Fiber for Functional Dyspepsia Calculator
Recommended Fiber Plan
Enter your details and click "Calculate Recommended Fiber Intake" to see your personalized plan.
Soluble Fiber Benefits
Forms a gel that soothes the stomach lining and slows gastric emptying, helping manage early satiety and pain.
Insoluble Fiber Benefits
Adds bulk to stool and speeds up transit, reducing bloating and promoting regular bowel movements.
Quick Take
- Fiber speeds up gastric emptying and eases bloating.
- Soluble fiber forms a gel that soothes the stomach lining.
- Insoluble fiber adds bulk, promoting regular bowel movements.
- Combining fiber with low‑FODMAP foods reduces symptom flare‑ups.
- Start with 5‑10g/day and increase gradually to avoid gas.
Living with functional dyspepsia is a daily struggle for many. The condition shows up as upper‑abdominal pain, early satiety, and a burning sensation, yet standard medications often fall short. One low‑cost, side‑effect‑free ally is fiber, the indigestible carbohydrate that lives in fruits, veggies, whole grains, and legumes. Below we unpack how different fiber types interact with the gut, why they matter for functional dyspepsia, and how to add them safely.
What Is Functional Dyspepsia?
Functional dyspepsia is a chronic disorder of the upper gastrointestinal tract with no obvious structural cause. The Rome IV criteria define it by at least one of these symptoms for three months: post‑prandial fullness, early satiety, epigastric pain, or burning. Studies from 2023‑2024 show a prevalence of 10‑15 % in the adult population, making it one of the most common functional GI disorders.
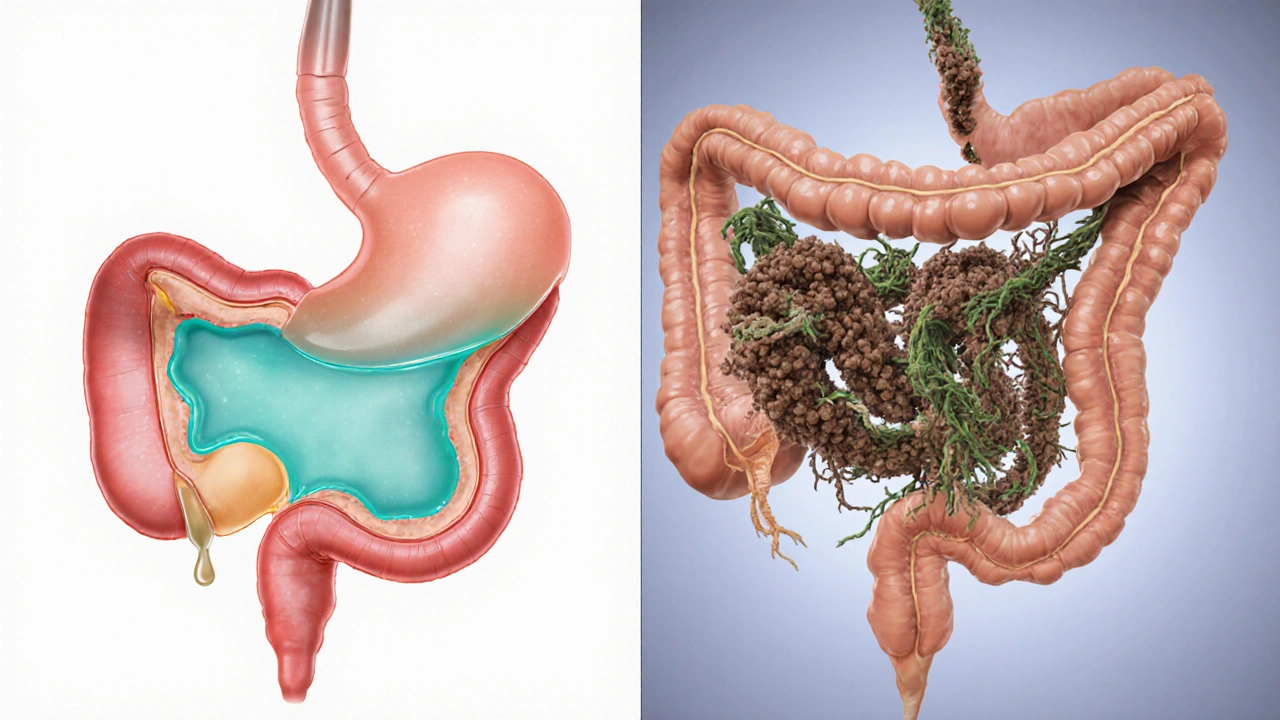
Why Fiber Matters for the Stomach
Fiber works on two fronts: mechanical and biochemical. Mechanically, bulk‑forming fiber (insoluble) speeds up transit, preventing food from sitting too long in the stomach. Biochemically, gel‑forming fiber (soluble) traps water and creates a protective mucous layer, reducing irritation.
