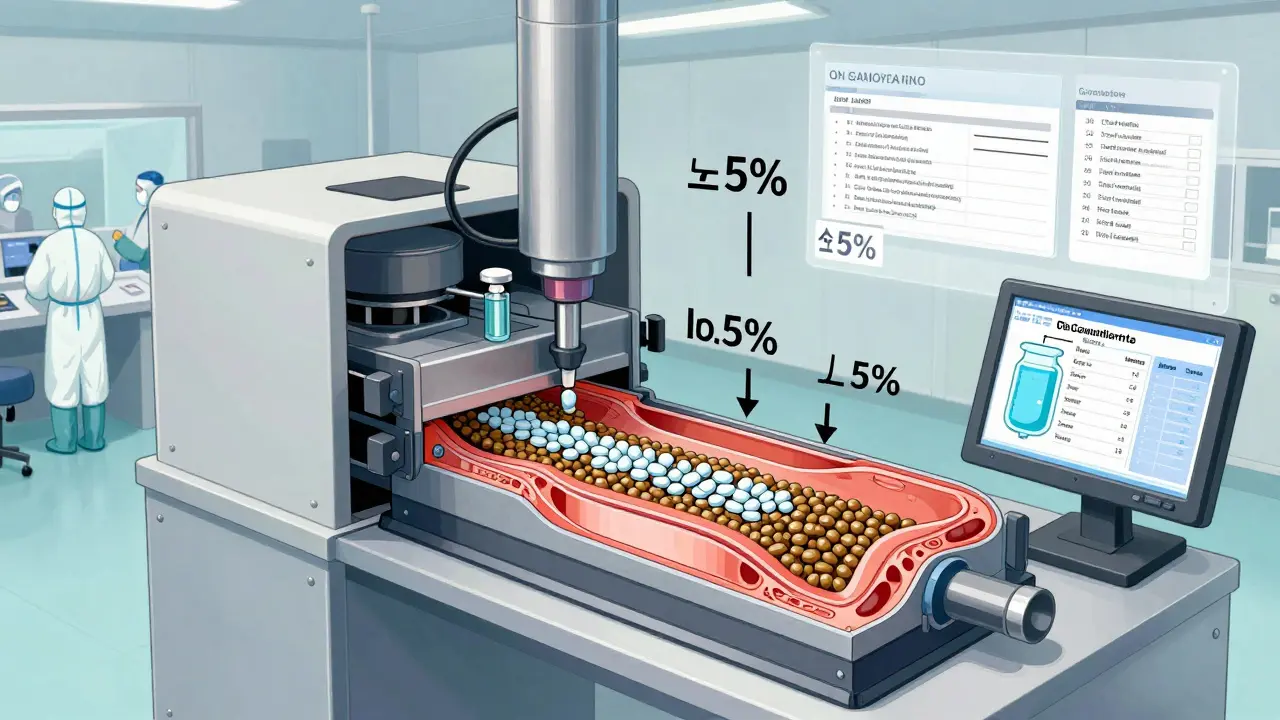
- Compression and Encapsulation - Dry granules are pressed into tablets using high-speed machines. Capsules are filled with powder or pellets. Each tablet must weigh within ±5% for pills under 130mg, or ±7.5% for pills between 130-324mg. The FDA checks this constantly.
- Coating - Tablets get a coating for multiple reasons: to mask bitter taste, protect the drug from stomach acid, or control how fast it releases. A delayed-release pill for arthritis, for example, needs to dissolve only in the intestines - not the stomach. Getting that right requires exact polymer thickness and composition.
- Quality Control - Every batch is tested. Not just once - multiple times. They check for identity (is it the right drug?), strength (is there enough?), purity (are there contaminants?), and dissolution (does it release properly?). Dissolution testing alone can involve dozens of samples tested over hours under simulated stomach and intestinal conditions.
- Packaging and Labeling - The final product is packaged in blister packs, bottles, or vials. Labels must match the brand-name drug exactly - same warnings, same instructions. But here’s a twist: by law, generics can’t look identical to the brand-name version. Color, shape, and markings must differ to avoid trademark infringement. That’s why your generic lisinopril might be blue and oval, while the brand is white and round.
