More people than ever are popping herbal supplements like they’re candy-turmeric for inflammation, green tea extract for weight loss, ashwagandha for stress. But what if these "natural" fixes are quietly harming your liver? The truth is, your liver doesn’t care if something is labeled "organic," "plant-based," or "ancient remedy." If it’s toxic, your liver has to process it. And for some supplements, that’s a dangerous job.
These six supplements are linked to serious liver damage
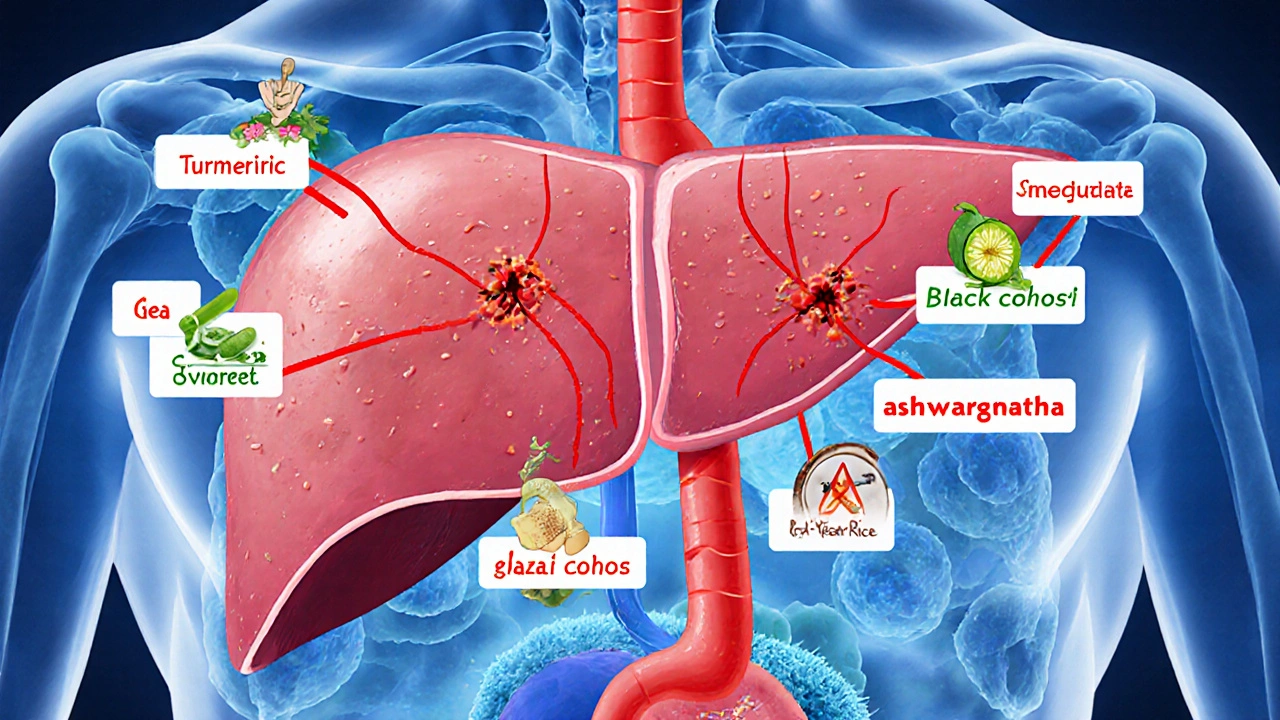
A 2024 study in JAMA Network Open analyzed real-world cases of liver injury tied to dietary supplements and pinpointed six botanicals that show up again and again in hospital reports: turmeric (or curcumin), green tea extract, Garcinia cambogia, black cohosh, red yeast rice, and ashwagandha. These aren’t rare outliers-they’re the most common culprits.
