Fluoroquinolone & NSAID Risk Calculator
Assess Your Risk
Risk Assessment
Key Findings
Important: This tool is for educational purposes only. Always consult your healthcare provider for medical advice.
What you need to know:
- Combining fluoroquinolones with NSAIDs increases kidney injury risk by 3.5-fold in elderly patients (per JAMA Internal Medicine study)
- Fluoroquinolones alone can cause permanent nerve damage in 32% of cases
- After age 40, kidney clearance drops by about 1% per year
- NSAIDs reduce kidney blood flow by blocking protective prostaglandins
When you’re sick with a urinary tract infection or sinusitis, your doctor might reach for a fluoroquinolone antibiotic like ciprofloxacin or levofloxacin. It’s fast, powerful, and often works when other antibiotics don’t. But if you’re also taking ibuprofen or naproxen for pain or inflammation, you could be putting yourself at risk for serious, sometimes permanent, damage to your kidneys and nervous system - even if you’re otherwise healthy.
What Are Fluoroquinolone Antibiotics?
Fluoroquinolones are a class of antibiotics that include ciprofloxacin, levofloxacin, moxifloxacin, norfloxacin, and ofloxacin. They’ve been used since the 1980s to treat stubborn bacterial infections - especially urinary tract infections, pneumonia, and some types of gastrointestinal infections. They work by stopping bacteria from reproducing, which makes them effective against a wide range of bugs.
But their power comes with a price. Since 2016, regulatory agencies like the U.S. FDA, Health Canada, and the European Medicines Agency have issued multiple warnings about these drugs. The biggest concerns? Tendon ruptures, nerve damage, and serious neurological reactions. In 2017, Health Canada updated its safety guidelines to say these side effects can be persistent and disabling, even after stopping the drug. The UK’s MHRA followed in 2019, restricting fluoroquinolones to only the most serious infections where no other options exist.
Why the crackdown? Data from the EU’s EudraVigilance system showed 286 cases of long-lasting, disabling reactions over 21 years - and that’s just the ones reported. Real-world patient surveys suggest this number is likely much higher. One study of 1,245 patients found that 78% had symptoms lasting over six months after stopping fluoroquinolones, and 32% reported permanent disability.
How Fluoroquinolones Hurt Your Kidneys
Your kidneys filter toxins out of your blood. Fluoroquinolones can interfere with that process in several ways. The most common is acute interstitial nephritis - an inflammatory reaction in the kidney tissue that can cause sudden kidney failure. This isn’t rare. A 2013 study published in PMC3708027 found that men taking fluoroquinolones had a twofold higher risk of needing hospitalization for acute kidney injury.
Another risk is crystalluria - when the drug forms crystals in your urine, especially if your urine is too alkaline (pH above 6.8). These crystals can block tiny tubes in the kidneys, leading to damage. In rare cases, fluoroquinolones cause acute tubular necrosis, where kidney cells die off. This can lead to permanent loss of function.
Even worse, these risks get worse if you’re older, dehydrated, or already have reduced kidney function. After age 40, kidney clearance drops by about 1% per year. By 60, you’re already at higher risk - and fluoroquinolones can push you over the edge.
NSAIDs: The Silent Kidney Killer
NSAIDs - nonsteroidal anti-inflammatory drugs like ibuprofen, naproxen, and diclofenac - are among the most common pain relievers in the world. But they’re not harmless. They work by blocking enzymes called COX-1 and COX-2, which reduce inflammation and pain. But they also block prostaglandins, chemicals your kidneys need to maintain blood flow.
When you take an NSAID, your kidneys get less blood. That lowers your glomerular filtration rate (GFR), which measures how well your kidneys filter waste. In healthy people, this isn’t a big deal. But in older adults, those with high blood pressure, diabetes, or existing kidney disease, it can trigger acute kidney injury.
Studies show that when NSAIDs are taken alone, they increase the risk of hospitalization for kidney injury by about 1.5 times. But when you combine them with fluoroquinolones, the risk jumps dramatically. A 2013 study in JAMA Internal Medicine found that in elderly patients, the combination led to a 3.5-fold increase in acute kidney injury.
