Many people think herbal supplements are safe because they’re natural. But that’s not always true-especially when you’re taking prescription drugs. What you might see as a harmless daily pill for energy, mood, or heart health could be quietly messing with your medication, sometimes with serious consequences.
Why Herbal Supplements and Prescription Drugs Don’t Always Mix
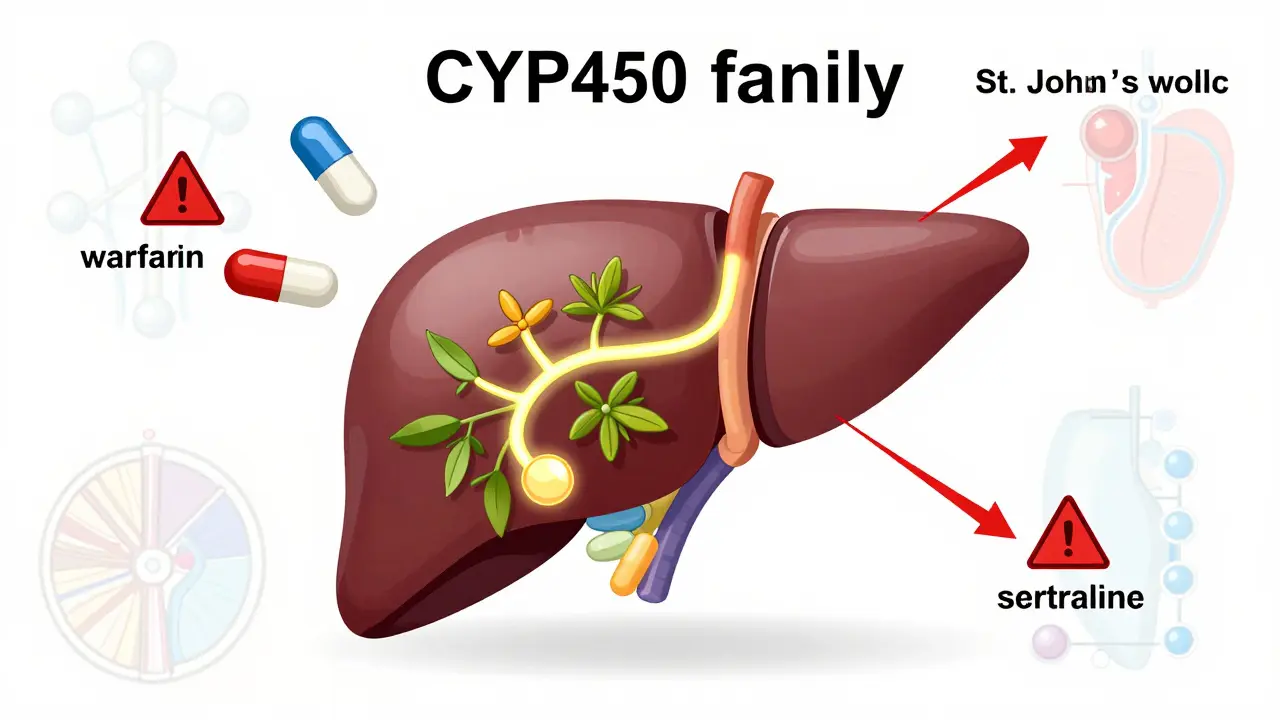
Herbal supplements don’t go through the same testing as prescription drugs. They’re not required to prove safety or effectiveness before hitting store shelves. That means you might be taking something that changes how your body processes your blood pressure medicine, antidepressant, or blood thinner-without knowing it. The body breaks down drugs using enzymes in the liver, mostly from the CYP450 family. Some herbs block these enzymes. Others speed them up. Either way, your drug’s levels in the blood can swing too high or too low. Too high? Risk of overdose. Too low? The drug stops working. A 2022 Mayo Clinic study found nearly 70% of adults over 65 take at least one herbal supplement. And only about 25% tell their doctor. That’s a dangerous gap. You might think, ‘It’s just garlic pills,’ but garlic can thin your blood just like aspirin. Combine it with warfarin? You’re playing Russian roulette with bleeding.High-Risk Herbal Supplements and the Drugs They Interact With
Some herbs have well-documented, life-altering interactions. Here are the top ones you need to know about.- St. John’s Wort - This popular mood booster cuts the effectiveness of over 60 medications. It can drop blood levels of antidepressants like sertraline by 20-40%, making them useless. It also reduces birth control effectiveness by 15-30%, leading to unplanned pregnancies. For people on HIV meds like saquinavir, levels can drop by 80%. One study showed 78% of users on Drugs.com reported contraceptive failure.