Where It’s Made: Cleanrooms, Regulations, and Compliance
You won’t find generic drugs being made in basements or garages. Every facility must meet Current Good Manufacturing Practices (CGMP). That means cleanrooms with controlled air quality (ISO Class 5-8), temperature between 20-25°C, and humidity at 45-65% RH. Workers wear full protective gear. Equipment is cleaned and validated. Every step is documented. The FDA inspects these facilities regularly. In 2023, the most common violations found were: inadequate investigation of out-of-spec results (37% of warning letters), poor process validation (29%), and weak quality unit oversight (24%). One bad batch can lead to a recall - like the 2021 Teva recall of 14 generic products due to CGMP failures at their Puerto Rico plant. Leading manufacturers invest heavily in training. Companies like Dr. Reddy’s require 160 hours of initial GMP training and 40 hours annually. Why? Because a single error in documentation or measurement can delay approval for months - or worse, put patients at risk.Complex Generics: The New Frontier
Not all generics are created equal. Simple pills - like metformin or atorvastatin - are easy to copy. But complex products? That’s where the real challenge begins. Topical creams, inhalers, nasal sprays, and extended-release tablets are harder to replicate because their performance depends on more than just chemistry. For example, a generic version of Clobetasol Propionate cream took seven years and $47 million to develop because skin absorption had to match the original exactly. Traditional bioequivalence tests didn’t cut it. Manufacturers had to invent new testing methods. That’s why the FDA launched its Complex Generic Products Initiative in 2022. As of December 2023, they’ve published 127 product-specific guidances to help manufacturers navigate these challenges. Today, 35% of pending ANDAs are for complex generics - up from just 12% in 2015.Why Generics Save Billions - and What Keeps Them Affordable
In the U.S., 90% of prescriptions are filled with generics. That’s not coincidence. It’s by design. Over the past decade, generics have saved the healthcare system over $1.7 trillion. A single course of Sovaldi (sofosbuvir) for hepatitis C cost $84,000 as a brand drug. The generic version? $28,000. That’s a 67% drop - and millions of patients got treated because of it. But price pressure is real. For simple generics, 15-20 manufacturers often compete, driving prices down 70-80% within two years. That’s why many companies now focus on complex generics, where only 2-5 competitors exist, and prices drop slower - around 20-30% over five years. There’s also a growing trend: authorized generics. These are brand-name companies selling their own drug under a generic label, often right after patent expiration. In 2023, they captured 23% of first-generic market share. It’s a smart business move - they keep profits while undercutting competitors.
Are Generic Drugs Safe? The Evidence
Concerns about quality variations in generics are real - but often overstated. A 2022 study in JAMA Internal Medicine raised flags about narrow therapeutic index drugs (like warfarin or levothyroxine), where small differences in absorption could matter. But here’s what the data shows: a 2023 survey by the Association for Accessible Medicines found that 89% of pharmacists reported no meaningful clinical differences between generics and brands. Only 3% saw any real impact. The FDA’s system is designed to catch inconsistencies. Every batch is tested. Every facility is inspected. Every bioequivalence study is scrutinized. When a problem arises - like the 2021 Teva recall - it’s made public. That’s accountability. The real issue isn’t quality. It’s concentration. Nearly 78% of the active ingredients in U.S. generic drugs come from just two countries: China and India. That creates supply chain risks. But it also keeps prices low. The trade-off is real - but so far, the system has held.What’s Next for Generic Drug Manufacturing?
The future is faster, smarter, and more automated. The FDA’s Emerging Technology Program has approved 17 continuous manufacturing facilities for generics. Instead of making drugs in batches over weeks, these systems run nonstop - producing pills in hours. Vertex’s cystic fibrosis drug, made this way, achieved 99.98% batch acceptance - far higher than the 95% from traditional methods. AI is also entering the picture. Pfizer’s pilot program used machine learning to detect tablet defects during visual inspection. It cut errors by 40%. Digital twins - virtual models of manufacturing lines - are being tested to predict problems before they happen. GDUFA IV, renewed in October 2022, now requires the FDA to review 90% of ANDAs within 10 months - down from 17. That’s progress. More approvals mean more competition. More competition means lower prices. And more patients get the medicine they need.Final Thoughts: More Than Just a Cheaper Pill
Generic drugs aren’t a compromise. They’re a triumph of science, regulation, and public policy. Behind every small, unbranded tablet is a team of scientists, engineers, and regulators working to ensure it’s as safe and effective as the original - while making it affordable for millions. The process is long, detailed, and unforgiving. One wrong excipient. One failed dissolution test. One inspection violation. And the whole batch is thrown out. That’s the cost of trust. If you’ve ever wondered why your generic medication works just as well as the brand - now you know. It’s not luck. It’s precision.Are generic drugs as effective as brand-name drugs?