Take turmeric. It’s everywhere: smoothies, golden lattes, capsules. But high-dose turmeric supplements have landed people in the hospital with acute hepatitis. One study found that people taking over 1,000 mg of curcumin daily were far more likely to develop liver enzyme spikes. And it’s not just the turmeric-it’s the concentration. Powdered spice in food? Generally safe. A 500 mg capsule taken twice a day? That’s a different story.
Green tea extract is another big one. While drinking green tea is fine, concentrated extracts-often sold for weight loss-pack in massive amounts of EGCG, a compound that can overwhelm liver cells. Consumer Reports tested supplements in 2023 and found that 25% of green tea extract products exceeded safe daily limits for EGCG. That’s not a typo. Some pills had enough to match the liver stress of drinking 10-15 cups of tea.
Black cohosh, often used for menopause symptoms, has been tied to liver failure in multiple case reports. Red yeast rice, marketed as a "natural statin," contains monacolin K-the same active ingredient as the prescription drug lovastatin. But unlike prescription meds, there’s no standardization. One batch might be safe; another could have enough to cause muscle breakdown and liver injury.
Ashwagandha is trending for stress and sleep, but the liver doesn’t distinguish between "adaptogen" and toxin. In clinical studies, people taking ashwagandha supplements developed jaundice, nausea, and elevated liver enzymes-even without pre-existing conditions.
What’s really in your supplement bottle?
Here’s the scary part: what’s on the label isn’t always what’s inside. The NIH’s LiverTox database found that up to 60% of herbal supplements are mislabeled or adulterated. That means you think you’re taking pure ashwagandha, but you might be getting a mix of herbs, heavy metals, or even hidden pharmaceuticals.
Testing by the FDA and independent labs has turned up:
- Lead in 18% of tested products
- Mercury in 12%
- Arsenic in 9%
- Sildenafil (Viagra) in 22% of sexual enhancement supplements
- NSAIDs like ibuprofen in 15% of pain relief formulas
- Corticosteroids in 8% of "natural" anti-inflammatories
One notorious case involved OxyELITE Pro®, a popular weight-loss supplement. After dozens of users developed liver failure, testing revealed it contained aegeline-a compound from the bael fruit that wasn’t even listed as an ingredient. The FDA had to pull it from shelves.
Even the source matters. Herbal potency changes based on where it’s grown, when it’s harvested, and which part of the plant is used. A root might be safe; the leaf from the same plant could be toxic. Soil contamination adds more risk: plants absorb heavy metals from polluted ground. No one tests for this before it hits the shelf.
Your liver doesn’t warn you-until it’s too late
Unlike a broken bone or a fever, liver damage doesn’t scream for attention. Most people don’t feel anything until their liver is already injured. By then, enzymes like ALT and AST are already elevated, and symptoms like fatigue, nausea, dark urine, and abdominal pain are already present.
According to the NIH LiverTox database, the most common signs of supplement-induced liver injury are:
- Fatigue (87% of cases)
- Abdominal pain (76%)
- Nausea (68%)
- Dark urine (52%)
- Yellowing skin or eyes (jaundice, 34%)
These symptoms often show up after weeks or months of daily use. People assume they’re just "tired" or have a "stomach bug." They don’t connect it to the turmeric pill they take every morning or the green tea extract they started for weight loss.
And here’s the kicker: liver damage from supplements looks identical to damage from prescription drugs. A 2023 report from Weill Cornell Medicine made this clear: "The liver can’t tell the difference between a pill from a pharmacy and a capsule from a health store."

Why regulation doesn’t protect you
Unlike prescription drugs, herbal supplements don’t need FDA approval before they’re sold. The FDA can’t require safety studies, clinical trials, or even accurate labeling. They can only act after someone gets hurt-and even then, the process is slow.
There’s no official daily limit for turmeric, ashwagandha, or green tea extract. The Office of Dietary Supplements sets upper limits for vitamins and minerals-but not for herbs. That means manufacturers can pack in as much as they want. And without standardized dosing, one brand’s "high potency" could be 10 times stronger than another’s.