- Ginkgo biloba - Often used for memory, it interferes with blood clotting. When taken with warfarin, clopidogrel, or apixaban, it increases bleeding risk by 300%. Between 2010 and 2020, Mayo Clinic recorded 23 major bleeding cases-including 3 deaths-linked to this combo. One Reddit user shared his INR spiked to 8.2 after mixing ginkgo with apixaban, leading to severe rectal bleeding.
- Garlic supplements - More than just a flavoring, garlic acts like a natural blood thinner. A 2019 University of Washington trial showed it cuts saquinavir levels by 51%. It also increases bleeding risk when taken with blood thinners. Even though garlic is in many ‘immune support’ products, most people don’t realize they’re taking a dose strong enough to matter.
- Goldenseal - This herb blocks CYP3A4, the same enzyme that processes 50% of all prescription drugs. It can reduce clearance of midazolam (a sedative) by 40%. That means you could end up overdosed on painkillers, statins, or even some cancer drugs without knowing why.
- Coenzyme Q10 - Often taken with statins to reduce muscle pain, it may weaken warfarin’s effect by 25-30%. That means your INR could drop, increasing clot risk. Weekly INR checks are needed if you’re taking both.
- Ginseng - Can interfere with monoamine oxidase inhibitors (MAOIs), leading to serotonin syndrome-a dangerous spike in body temperature, confusion, and muscle rigidity. It may also lower blood pressure too much when taken with calcium channel blockers.
- Hawthorn - Used for heart health, it can cause dangerously low blood pressure when mixed with beta-blockers or ACE inhibitors. One patient’s systolic pressure dropped to 84 mmHg after combining hawthorn with metoprolol.
- Licorice - Found in many teas and throat lozenges, it causes potassium loss. When taken with diuretics like furosemide, it can lead to muscle weakness, irregular heartbeat, or even cardiac arrest.
What About the ‘Safe’ Herbs?
Not all herbs are high-risk. Some, like milk thistle, saw palmetto, and black cohosh, have minimal documented interactions. But ‘minimal’ doesn’t mean ‘none.’ Cranberry juice is a good example. Many assume it’s safe with warfarin. But while some studies show no effect, others-like a 2020 JAMA meta-analysis-found INR levels rose by up to 1.8 units in some people. The difference? Dose, frequency, and individual metabolism. One person sipping a glass a day might be fine. Another drinking 250 mL daily could end up in the ER. The same goes for green tea. New data from NCCIH’s January 2024 update shows it reduces the effectiveness of bortezomib, a drug used for multiple myeloma, by 35-40%. Even something as simple as tea can matter.
How to Protect Yourself
You don’t have to give up supplements. But you need to be smart.- Always tell your doctor and pharmacist what you’re taking-even if you think it’s ‘just a vitamin.’ Write it down. Bring the bottle. Don’t say ‘I take something for my memory.’ Say ‘I take ginkgo biloba, 120 mg daily.’
- Check your labels. Many ‘brain health’ supplements contain ginkgo. ‘Mood support’ products often have St. John’s Wort. ‘Immune boosters’ may include garlic. Read the ingredients.
- Know the warning signs. If you’re on warfarin and notice unusual bruising, nosebleeds, or dark stools, stop the supplement and call your doctor. If you’re on antidepressants and feel agitated, sweaty, or feverish, seek help immediately-those could be signs of serotonin syndrome.
- Use trusted resources. The National Center for Complementary and Integrative Health (NCCIH) has a free, updated herb-drug interaction checker. Memorial Sloan Kettering’s database is another reliable source.
- Don’t assume ‘natural’ means safe. A 2019 University of Michigan survey found 76% of supplement users believed that. That myth kills.
What Your Pharmacist Can Do
Pharmacists are your frontline defense. They see your full prescription list and can spot conflicts before you even walk out the door. The Stockley’s Herbal Medicine Interactions protocol (2023 edition) gives pharmacists clear guidelines:- For ginkgo + warfarin: Check INR within 72 hours of starting, then weekly.
- For St. John’s Wort + antidepressants: Use the Hunter Criteria to screen for serotonin syndrome at every visit.
- For garlic + anticoagulants: Monitor for bruising and bleeding, even if INR looks normal.


Lynsey Tyson
December 19, 2025 AT 12:02I took St. John’s Wort for a few months last year thinking it was just a ‘natural mood boost.’ Didn’t tell my doctor. Then my birth control failed. Total accident. Now I’m on a different supplement and I tell every provider I see. Don’t be like me.
Just say no to assuming ‘natural’ = safe.
Allison Pannabekcer
December 20, 2025 AT 17:05My grandma swears by ginkgo for memory. She’s on warfarin. I’ve been begging her to stop. She says ‘it’s just a leaf.’
