When you're trying to manage type 2 diabetes and lose weight at the same time, most medications make you choose one or the other. Insulin helps control blood sugar but often leads to weight gain. Metformin might help a little with weight, but not enough for many people. That’s where GLP-1 receptor agonists change the game. These aren’t just another diabetes pill-they’re a powerful tool that tackles both high blood sugar and excess weight, often at the same time.
How GLP-1 Receptor Agonists Actually Work
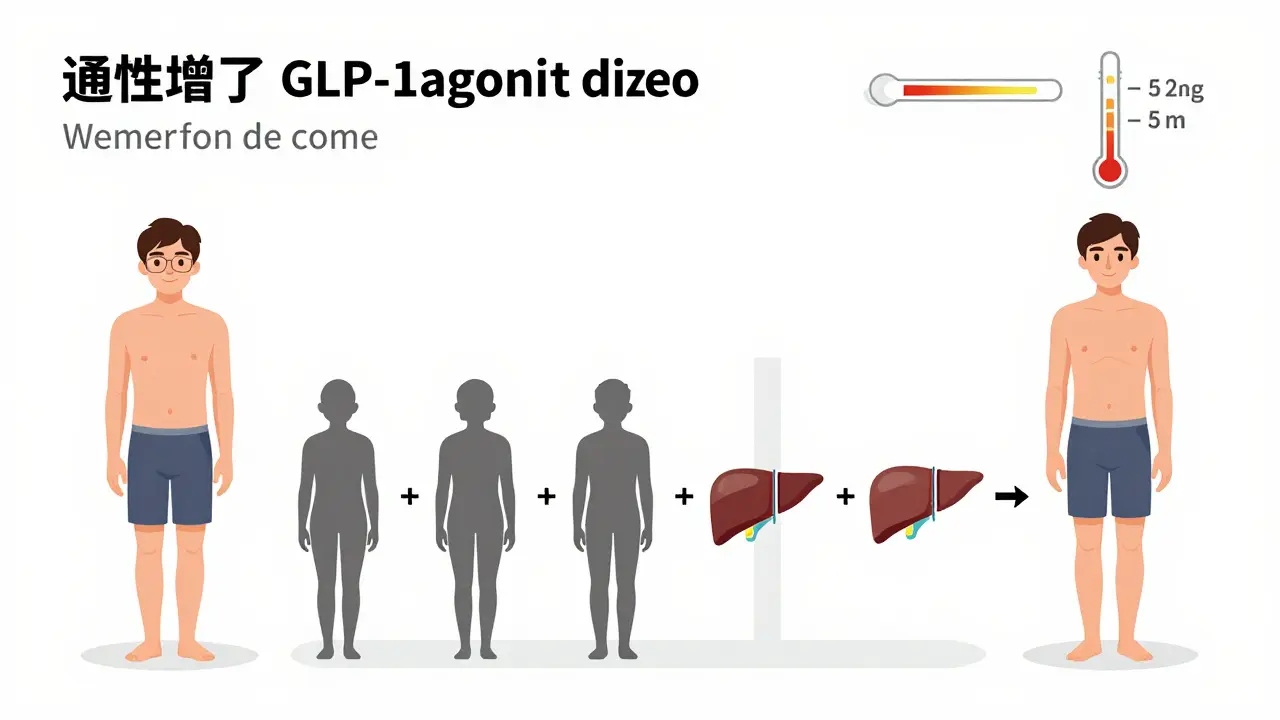
GLP-1 receptor agonists mimic a hormone your body already makes called glucagon-like peptide-1. This hormone is released by your gut after you eat. It tells your pancreas to release insulin when blood sugar rises, but only when it’s needed-so it doesn’t cause dangerous low blood sugar like some other drugs. It also tells your liver to stop making so much glucose, slows down how fast food leaves your stomach, and sends a clear signal to your brain: you’re full.
That last part is key. Most weight loss drugs just suppress appetite. GLP-1 agonists do that, but they also change how your brain responds to food. Studies show they reduce cravings for sugary, high-fat foods by targeting specific areas in the hypothalamus. People on these drugs often say, “I used to think about food all the time. Now, I just don’t care as much.” It’s not willpower-it’s biology.
And the numbers back it up. In clinical trials, semaglutide (the active ingredient in Ozempic and Wegovy) lowered A1C by up to 1.8% on average. For someone with an A1C of 9%, that’s a drop to 7.2%-well within the target range. At the same time, people lost 10-15% of their body weight. That’s not a few pounds. For someone weighing 200 pounds, that’s 20 to 30 pounds gone. And it’s not just temporary. As long as you keep taking it, the results stick.
Which Drugs Are Available and How Do They Compare?