Research published in the Journal of Gastroenterology (2024) found that participants who added 12g of soluble fiber daily reported a 30 % drop in dyspeptic pain scores compared with a placebo group. The same study linked higher short‑chain fatty acid (SCFA) production to improved gastric motility, highlighting the gut‑microbiota connection.
Soluble vs. Insoluble Fiber: A Side‑by‑Side Look
| Attribute | Soluble Fiber | Insoluble Fiber |
|---|---|---|
| Primary Sources | Oats, barley, legumes, apples, psyllium | Whole wheat, bran, nuts, seeds, vegetable skins |
| Viscosity | High - forms gel | Low - retains shape |
| Effect on Gastric Emptying | Slows, allowing smoother digestion | Accelerates transit, reducing stasis |
| Impact on Gut Microbiota | Feeds beneficial bacteria → more SCFAs | Less fermentable, mainly adds bulk |
| Typical Daily Intake (g) | 5‑10 | 10‑15 |
How Fiber Improves Specific Dyspeptic Symptoms
- Early Satiety: Soluble fiber’s gel slows the rate at which the stomach empties, giving the brain more accurate signals about fullness.
- Bloating & Gas: Insoluble fiber’s bulk prevents food from fermenting excessively, while a gradual increase limits gas production.
- Epigastric Pain: A thicker mucous layer from soluble fiber buffers acid, lessening irritation.
- Nausea: Faster gastric emptying with insoluble fiber reduces the time irritants sit in the stomach.
Putting Fiber Into Your Daily Routine
Start low, go slow. Jumping from 0 to 30g can trigger cramping. Here’s a 7‑day ramp‑up plan that balances soluble and insoluble sources.
- Day1‑2: Add 5g of psyllium husk (soluble) to a smoothie.
- Day3‑4: Include a small apple and a handful of almonds (insoluble).
- Day5‑6: Swap white rice for brown rice; add a spoonful of oat bran.
- Day7: Aim for 15g total (mix oats, beans, and veggies).
Drink at least eight glasses of water daily; fiber needs fluid to move smoothly through the tract.
Combining Fiber With Other Gut‑Friendly Strategies
Fiber works best as part of a broader plan:
- Low‑FODMAP diet: Reduces fermentable carbs that can aggravate dyspepsia. Pair with fiber to keep stool regularity.
- Probiotics: Strains like Lactobacillus plantarum boost SCFA production, complementing soluble fiber.
- Prebiotic foods: Garlic, onions, and chicory root feed beneficial bacteria, enhancing the fiber effect.
- Mindful eating: Chew slowly, avoid large meals, and limit caffeine and alcohol, which can worsen gastric sensitivity.
Potential Pitfalls and How to Avoid Them
Even a good thing can go wrong if misused:
- Over‑fibering: More than 40g/day can cause constipation or diarrhea. Stay within 25‑30g for most adults.
- Skipping fluids: Without water, insoluble fiber can harden stools.
- Ignoring underlying conditions: If symptoms persist despite dietary changes, rule out peptic ulcer disease, gallbladder issues, or medication side effects.
- Allergic reactions: Some people react to oats or wheat bran; switch to gluten‑free or hypoallergenic sources.
When to Seek Professional Help
If you notice any of the following, schedule a gastroenterology appointment:
- Weight loss >5% over a month
- Vomiting blood or black stools
- Severe, unrelenting pain
- No improvement after 8weeks of dietary tweaks
Doctors may recommend endoscopy, H‑pylori testing, or pro‑kinetic medications. Fiber can still be integrated, but under guidance.
Summary Checklist for Managing Functional Dyspepsia With Fiber
- Identify your baseline fiber intake (use a food diary).
- Start with 5g soluble fiber; increase by 5g every 2‑3days.
- Mix soluble (oats, psyllium) and insoluble (bran, nuts) sources.
- Drink 2‑3L of water daily.
- Combine with low‑FODMAP foods, probiotics, and mindful eating.
- Track symptoms; adjust if bloating or gas spikes.
- Consult a clinician if red‑flag symptoms appear.
Frequently Asked Questions
Can I treat functional dyspepsia with fiber alone?
Fiber can markedly lessen mild‑to‑moderate symptoms, but it isn’t a cure‑all. Most patients benefit from a combined approach that includes diet adjustments, stress management, and sometimes medication.
How much fiber should I aim for each day?
The general target is 25g for women and 38g for men, but when managing functional dyspepsia start at 5‑10g of soluble fiber and gradually work up to 20‑30g total, split between soluble and insoluble types.