Two weeks ago she bruised her thigh for no reason. ER visit. INR was 7.9. She’s not taking it anymore. But she still buys it ‘for the antioxidants.’
We need better education. Not just warnings. Real conversations.
Pharmacists should hand out pamphlets with every prescription. Not just when you ask.
anthony funes gomez
December 22, 2025 AT 05:42Pharmacokinetic modulation via CYP450 is the core issue-not the ‘natural’ fallacy. The regulatory vacuum under DSHEA is a failure of risk governance, not consumer ignorance.
Garlic’s allicin inhibits CYP3A4 with an IC50 of 12.3μM-comparable to grapefruit juice. Yet we treat it like a spice, not a pharmacologically active compound.
CoQ10’s interaction with warfarin? Likely mediated by VKORC1 downregulation. But nobody’s funded the RCTs because supplements aren’t patentable.
And yes, the FDA’s reactive stance is indefensible. Pre-market approval should be mandatory for any substance with known enzyme affinity. Period.
Dikshita Mehta
December 24, 2025 AT 04:02I work in a clinic in Delhi and see this all the time. People take ashwagandha with thyroid meds. Or turmeric with blood thinners. They say ‘it’s Ayurvedic, so it’s fine.’
We need a simple checklist: 1) What are you taking? 2) Why? 3) Did your doctor know?
It’s not about scaring people. It’s about making sure they don’t get hurt because no one asked.
Gloria Parraz
December 25, 2025 AT 13:27I almost lost my dad because of hawthorn. He had heart failure. Took it because he read it ‘helps circulation.’ Combined it with metoprolol. His BP dropped to 78/45. He collapsed in the kitchen.
He’s fine now. But he doesn’t take anything without me checking it first.
Doctors don’t have time. Pharmacists don’t always ask. So we have to be our own advocates.
Bring the bottle. Show the label. Say ‘I need to know if this kills me.’
It’s not dramatic. It’s survival.
Sahil jassy
December 26, 2025 AT 21:01Carolyn Benson
December 27, 2025 AT 03:14Of course you’re not supposed to mix herbs and drugs. Everyone knows that. But people are lazy. They want a magic pill that fixes everything without changing their habits.
And now we have this cult of ‘natural wellness’ where people think science is corporate propaganda.
It’s not that supplements are dangerous. It’s that people are stupid enough to think they can outsmart biology.
Stop glorifying ignorance. It’s killing people.
Chris porto
December 27, 2025 AT 10:54I get it. You want to feel better. But if you’re on meds, just stick to the basics: food, sleep, walking.
I used to take magnesium for cramps. Then I realized my blood pressure was dropping too low. Stopped it. No side effects. Life went on.
Why complicate it? You don’t need a 12-ingredient ‘energy blend’ to be healthy.
Simple wins.
Aadil Munshi
December 28, 2025 AT 19:01Let’s be real. The whole ‘herbal supplement’ industry is a pyramid scheme disguised as wellness.
St. John’s Wort? It’s basically an SSRI with worse dosing control.
Garlic pills? You’d get the same effect from eating three cloves and saving $20.
And don’t even get me started on CoQ10. The only people who benefit are the guys selling it.
90% of these are placebo with side effects.
And yet people spend thousands a year on ‘immune boosters’ that do nothing but empty their wallets.
It’s not science. It’s capitalism preying on fear.
Glen Arreglo
December 29, 2025 AT 14:09I’m from the Philippines. In my village, we use turmeric for everything-wounds, inflammation, even digestion.
But we also know when to stop. When someone’s on blood thinners? We don’t touch turmeric. We ask the local nurse.
It’s not about fear. It’s about respect-for the medicine, for the body, for the people who made it.
We don’t need apps or databases. We need community wisdom.
And maybe a little humility.
shivam seo
December 30, 2025 AT 04:43U.S. is so soft. You can buy poison in a bottle labeled ‘natural energy.’
In Australia, if you want something that affects your liver, you need a script. Simple.
Why does America let anyone sell ‘immune boosters’ that interfere with chemo?
It’s not freedom. It’s negligence.
And you wonder why healthcare costs are insane?
Mike Rengifo
December 30, 2025 AT 21:29I take ashwagandha for stress. My doc knows. We checked my thyroid levels. All good.
Point is-you don’t have to quit everything. Just talk to someone who knows what they’re talking about.
It’s not rocket science. Just don’t be lazy.
Ashley Bliss
December 31, 2025 AT 12:26They say ‘natural’ means safe. But what about the 17 companies the FDA caught hiding actual drugs in their ‘herbal’ products?
That’s not a mistake. That’s evil.
And the people who sell this stuff? They don’t care if you bleed out. They care about their next quarterly report.
So you think you’re being healthy? You’re being used.
Wake up. Your life isn’t a marketing campaign.