There are several GLP-1 agonists on the market, but not all are created equal. Here’s what you need to know:
| Drug Name | Brand Names | Frequency | A1C Reduction | Average Weight Loss |
|---|---|---|---|---|
| Exenatide | Byetta, Bydureon | Twice daily or weekly | 0.8-1.1% | 4-6% |
| Liraglutide | Victoza, Saxenda | Daily | 1.0-1.1% | 5-7% |
| Dulaglutide | Trulicity | Weekly | 1.1-1.6% | 5-8% |
| Semaglutide | Ozempic, Wegovy | Weekly | 1.5-1.8% | 10-15% |
| Tirzepatide | Mounjaro, Zepbound | Weekly | 1.8-2.4% | 15-21% |
Tirzepatide (Zepbound) is the newest and strongest. It’s not just a GLP-1 agonist-it also activates GIP receptors, another gut hormone that boosts insulin and suppresses appetite. In the SURMOUNT-1 trial, people on the highest dose lost over 20% of their body weight. That’s more than most bariatric surgeries achieve.
But you don’t need the strongest drug to see results. Even liraglutide (Saxenda), approved for weight loss, helped people lose an average of 8% of their weight over a year. The difference between drugs isn’t just about strength-it’s about how often you inject, how quickly you reach the full dose, and how your body reacts to side effects.
Side Effects: What to Expect and How to Handle Them
These drugs work so well because they affect your gut and brain. But that also means your stomach might not like them-at least at first.
Nausea is the most common side effect. About 1 in 5 people feel it, especially when starting or increasing the dose. Vomiting happens in about 1 in 10. Diarrhea and constipation are also common. Most of these side effects fade after a few weeks as your body adjusts.
The best way to reduce them? Go slow. All GLP-1 agonists require a gradual dose increase. Semaglutide starts at 0.25 mg per week for a month, then moves up every 4 weeks until you hit the full dose. Rushing this process makes side effects worse. Many people give up too soon because they think the nausea means it’s not working. It doesn’t. It just means you’re moving too fast.
Other tips:
- Take your dose at night-it helps reduce nausea during the day.
- Avoid greasy or fried foods while titrating up.
- Stay hydrated. Dehydration makes nausea worse.
- Over-the-counter medications like dimenhydrinate (Dramamine) can help if nausea is severe.
Some people worry about injections. But the pens used today are tiny, with fine needles. Most users say they’re easier than expected. A survey found that 85% of people are self-administering successfully after just two or three tries.
Weight Loss Isn’t Permanent-Unless You Keep Taking It
This is the hard truth: if you stop, you’ll likely gain the weight back. Studies show that within a year of stopping, most people regain more than half of what they lost. That’s not a failure-it’s biology. Your body is trying to return to its old weight set point.
Think of GLP-1 agonists like blood pressure medication. You don’t stop taking it because you feel better-you keep taking it because it’s still working. The same applies here. For many, this isn’t a short-term fix. It’s a long-term tool for managing metabolic health.
That’s why experts now talk about GLP-1 agonists as “metabolic reset” drugs. They don’t just help you lose weight-they help your body function better. Insulin sensitivity improves. Blood pressure drops. Liver fat decreases. Even cholesterol levels get better.
Cost and Access: The Biggest Hurdle
These drugs are expensive. Without insurance, a monthly supply of semaglutide can cost $1,000 or more. Even with insurance, many plans require you to try other weight loss methods first-like diet counseling or older medications-before approving coverage.
In the U.S., Medicare Part D covers about 62% of GLP-1 prescriptions, but only if you have a BMI over 30 and a weight-related condition like high blood pressure or sleep apnea. Private insurers vary widely. Some require proof of failed attempts with other treatments. Others limit coverage to diabetes patients only, not those using it for weight loss.
There’s also a global shortage. Because demand has exploded, Novo Nordisk (maker of Ozempic and Wegovy) can’t make enough to meet it. In 2023, the FDA listed semaglutide as in shortage. That means some pharmacies run out. Some doctors delay starting patients until supply improves.
What’s Next? The Future of GLP-1 Drugs
The next wave of drugs is even more exciting. Tirzepatide (Zepbound) is already showing better results than semaglutide. Now, researchers are testing triple agonists that target GLP-1, GIP, and glucagon-all at once. Early data suggests even greater weight loss and better blood sugar control.
There’s also talk of oral versions. Right now, all GLP-1 agonists are injections. But Novo Nordisk has an oral semaglutide pill (Rybelsus) approved for diabetes. It’s less effective than the injection, but it’s a start. If they can make an oral version as strong as Wegovy, access will explode.
And it’s not just diabetes and obesity anymore. Studies are looking at using these drugs for non-alcoholic fatty liver disease, heart failure, and even Alzheimer’s. Early results show reduced brain inflammation and improved memory in animal models. Human trials are just beginning.
Who Should Consider These Drugs?