Even worse, many supplements are sold online through social media. TikTok influencers push "liver cleanse" blends or "detox" teas with no scientific backing. A 2024 article in Medical News Today showed that social media is driving a spike in supplement use among young adults-exactly the group least likely to ask a doctor about risks.
Who’s most at risk?
Not everyone who takes these supplements gets hurt. But some people are far more vulnerable. Think of it like a food allergy: most people can eat peanuts fine. A small percentage have a severe reaction. The same goes for liver toxicity.
Research suggests genetics play a role. One 2022 study in Hepatology linked a specific gene variant-HLA-B*35:01-to increased risk of liver injury from certain herbs. People with this gene may react badly to even small doses.
Other risk factors include:
- Pre-existing liver disease (fatty liver, hepatitis, cirrhosis)
- Using multiple supplements at once
- Taking supplements with alcohol or prescription meds
- Long-term use (more than 3-6 months)
- Age over 50
And don’t assume "natural" means safe for pregnant women, children, or people with autoimmune conditions. The risks are higher, and data is even scarcer.

What you can do to protect your liver
Here’s the practical stuff:
- Stop taking supplements if you feel unwell. Fatigue, nausea, or dark urine aren’t normal. Stop immediately and see a doctor.
- Tell your doctor about every supplement you take. The American College of Gastroenterology now recommends that doctors ask about supplements during every liver function check. Don’t assume they’ll ask-you need to bring it up.
- Avoid high-dose extracts. Stick to whole-food sources when possible. Eat turmeric in curry, not in a 1,000 mg capsule.
- Check third-party testing. Look for supplements with USP, NSF, or ConsumerLab verification. These aren’t perfect, but they’re better than nothing.
- Don’t stack supplements. Taking 5 different herbs at once multiplies your risk. Less is more.
- Be skeptical of TikTok trends. If it sounds too good to be true-"lose 10 pounds in 2 weeks with this tea"-it probably is.
There’s no magic supplement that replaces sleep, exercise, and a balanced diet. If you’re taking something for energy, stress, or weight loss, ask yourself: Is this helping-or hurting?
What to do if you think your liver is damaged
If you’ve been taking herbal supplements and notice symptoms like fatigue, nausea, or yellowing skin:
- Stop all supplements immediately.
- Don’t wait for symptoms to get worse.
- See your doctor and ask for a liver panel (ALT, AST, bilirubin, alkaline phosphatase).
- Bring the supplement bottles with you.
- Report the case to the FDA’s MedWatch program.
Early detection can prevent permanent damage. Many people recover fully once they stop the offending supplement. But delay can mean hospitalization-or worse.
The bottom line: Just because something is sold as a "natural remedy" doesn’t mean it’s safe. Your liver works hard every day. Don’t ask it to detoxify unregulated, untested, and potentially toxic substances.
Can turmeric really hurt your liver?
Yes. While turmeric spice in food is generally safe, high-dose turmeric supplements-especially those with concentrated curcumin-have been linked to liver injury in multiple studies. Cases include hepatitis, jaundice, and elevated liver enzymes. The risk increases with doses over 1,000 mg daily and long-term use.
Is green tea extract dangerous for the liver?
Yes, especially in extract form. Drinking brewed green tea is fine, but concentrated extracts can deliver excessive amounts of EGCG, a compound that overwhelms liver cells. Consumer Reports found 25% of green tea extract supplements exceeded safe daily limits. This has led to hospitalizations for acute hepatitis.
Are herbal supplements regulated like medications?
No. Unlike prescription drugs, herbal supplements don’t need FDA approval before being sold. Manufacturers aren’t required to prove safety, effectiveness, or accurate labeling. The FDA can only act after harm is reported-and even then, removal is slow and rare.
What supplements should I avoid if I have liver disease?