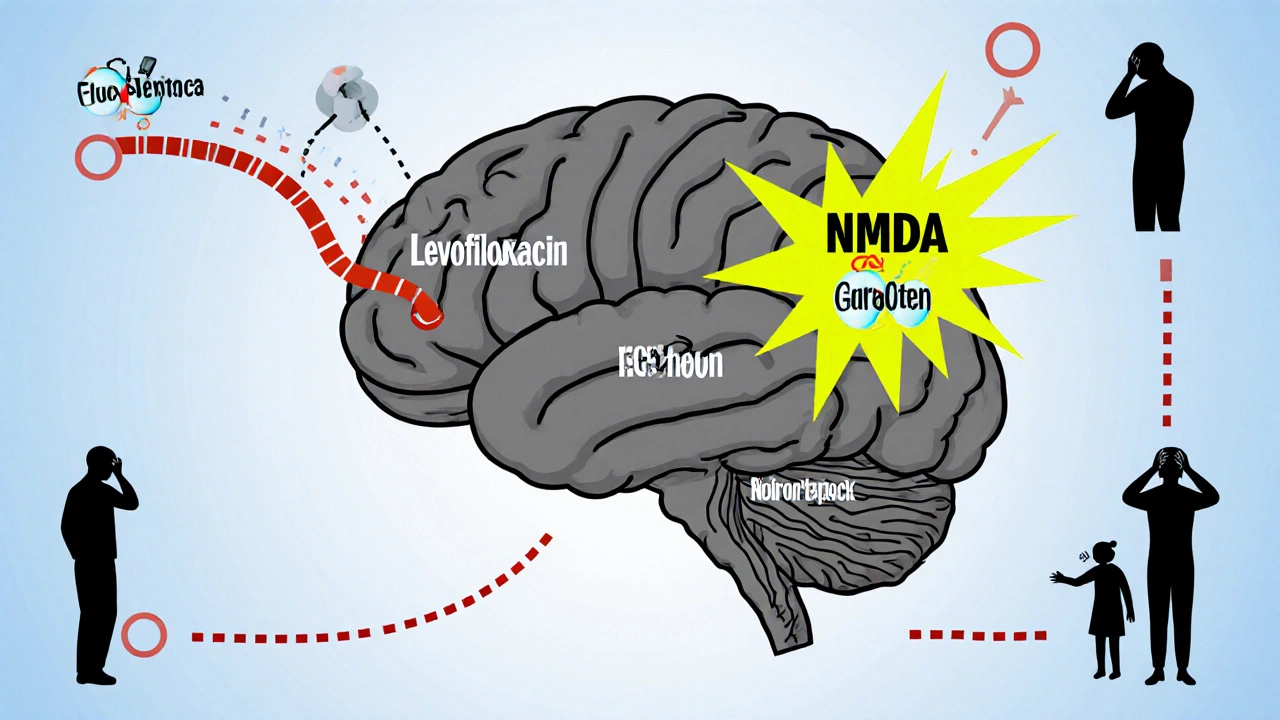
Neurological Risks: When Your Brain Gets Hit
Fluoroquinolones don’t just attack bacteria - they can also mess with your brain. These antibiotics cross the blood-brain barrier and interfere with GABA receptors, the brain’s main calming system. At the same time, they overstimulate NMDA receptors, which are linked to excitability and seizures.
The result? Confusion, hallucinations, seizures, delirium, and even psychosis. Levofloxacin is especially linked to seizures. Ciprofloxacin is notorious for causing mental fogginess. And ofloxacin? It’s less likely to cause neurological issues - but only because it’s less common now.
NSAIDs aren’t innocent here either. While they don’t usually cause major brain problems, they can trigger headaches, dizziness, and - very rarely - aseptic meningitis. This is a painful inflammation of the brain’s protective membranes, often mistaken for infection.
When you combine both drugs, the danger multiplies. If your kidneys are already struggling to clear the fluoroquinolone, the drug builds up in your blood. Studies show that in moderate kidney impairment (eGFR 30-59 mL/min), fluoroquinolone levels can rise by 50-100%. That means more drug reaching your brain - and a much higher chance of neurotoxicity.