Is psyllium safe for everyone?
Psyllium is widely tolerated, but people with bowel obstruction, severe constipation, or swallowing difficulties should avoid it unless a doctor approves.
Will a high‑fiber diet cause more gas?
A sudden surge in fiber can increase gas, especially from fermentable soluble fiber. Introducing fiber slowly and staying hydrated keeps the gas buildup in check.
Should I avoid gluten if I have functional dyspepsia?
Only if you have a confirmed gluten sensitivity or celiac disease. Otherwise, whole‑grain gluten‑containing foods provide valuable insoluble fiber and can be part of the plan.


kat gee
October 3, 2025 AT 16:00Wow, because a bit of bran is totally the miracle cure-who needs meds, right?
Iain Clarke
October 3, 2025 AT 18:46Adding fiber works best when you also keep your diet low in FODMAPs to limit excess fermentation.
Remember to increase water intake gradually, at least two to three litres a day.
This balanced approach helps avoid the bloating some people report.
Courtney Payton
October 3, 2025 AT 21:33It'se not just about eating more carbs; we have a moral duty to question quick‑fix trends.
People often ignore the deeper causes of dyspepsia, preferring a sprinkle of oats over real self‑care.
Muthukumaran Ramalingam
October 4, 2025 AT 01:43I get why people love the idea of a fiber fix, but the reality is messier than a quick blog post suggests.
First, not all fiber is created equal; soluble and insoluble act in opposite ways, and you can’t just dump a handful of bran and expect miracles.
Second, the gut microbiome reacts differently to each source, so a one‑size‑fits‑all recommendation ignores individual variability.
Third, many studies cited are short‑term and involve small sample sizes, which limits how much we can trust the numbers.
Fourth, the calculator on this page assumes you’ll increase intake by exactly five grams a week, but most people experience bloating long before that threshold.
Fifth, the advice to drink eight glasses of water sounds generic, yet many patients already struggle with fluid retention or kidney issues.
Sixth, the suggestion to pair fiber with low‑FODMAP foods is sound, but the low‑FODMAP list itself eliminates many fiber‑rich fruits and vegetables, creating a paradox.
Seventh, the claim that soluble fiber forms a protective gel is partially true, but excess gel can slow gastric emptying too much, worsening early satiety.
Eighth, insoluble fiber’s bulk can aggravate intestinal hypersensitivity in some dyspepsia subtypes, leading to more pain rather than relief.
Ninth, the article never mentions potential interactions with common medications like antacids or PPIs, which can alter fiber efficacy.
Tenth, you’ll find that stumbling over the recommended 12‑gram soluble boost may trigger gas that mimics the very symptoms you’re trying to fix.
Eleventh, adherence rates drop dramatically when patients are asked to track grams every day instead of listening to hunger cues.
Twelfth, cost can be a hidden barrier; high‑quality psyllium or oat bran isn’t cheap for a low‑income household.
Thirteenth, the psychological aspect of chronic dyspepsia is ignored; stress management often outperforms any dietary tweak.
Finally, before overhauling your diet, a proper medical work‑up is essential to rule out ulcers, gallbladder disease, or Celiac, because fiber won’t heal those.
Garrett Williams
October 4, 2025 AT 03:06Keep it steady and you’ll feel better each day!
joba alex
October 4, 2025 AT 04:30Honestly, the whole fiber hype is just another marketing gimmick; the bioavailability metrics are over‑engineered and the recommended grams are arbitrarily set based on outdated RDA models.
Using terms like 'soluble gel matrix' sounds scientific but it masks the fact that many of these compounds have negligible effect on gastric motility when consumed in isolation.
Rene Lacey
October 4, 2025 AT 05:53When we contemplate the act of eating, we are not merely ingesting calories but engaging in a ritual that shapes our very perception of self.
Fiber, in this philosophical sense, can be seen as a conduit between the material and the ethereal, grounding us while simultaneously inviting contemplation of the unseen microbial allies within.
Thus, the recommendation to integrate soluble and insoluble sources is not just a medical directive but an invitation to participate in a larger ecological narrative.
OKORIE JOSEPH
October 4, 2025 AT 08:40Stop reading nonsense and just try a real diet plan without all that fluff
Lucy Pittendreigh
October 4, 2025 AT 11:26This pseudo‑science is dangerous and trivializes real health struggles
Nikita Warner
October 4, 2025 AT 14:13For a comprehensive approach, consider scheduling a consultation with a gastroenterologist to rule out structural causes.
In parallel, a gradual increase in dietary fiber-targeting 20‑30 g per day split between soluble and insoluble sources-combined with adequate hydration can be beneficial.
Monitoring symptom patterns in a diary will help identify which foods provide the most relief.