GLP-1 agonists aren’t for everyone. But they’re a game-changer for:
- People with type 2 diabetes who need better A1C control and have struggled with weight gain from other meds
- People with obesity (BMI ≥30) or overweight (BMI ≥27) with at least one weight-related condition
- Those who’ve tried diet and exercise but hit a plateau
- People who want a non-surgical option for significant weight loss
They’re not recommended for people with a personal or family history of medullary thyroid cancer or multiple endocrine neoplasia syndrome type 2. They’re also not approved for use in pregnancy or in people under 18.
If you’re considering one, talk to your doctor. Bring your A1C numbers, your weight history, and a list of other medications you’re taking. Ask about your insurance coverage. Ask about the titration plan. Ask what to do if side effects hit hard.
These drugs aren’t magic. But for the first time in decades, we have a treatment that doesn’t just manage diabetes-it reverses some of its worst effects. And that’s something worth understanding.
Do GLP-1 agonists cure diabetes?
No, they don’t cure diabetes. They help manage it by lowering blood sugar and improving insulin sensitivity. Many people see their A1C drop into the normal range, but if they stop taking the drug, blood sugar levels usually rise again. It’s a long-term management tool, not a cure.
Can I take GLP-1 agonists without having diabetes?
Yes. Wegovy and Zepbound are FDA-approved for chronic weight management in adults with obesity or overweight and at least one weight-related condition, even if they don’t have diabetes. Ozempic is approved only for diabetes, but doctors can prescribe it off-label for weight loss.
How long does it take to see weight loss results?
Most people start seeing weight loss within 4 to 8 weeks. But the full effect takes time. Because dosing is gradual, it can take 16 to 20 weeks to reach the highest dose. The biggest weight loss typically happens between 6 and 12 months.
Are GLP-1 agonists safe for long-term use?
Current data shows they’re safe for long-term use. The LEADER trial followed patients on liraglutide for over 5 years and found no increased risk of serious side effects. In fact, they reduced heart attacks and strokes in high-risk patients. Ongoing studies are tracking safety beyond 10 years.
Can I drink alcohol while taking a GLP-1 agonist?
Moderate alcohol is usually fine, but it can increase the risk of low blood sugar, especially if you have diabetes. Alcohol also worsens nausea and dehydration, which are already common side effects. It’s best to limit alcohol, especially when starting or adjusting your dose.


sue spark
December 15, 2025 AT 16:34These drugs are amazing but I worry about how fast they're being pushed without long-term data
Colleen Bigelow
December 15, 2025 AT 22:36Oh please here we go again with Big Pharma’s latest magic bullet-next they’ll tell us the moon landing was faked and this is the real cure for diabetes. They’re not fixing your metabolism they’re locking you into a $1000/month subscription for life. Wake up people this isn’t medicine it’s corporate slavery wrapped in a pen.
Elizabeth Bauman
December 16, 2025 AT 18:36Colleen you’re not wrong but let’s be real-the FDA didn’t approve this because they’re in bed with Novo Nordisk they approved it because the data is rock solid. People are dropping 30 pounds and reversing prediabetes. If you want to live in a tin-foil world fine but don’t drag the rest of us down with your paranoia. This isn’t a scam it’s science.
SHAMSHEER SHAIKH
December 18, 2025 AT 06:44Dear friends, I write from India where access to these medications remains a distant dream for most. Yet, the science behind GLP-1 agonists is profoundly beautiful-nature’s own satiety signal, amplified. We must not allow cost or geography to become barriers to health. Let us advocate, let us educate, let us demand equitable access-for every human being deserves the chance to heal their metabolism, not merely manage it.
James Rayner
December 18, 2025 AT 12:46I’ve been on semaglutide for 11 months. Lost 28 lbs. My A1C dropped from 8.1 to 5.7. But honestly? The weirdest part wasn’t the weight loss. It was how quiet my mind got around food. I used to spiral over snacks like they were life-or-death. Now? I eat when I’m hungry. I stop when I’m full. It’s like my brain finally stopped screaming. I don’t know if this is a drug or a reset. I just know I feel more like myself than I have in 15 years.
Dylan Smith
December 19, 2025 AT 11:26My doctor told me to try this after I gained 40 lbs on insulin. I started at 220 lbs. Now I’m 172. I didn’t change my diet. I didn’t start working out. I just stopped thinking about food like it was my emotional crutch. I’m not saying this is for everyone but if you’ve been stuck for years this might be the key you didn’t know you were holding
Mike Smith
December 21, 2025 AT 05:08For anyone considering this: patience is non-negotiable. I went from 0.25 mg to 1.7 mg over 16 weeks. Nausea? Yes. Vomiting? Once. I stuck with it because I knew it wasn’t the drug-it was the pace. Your body isn’t broken. It’s just been overwhelmed. These drugs give you back control-not by force, but by restoring balance. Trust the process. And if you feel discouraged? Remember: this isn’t a sprint. It’s a recalibration.
Kitty Price
December 22, 2025 AT 15:15Just started the 0.25mg. Nausea is real but manageable. Took it at night like they said. Slept through it. No drama. Still can’t believe I’m actually doing this. 😌