A Real Case: What Happens When Things Go Wrong
In 2021, a 58-year-old man in the UK was prescribed ciprofloxacin 500mg twice daily for a urinary tract infection. He was also taking ibuprofen 400mg three times a day for back pain. Within three days, he developed severe nausea, confusion, and a sudden spike in creatinine - from 82 to 287 μmol/L. He was hospitalized with acute kidney injury and peripheral neuropathy.
His symptoms didn’t go away after stopping the drugs. Eighteen months later, he still had burning pain in his feet, muscle weakness, and brain fog. His case was reported to the UK’s Yellow Card system (reference: 11622674). He wasn’t alone. Online communities like Reddit’s r/FQAntibioticDamage have over 14,500 members sharing stories of people who developed chronic pain, nerve damage, and cognitive decline after standard fluoroquinolone courses - often while also taking NSAIDs.
What Should You Do Instead?
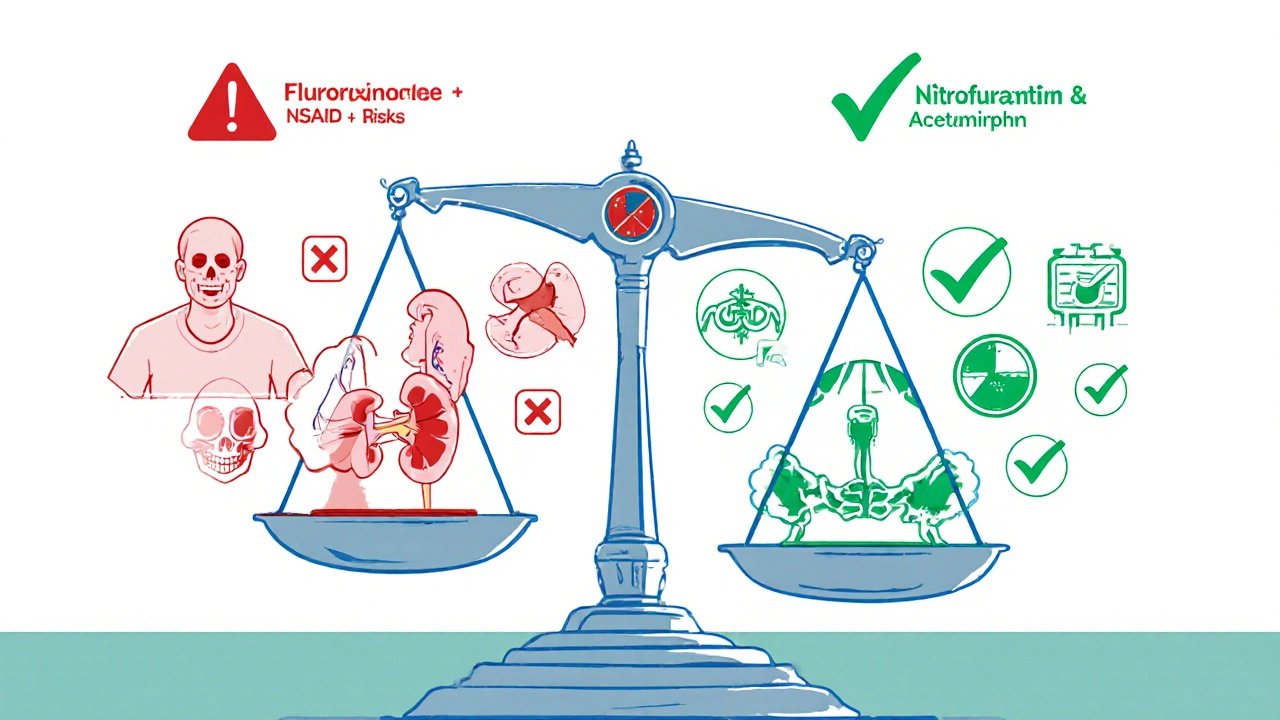
If you need an antibiotic and pain relief, here’s what works better:
- For UTIs: Use nitrofurantoin or fosfomycin instead of fluoroquinolones. They’re just as effective and don’t carry the same neurological or kidney risks.
- For respiratory infections: Amoxicillin-clavulanate is safer than levofloxacin for sinusitis or bronchitis.
- For pain: Switch from ibuprofen or naproxen to acetaminophen (paracetamol). It doesn’t affect kidney blood flow and doesn’t interact with fluoroquinolones.