Yes. The FDA requires generic drugs to have the same active ingredient, strength, dosage form, and route of administration as the brand-name version. They must also prove bioequivalence - meaning they deliver the same amount of medicine into your bloodstream at the same rate. Studies show no meaningful difference in clinical outcomes for the vast majority of patients.
Why are generic drugs cheaper?
Generic manufacturers don’t have to repeat expensive clinical trials to prove safety and effectiveness. They rely on the brand-name drug’s existing data through the Abbreviated New Drug Application (ANDA) pathway. This cuts development costs from over $2 billion to $5-10 million. Plus, competition among multiple generic makers drives prices down further.
Can generic drugs have different side effects?
The active ingredient is identical, so the core side effects are the same. But generics can use different inactive ingredients (like dyes or fillers), which may cause rare allergic reactions in sensitive individuals. For example, someone allergic to a dye in one brand might react to that same dye in a specific generic version. That’s why pharmacists check for known allergens when substituting.
How long does it take to make a generic drug?
The entire process - from reverse-engineering the brand drug to FDA approval - typically takes 3 to 4 years. Simple generics can be approved faster, while complex ones (like inhalers or extended-release tablets) may take 5-7 years. The FDA’s review time averages 17 months, but can stretch to 36 months for difficult cases.
Are all generic drugs made in the U.S.?
No. Nearly 78% of the active ingredients in U.S. generic drugs come from China and India. Final packaging often happens in the U.S. or Europe, but the raw materials and bulk manufacturing are global. All facilities - no matter where they’re located - must meet U.S. FDA standards and are subject to inspection.
What’s the difference between a generic and an authorized generic?
An authorized generic is made by the original brand-name company but sold under a generic label, usually right after the patent expires. It’s chemically identical to the brand drug - same manufacturer, same facility, same formula. The only difference is the label. Authorized generics often capture a large share of the first-generic market because they eliminate uncertainty for patients and pharmacists.
Why do generic pills look different from brand-name pills?
U.S. trademark law prohibits generic drugs from looking identical to brand-name versions. So even if the active ingredient is the same, generics must differ in color, shape, size, or markings. This prevents confusion and protects the brand’s intellectual property. But the medicine inside works the same way.
Can I trust generic drugs from other countries?
Yes - if they’re sold in the U.S. All generic drugs sold here, regardless of where they’re made, must meet FDA standards. The FDA inspects foreign manufacturing facilities just like domestic ones. If a facility fails inspection, the FDA blocks imports. You can trust U.S.-marketed generics because they’re held to the same rigorous standards as brand-name drugs.


Gray Dedoiko
December 22, 2025 AT 17:44Man, I never realized how much science goes into these little pills. I always thought generics were just cheap knockoffs, but this breakdown makes it clear they’re just as precise. The bioequivalence stuff? Wild that they test it on humans with such tight margins. Feels good knowing my blood pressure med isn’t a gamble.
Thanks for laying this out so clearly.
Aurora Daisy
December 24, 2025 AT 01:15Oh great, another American propaganda piece. So now we’re supposed to believe the FDA is some infallible guardian of health? Meanwhile, 78% of the active ingredients come from China and India - places with zero transparency. You think they’re testing every batch? Please. They’re printing labels and calling it a day.
bharath vinay
December 24, 2025 AT 18:05They’re lying. The FDA doesn’t inspect every facility. The real manufacturers are bribing inspectors. Look at the Teva recall - that was just the tip. The entire system is rigged to keep Big Pharma in control. Generics aren’t cheaper because of competition - they’re cheaper because the ingredients are cut with talc and chalk. You think your diabetes med is safe? It’s not. It’s poison with a label.
Wilton Holliday
December 25, 2025 AT 14:41This is actually one of the most reassuring things I’ve read in a long time. I used to be scared to switch to generics, but now I get it - it’s not about cutting corners, it’s about smart science. The QbD framework alone is genius. And the fact that they test dissolution under simulated stomach conditions? That’s next-level detail.
Props to everyone who works in this space. You’re the real MVPs of healthcare.
:)
Raja P
December 26, 2025 AT 10:56Interesting read. I’ve been on generic metformin for years and never had an issue. Still, I get why people worry - especially with the supply chain stuff. Maybe we need more domestic production? Not to be nationalist, but it’d help with reliability.
Either way, glad someone took the time to explain this properly.