If you have fatty liver, hepatitis, or cirrhosis, avoid all herbal supplements unless approved by your hepatologist. The six most commonly implicated ones are turmeric, green tea extract, Garcinia cambogia, black cohosh, red yeast rice, and ashwagandha. Even "mild" herbs like valerian and ginseng have been linked to liver enzyme spikes in sensitive individuals.
Can supplements cause liver failure?
Yes. Between 2007 and 2015, herbal and dietary supplements caused 21.1% of drug-induced liver failure cases in the U.S., according to the Acute Liver Failure Study Group. Products like OxyELITE Pro®, black cohosh, and high-dose green tea extract have led to transplants and death.
How do I know if a supplement is safe?
There’s no guaranteed way, but you can reduce risk: look for third-party tested products (USP, NSF, ConsumerLab), avoid high-dose extracts, stick to whole-food sources, and never take more than one herbal supplement at a time. If you’re unsure, talk to your doctor or a registered dietitian.

Holli Yancey
November 18, 2025 AT 15:29I’ve been taking ashwagandha for anxiety for over a year-never thought twice about it until I read this. My ALT levels were borderline high last checkup, and my doctor didn’t even ask about supplements. I’ve already stopped. Feels weird to admit I trusted a TikTok influencer more than my own body.
Gordon Mcdonough
November 19, 2025 AT 15:40WHAT THE F*** IS THIS NATION COMING TO?! YOU CAN’T JUST TAKE SOME HERBS AND THINK YOU’RE BEING HEALTHY!!! THIS IS WHY AMERICA IS FALLING APART!!! PEOPLE ARE MORE AFRAID OF PHARMACIES THAN THEY ARE OF POISON!!! THE FDA IS ASLEEP AT THE WHEEL!!!
Jessica Healey
November 20, 2025 AT 07:41omg i literally just bought that green tea extract for weight loss last week 😭 i thought it was 'natural' so it was safe?? now im paranoid i'm gonna wake up yellow. why does no one warn you???
Levi Hobbs
November 21, 2025 AT 08:31This is such an important post. I’m a pharmacist, and I see this all the time-patients come in with liver enzyme spikes and swear they ‘only take herbs.’ The lack of regulation is terrifying. I always tell my patients: if it’s not on the label, it’s not safe. Look for USP or NSF seals. And please, please tell your doctor what you’re taking-even if you think it’s ‘just turmeric.’
henry mariono
November 22, 2025 AT 09:21I appreciate this. I’ve been taking red yeast rice for cholesterol since my dad had a heart attack. I didn’t know it was basically lovastatin. I’m going to stop and talk to my cardiologist. Thanks for the clarity.
Sridhar Suvarna
November 23, 2025 AT 06:39As someone from India where Ayurveda is part of daily life I must say this is a wake up call. We have centuries of tradition but modern extraction methods and global supply chains have changed everything. What was safe in village kitchens is now concentrated and sold as a miracle cure. We need global standards not just in the US but everywhere.
Joseph Peel
November 23, 2025 AT 11:31The irony is that people who reject pharmaceuticals often trust supplements with zero oversight. The liver doesn’t care about marketing. It only cares about biochemistry. If you’re going to take something daily, demand third-party testing. If you can’t find it, don’t take it.
Kelsey Robertson
November 23, 2025 AT 21:10Oh please. This is just Big Pharma fearmongering. Turmeric has been used for 4,000 years. You think a few lab rats in a corporate-funded study are more trustworthy than ancient wisdom? The real toxin here is the medical-industrial complex trying to scare you out of natural healing. Wake up.
Joseph Townsend
November 24, 2025 AT 15:32I took black cohosh for hot flashes and ended up in the ER with jaundice. My liver enzymes were through the roof. I thought I was being ‘holistic.’ Turns out I was just poisoning myself with a $30 bottle from Amazon. Now I’m on the other side of the fence: if it doesn’t come with a prescription label and a 12-page insert, I don’t touch it. My liver thanked me.