- If you must take both: Only do so under close medical supervision. Your doctor should check your kidney function before and after. Avoid this combo if you’re over 60, have diabetes, high blood pressure, or already have kidney problems.
Many doctors still prescribe fluoroquinolones out of habit. But guidelines have changed. The 2021 Cannizzaro study suggested fluoroquinolones might cause a multisystem disorder called Fluoroquinolone-Associated Disability (FQAD), affecting not just nerves and kidneys, but also the gut, muscles, and mitochondria. That’s why the FDA is now updating labels to include warnings about mitochondrial toxicity - the underlying mechanism behind long-term damage.
The Bigger Picture: Why This Matters
Fluoroquinolone prescriptions in the U.S. dropped 22% between 2015 and 2022 - from 28.3 million to 22.1 million. That’s good news. But they’re still widely used, especially in countries like India and China, where 45% of global fluoroquinolone consumption happens.
The cost of these side effects isn’t just physical - it’s financial. A 2020 study estimated that fluoroquinolone-related adverse events cost the U.S. healthcare system $1.8 billion annually. Kidney problems accounted for 37% of those costs. Neurological complications made up another 29%.
These aren’t just rare side effects. They’re preventable. And too often, they’re overlooked because they don’t show up in the first few days. The damage builds quietly - until it’s too late.
Bottom Line: Don’t Mix These Drugs
If you’re prescribed a fluoroquinolone, ask: Is this really the best option? Are there safer alternatives? And if you’re on NSAIDs for pain, tell your doctor - because combining them with fluoroquinolones can lead to kidney failure, nerve damage, or brain fog that lasts for years.
There’s no magic pill that fixes the damage once it’s done. Prevention is the only real treatment. Don’t assume your doctor knows the risks. Ask questions. Push for safer options. Your kidneys and your brain will thank you.
Can fluoroquinolones cause permanent nerve damage?
Yes. Fluoroquinolones can cause peripheral neuropathy - damage to nerves outside the brain and spinal cord - that may become permanent. Symptoms include burning, tingling, numbness, or weakness in the hands and feet. Health Canada and the FDA both warn that these effects can be disabling and persist long after stopping the drug. In patient surveys, 32% of those affected reported lasting disability.
Is it safe to take ibuprofen with ciprofloxacin?
No, it’s not recommended. Combining ibuprofen with ciprofloxacin increases the risk of both kidney injury and neurological side effects like seizures or confusion. This is especially dangerous in older adults or those with existing kidney problems. Acetaminophen is a safer pain reliever to use with fluoroquinolones.
What are the signs of kidney damage from these drugs?
Signs include reduced urine output, swelling in the legs or ankles, fatigue, nausea, confusion, and sudden increases in creatinine levels detected by blood tests. If you’re taking fluoroquinolones and NSAIDs together and notice any of these symptoms, stop the medications and contact your doctor immediately.
Are there safer antibiotics than fluoroquinolones?
Yes. For urinary tract infections, nitrofurantoin or fosfomycin are preferred. For respiratory infections, amoxicillin-clavulanate or azithromycin are safer alternatives. Fluoroquinolones should only be used when other options have failed or aren’t suitable - and never as a first-line treatment for mild infections.
Why are fluoroquinolones still prescribed if they’re so dangerous?
They’re still used because they’re broad-spectrum and work quickly, especially for complicated infections. But regulatory agencies now restrict their use to cases with no other options. Many doctors still prescribe them out of habit or because patients expect a strong antibiotic. Patient awareness is growing, and prescriptions are declining - but the risk remains high for those who receive them.


Bart Capoen
October 29, 2025 AT 12:54Bob Martin
October 31, 2025 AT 03:24Sage Druce
October 31, 2025 AT 23:19Jen Taylor
November 1, 2025 AT 08:57Kevin Stone
November 3, 2025 AT 03:55Natalie Eippert
November 4, 2025 AT 09:53Tyler Mofield
November 5, 2025 AT 21:06kendall miles
November 6, 2025 AT 14:52Patrick Dwyer
November 6, 2025 AT 16:27luna dream
November 7, 2025 AT 18:16Linda Patterson
November 8, 2025 AT 21:37Gary Fitsimmons
November 9, 2025 AT 14:56