Payson Mattes
December 27, 2025 AT 07:43Wait, so you’re telling me the FDA approves drugs based on 24 volunteers? That’s it? No wonder so many people get sick. I know a guy whose cousin took a generic version of Xanax and ended up in the ER. They didn’t even test it on people with anxiety disorders. This whole system is a scam. And don’t even get me started on how they’re hiding the real manufacturers behind shell companies. The government’s in on it. I’ve got the documents.
Just sayin’.
Isaac Bonillo Alcaina
December 28, 2025 AT 11:52Your article contains multiple grammatical errors. For instance, 'It’s not about cutting corners. It’s about meeting the same exact standards as the original' - redundant use of 'same' and 'exact.' Also, 'bioequivalence' is misspelled as 'bioequivalance' in the third paragraph. And you used 'they' as a singular pronoun in 'they measure how quickly...' - improper syntax. This undermines your credibility. Precision matters - especially when discussing pharmaceuticals.
siddharth tiwari
December 30, 2025 AT 04:28they say its the same but everyone knows its not. i took a generic for my thyroid and i felt like a zombie for 2 weeks. the brand worked fine. they dont test on real people with real conditions. just young healthy kids. and the factory in india? they dont even wash their hands. i seen the videos. the FDA is bought. i dont trust any of it.
suhani mathur
December 30, 2025 AT 21:08Oh wow, so the FDA reviews 10,000 pages of paperwork? And you think that’s enough? Sweetheart, if I had to read that much of my ex’s apology text, I’d need a therapist. But hey - at least the pills aren’t purple. Because, you know, trademark law.
Still, I’m impressed. Someone actually did their homework. Most people think ‘generic’ = ‘I hope this doesn’t kill me.’ You just gave them a reason to trust it.
Diana Alime
January 1, 2026 AT 17:51I JUST SWITCHED TO GENERIC LIPITOR AND NOW I CAN’T GET OUT OF BED. MY LEGS ARE WEAK. MY BRAIN IS MUSH. I THOUGHT THIS WAS SUPPOSED TO BE THE SAME?!?!? THIS IS A SCAM. I’M SENDING A LETTER TO CONGRESS. I’M TELLING MY FACEBOOK GROUP. I’M TELLING MY DOG. MY DOG IS NOW WORRIED. I NEED A REFUND. AND A THERAPIST. AND A NEW LIFE.
Adarsh Dubey
January 2, 2026 AT 10:23It’s fascinating how much engineering goes into something so small. I never thought about coating thickness or granule size affecting absorption. Makes you appreciate the quiet work behind everyday medicine. Also, the part about authorized generics? That’s actually kind of brilliant - same pill, different label. No wonder they dominate the first wave.
Bartholomew Henry Allen
January 3, 2026 AT 19:43USA leads in generic drug safety and innovation. No other country has the discipline or standards. China and India produce the raw materials but only the USA ensures quality. This system works. Trust the process. The FDA is not perfect but it is the best. No exceptions.
Chris Buchanan
January 5, 2026 AT 15:02Okay, but let’s be real - if a generic pill costs $4 and the brand costs $400, and they’re ‘the same’… why does the brand still exist? Because people are scared. Because they think ‘expensive = better.’ That’s not science, that’s psychology. And the system is banking on it.
But hey - I’m switching to generic. My wallet thanks you.
Delilah Rose
January 5, 2026 AT 20:18It’s wild to think about how many variables are in play here - from the particle size of lactose to the humidity in the drying room to the exact polymer blend used in the coating. One tiny change and suddenly the drug doesn’t dissolve properly, or it degrades too fast, or the tablet cracks in transit. And then you’ve got regulators going through 10,000 pages of documentation, checking every batch, inspecting factories halfway across the world, all to make sure that little white pill you pick up at CVS does exactly what it’s supposed to do - and nothing more. It’s like a symphony of precision, and most people just swallow it without thinking. I’m genuinely in awe of how much effort goes into something so invisible in our daily lives. We take it for granted, but this is one of the most sophisticated public health systems ever built. And it’s working. Mostly.
Bret Freeman
January 7, 2026 AT 13:20They say generics are safe. But what about the ones that don’t get recalled? The ones that slip through? The ones that make people feel weird but not sick enough to go to the hospital? You think they track that? Nah. They just count the number of approvals and call it a win. Meanwhile, grandma’s on five different generics and she’s been crying for three weeks because she can’t remember her own name. But hey - at least it’s cheap. And that’s what matters, right? The bottom line. Always the bottom line.